Introduction: The Evolving Landscape of Heart Disease Treatment
Heart disease remains a leading cause of mortality worldwide, necessitating continuous advancements in medical research and treatment approaches. While traditional interventions such as lifestyle changes, medications, and invasive procedures have long been the cornerstone of heart disease management, recent breakthroughs in cardiovascular treatment have paved the way for more effective, minimally invasive, and personalized therapeutic options. Understanding these advancements is crucial for both healthcare professionals and patients seeking the best possible care.
You may also like: Fatigue and Psoriatic Disease
The question, “how is heart disease diagnosed?” is central to effective treatment planning. Modern diagnostic techniques enable early detection, allowing timely interventions that can prevent disease progression. From non-invasive imaging technologies to cutting-edge genetic screenings, the ability to identify cardiac conditions early enhances treatment success rates. This article explores five modern treatments for heart disease, detailing how these innovations contribute to improved patient outcomes and shaping the future of cardiac care.
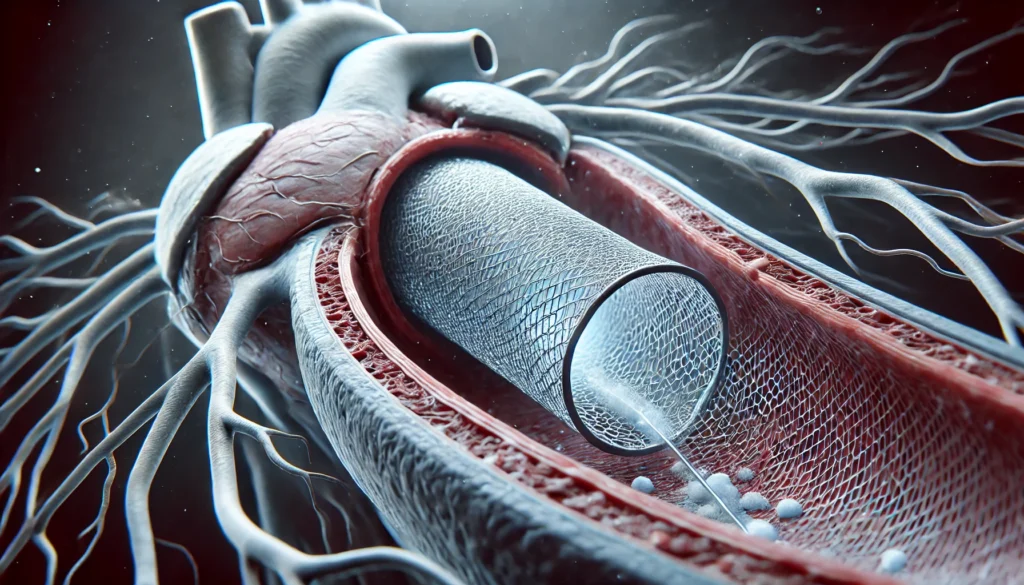
1. Transcatheter Aortic Valve Replacement (TAVR)
One of the most groundbreaking developments in heart disease treatment is Transcatheter Aortic Valve Replacement (TAVR). This minimally invasive procedure has revolutionized the management of aortic stenosis, a condition where the heart’s aortic valve narrows, restricting blood flow. Traditionally, open-heart surgery was the only option for replacing the damaged valve. However, TAVR provides an alternative that significantly reduces recovery time and risks associated with major surgery.
TAVR involves threading a catheter through a blood vessel, usually via the femoral artery, to deliver and implant a replacement valve within the existing, diseased valve. This procedure is particularly beneficial for patients who are at high risk for complications from open-heart surgery. Clinical studies have demonstrated that TAVR offers comparable, if not superior, survival rates to traditional surgery, particularly among elderly and high-risk patients.
Beyond its efficacy, TAVR highlights the importance of patient-specific treatments. The ability to tailor cardiovascular treatment based on individual risk profiles represents a shift toward personalized medicine in cardiology. As researchers refine the technique, expanding its indications to lower-risk patients, TAVR is poised to become a standard of care for aortic stenosis worldwide.
2. Gene and Stem Cell Therapy for Heart Disease
Gene and stem cell therapy represent some of the most promising frontiers in treating heart disease. These cutting-edge approaches focus on regenerating damaged heart tissue and improving cardiac function, offering hope to patients with severe heart failure or irreversible myocardial damage.
Gene therapy aims to modify or introduce genetic material to correct abnormalities in heart cells. Research has explored methods to stimulate the production of proteins that promote vascular growth and improve heart function. Early clinical trials suggest that targeted gene therapies could one day be used as a standard treatment for cardiovascular disease, particularly in patients with limited therapeutic options.
Similarly, stem cell therapy harnesses the body’s ability to repair itself. Stem cells, particularly mesenchymal stem cells and induced pluripotent stem cells, are injected into damaged heart tissue to encourage regeneration. While this therapy is still in experimental stages, clinical trials have shown encouraging results, with some patients experiencing improved heart function and reduced symptoms of heart failure.
Despite the promise, challenges remain, including ensuring the safe and controlled differentiation of stem cells and mitigating potential risks such as immune rejection. However, as research progresses, gene and stem cell therapies may become viable options for treating cardiovascular disease, offering a potential cure for heart disease at a molecular level.
3. Artificial Intelligence (AI) in Cardiac Diagnostics and Treatment
Artificial intelligence (AI) is transforming the way heart disease is diagnosed and managed. By leveraging machine learning algorithms, AI can analyze vast datasets, identify patterns, and predict outcomes with remarkable accuracy. AI-driven diagnostic tools assist cardiologists in making precise diagnoses, ultimately improving treatment efficacy and patient outcomes.
One of the key applications of AI in cardiac care is its role in imaging analysis. AI-powered systems can assess echocardiograms, CT scans, and MRIs with speed and accuracy, identifying early signs of heart disease that might be missed by the human eye. This enhances the reliability of heart problem diagnosis, ensuring timely intervention.
Beyond diagnostics, AI is being integrated into treatment planning. Predictive analytics help cardiologists determine which therapy for heart disease will yield the best outcomes for individual patients. AI models consider factors such as genetic predisposition, lifestyle, and pre-existing conditions to customize treatment plans. Additionally, wearable AI-enabled devices continuously monitor cardiac activity, alerting patients and healthcare providers to potential issues in real time.
As AI continues to evolve, its potential applications in cardiac treatment are expanding. From automating risk assessments to optimizing drug therapies, AI is becoming an indispensable tool in modern cardiology, improving the precision and efficiency of treating heart disease.
4. 3D Bioprinting of Cardiac Tissues and Organs
The advent of 3D bioprinting is revolutionizing the treatment of cardiovascular disease by enabling the fabrication of heart tissues and, potentially, whole organs. This technology uses bio-inks composed of living cells to create structures that mimic natural heart tissue, offering a novel approach to treating heart defects and end-stage heart failure.
One of the most exciting applications of 3D bioprinting is the development of bioengineered heart patches. These patches, created from patient-derived cells, can be implanted onto damaged heart tissue to promote regeneration and restore function. Unlike traditional grafts, these bioprinted tissues integrate seamlessly with existing cardiac structures, reducing the risk of immune rejection.
In the future, researchers aim to bioprint entire heart valves or even complete hearts, addressing the critical shortage of organ donors. While significant hurdles remain, including scalability and long-term viability, the potential for 3D bioprinting to transform cardiac disease treatment is immense.
5. Personalized Medicine and Pharmacogenomics in Cardiology
The field of pharmacogenomics—tailoring drug therapies based on an individual’s genetic makeup—is ushering in a new era of personalized medicine for heart disease treatment. Traditional one-size-fits-all approaches often result in varying responses to medications. However, pharmacogenomics enables clinicians to prescribe drugs with greater precision, reducing adverse reactions and enhancing efficacy.
By analyzing genetic markers, doctors can determine which cardiovascular treatment is most likely to be effective for a given patient. This approach is particularly beneficial for managing conditions such as hypertension, arrhythmias, and heart failure, where medication responses can vary widely. Additionally, advancements in lipid-lowering therapies, including PCSK9 inhibitors, demonstrate how targeted treatments can significantly reduce cardiovascular risk.
The integration of pharmacogenomics into routine clinical practice is still in its early stages, but its potential is vast. As genetic testing becomes more accessible and cost-effective, the ability to optimize heart problem treatment through personalized medicine will likely become a cornerstone of modern cardiology.
Frequently Asked Questions (FAQ) on Modern Treatments for Heart Disease
1. What are the latest advancements in treating cardiovascular disease? The latest advancements in treating cardiovascular disease include innovations in minimally invasive procedures, regenerative medicine, and artificial intelligence-driven diagnostics. Transcatheter aortic valve replacement (TAVR) has significantly improved outcomes for patients with severe aortic stenosis who cannot undergo open-heart surgery. Additionally, gene and stem cell therapy are emerging as potential solutions for regenerating damaged heart tissue, offering a long-term approach to cardiac disease treatment. AI-powered diagnostics now enhance the accuracy of heart problem diagnosis by analyzing imaging data with greater precision than traditional methods. These advancements collectively improve both the survival rate and quality of life for patients undergoing treatment for cardiovascular disease.
2. How is heart disease diagnosed with modern technology? The diagnosis of heart disease has evolved significantly with the advent of advanced imaging techniques and AI-driven tools. Traditional diagnostic methods such as echocardiograms, stress tests, and angiography are now complemented by AI-enhanced cardiac imaging, which can detect abnormalities earlier and with greater accuracy. Machine learning algorithms assist in analyzing large datasets, improving the speed and precision of detecting various heart condition names. Moreover, wearable technology plays a crucial role in monitoring real-time cardiovascular health, alerting individuals to irregular heart rhythms and other warning signs. This combination of technology-driven diagnostics enhances early intervention, making the treatment for cardiovascular disease more effective.
3. Is cardiovascular disease curable with modern treatments? While there is no absolute cure for heart disease, modern treatments have made it possible to manage and, in some cases, reverse certain conditions. Healthy heart treatments such as lifestyle modifications, targeted medications, and interventional procedures can significantly slow disease progression and prevent complications. Regenerative medicine, including stem cell therapy and gene therapy, is showing promise in repairing heart tissue and restoring function in patients with advanced disease. For many patients, the key to treating cardiovascular disease effectively lies in early detection and a comprehensive, personalized treatment plan. As research continues, future advancements may bring us closer to a cure for heart disease.
4. What are the benefits of personalized medicine in cardiac treatment? Personalized medicine in cardiac treatment focuses on tailoring therapies based on a patient’s genetic profile, lifestyle, and specific risk factors. Pharmacogenomics, the study of how genes influence drug response, allows doctors to prescribe the most effective medications with minimal side effects. This approach is particularly beneficial for conditions such as hypertension, heart failure, and arrhythmias, where standard treatments may not be equally effective for all patients. Additionally, AI-driven predictive analytics can help determine which treatment would most likely be used for cardiovascular disease in a given patient. Personalized medicine ensures that heart disease treatment is both efficient and patient-specific, optimizing outcomes.
5. Can artificial intelligence improve heart disease treatment? Artificial intelligence (AI) is transforming heart disease treatment by enhancing diagnostic accuracy, predicting patient outcomes, and optimizing treatment plans. AI-driven imaging analysis can detect signs of cardiovascular disease earlier than conventional methods, leading to timely intervention. Machine learning algorithms assess patient data to recommend personalized therapy for heart disease, reducing trial-and-error prescribing. Additionally, AI-powered wearable devices continuously monitor cardiac health, detecting irregularities and notifying healthcare providers in real time. As AI technology advances, its integration into cardiovascular treatment is expected to further improve precision, efficiency, and accessibility.
6. What role does 3D bioprinting play in treating heart defects? 3D bioprinting is an emerging technology with the potential to revolutionize treatments of heart defect conditions and advanced cardiac disease. Using bio-inks made from living cells, scientists can create heart tissues, patches, and even heart valves for transplantation. This innovation offers a potential solution for patients who require cardiac treatment but face organ donor shortages. Bioengineered tissues can integrate seamlessly into the heart, reducing the risk of rejection and improving long-term outcomes. As research progresses, 3D bioprinting could provide a groundbreaking cure for heart disease by enabling the creation of fully functional artificial hearts.
7. How can lifestyle modifications complement modern heart problem treatment? Lifestyle modifications remain an essential component of treating heart disease alongside advanced medical interventions. A heart-healthy diet, regular physical activity, and smoking cessation can significantly enhance the effectiveness of cardiac treatment. Stress management techniques, such as meditation and yoga, also play a role in improving cardiovascular health. When combined with cutting-edge treatments for CVD, these lifestyle adjustments help prevent disease progression and improve patient outcomes. Integrating both medical advancements and holistic approaches ensures a comprehensive treatment strategy for long-term heart health.
8. What are the current guidelines for coronary heart disease treatment? Coronary heart disease treatment guidelines emphasize a multi-faceted approach that includes medication, lifestyle changes, and procedural interventions when necessary. Medications such as statins, beta-blockers, and anticoagulants are commonly prescribed to manage risk factors and prevent complications. When medical therapy alone is insufficient, interventional procedures like angioplasty and stent placement are performed to restore blood flow. The latest coronary heart disease treatment guidelines also highlight the importance of personalized care, incorporating genetic testing to refine medication choices. As research progresses, new recommendations continue to emerge, ensuring that patients receive the most effective and up-to-date cardiovascular treatment.
9. How do wearable devices contribute to diagnosing and treating cardiovascular disease? Wearable devices have become a valuable tool in diagnosing and treating cardiovascular disease by providing continuous heart health monitoring. Smartwatches equipped with ECG functionality detect irregular heart rhythms, such as atrial fibrillation, allowing for early intervention. These devices also track heart rate variability, sleep patterns, and physical activity, all of which contribute to a more comprehensive heart problem diagnosis. For patients undergoing therapy for heart disease, wearable technology helps track progress and adherence to treatment regimens. By integrating these devices into cardiac care, physicians can offer more data-driven and personalized treatment plans.
10. What is the future of cardiovascular disease treatment? The future of cardiovascular disease treatment is promising, with ongoing advancements in regenerative medicine, AI-driven healthcare, and bioengineered solutions. Researchers are exploring how to cure cardiovascular disease through genetic editing techniques such as CRISPR, which could correct inherited cardiac conditions at the DNA level. AI is expected to further refine diagnostics, making heart problem treatment more precise and proactive. Additionally, advancements in nanotechnology may allow for targeted drug delivery systems, minimizing side effects and maximizing therapeutic benefits. With continuous innovation, the goal of making cardiovascular treatment more effective, less invasive, and potentially curative is within reach.

Conclusion: The Future of Cardiac Care
The rapid evolution of heart disease treatment highlights the importance of continuous research and innovation in the field of cardiology. From minimally invasive procedures like TAVR to groundbreaking advances in gene therapy, AI diagnostics, and 3D bioprinting, the landscape of cardiac care is transforming before our eyes. As these technologies progress, they offer new hope for patients and healthcare providers alike, addressing long-standing challenges in treating cardiovascular disease.
The ultimate goal of these advancements is not only to extend life but also to improve quality of life. While significant progress has been made, ongoing research and collaboration will be essential to refining these treatments and expanding their accessibility. The future of cardiovascular treatment is bright, promising a new era where heart disease may no longer be the leading cause of mortality but a manageable condition with highly effective solutions.
cardiovascular health advancements, innovative heart disease therapies, cutting-edge cardiac care, latest treatments for heart conditions, minimally invasive heart procedures, heart disease prevention strategies, modern cardiology breakthroughs, AI in cardiovascular medicine, regenerative medicine for heart health, emerging trends in heart treatment, personalized cardiology treatments, stem cell therapy for heart repair, heart valve replacement innovations, genetic research in cardiology, digital health in heart care, future of heart disease management, wearable technology for heart monitoring, precision medicine in cardiology, artificial intelligence in heart diagnostics, non-invasive heart treatments
Further Reading:
7 Types of Heart Diseases that Need Modern Treatment
5 advances in heart health that are saving lives
Everything you need to know about heart disease
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.