Understanding the Widowmaker Heart Attack
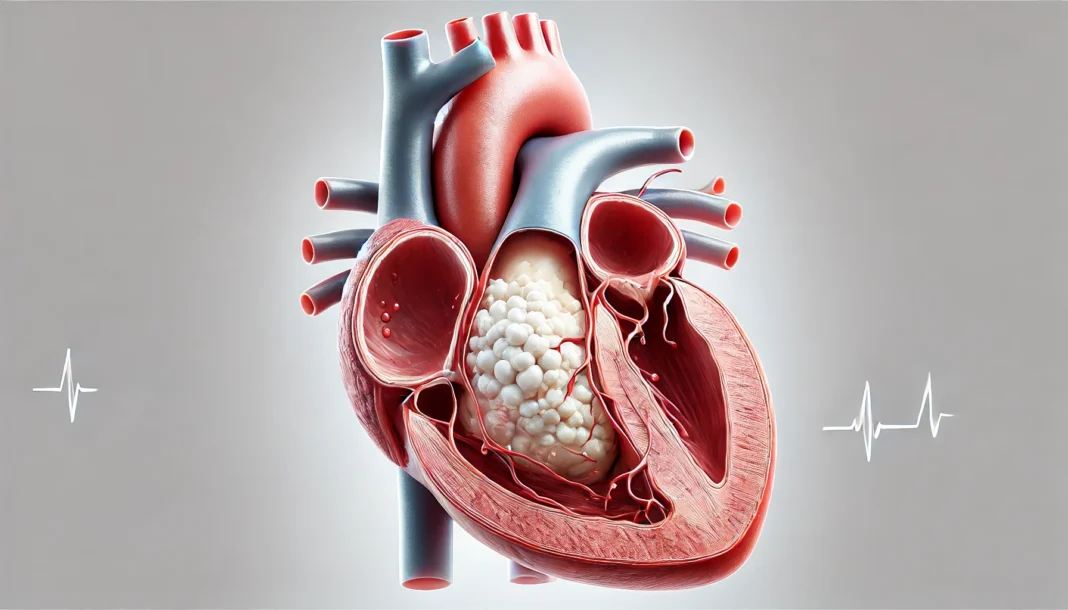
A widowmaker heart attack is one of the deadliest cardiovascular events, occurring when a severe blockage in the left anterior descending (LAD) artery significantly restricts blood flow to the heart. The term “widowmaker” reflects its high fatality rate if not treated immediately. As the LAD artery supplies a substantial portion of the heart muscle with oxygenated blood, any significant LAD artery blockage can result in catastrophic consequences.
You may also like: How to Naturally Clear Blocked Arteries and Improve Heart Health Without Surgery
This type of heart attack is especially dangerous because it can cause the heart to stop beating suddenly. Many individuals who suffer from a widowmaker heart attack experience little warning, making it imperative to understand the risk factors, early symptoms, and available life-saving treatment options. Knowing how to tell if arteries are clogged and recognizing the warning signs of an impending heart attack can be the difference between life and death.
The Role of the LAD Artery and Its Medical Significance
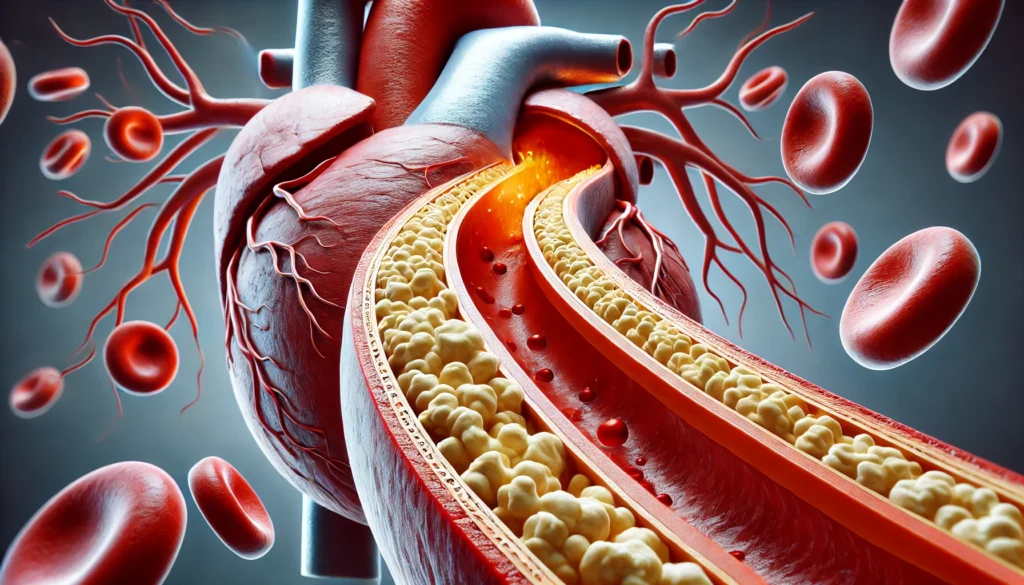
The LAD artery, medically abbreviated as “LAD,” is one of the major coronary arteries responsible for supplying blood to the front and left side of the heart. When this artery becomes blocked due to plaque buildup—a condition known as atherosclerosis—the heart muscle is deprived of oxygen, leading to the onset of a heart attack.
LAD artery involvement meaning a significant obstruction can lead to severe myocardial infarction, often resulting in extensive damage to the heart tissue. This is why it is critical to detect LAD blockage early and take preventative measures to ensure optimal cardiovascular health. Medical professionals often utilize imaging techniques to obtain a picture of the widow maker artery, helping to assess the severity of blockages and determine the most effective treatment plan.
Risk Factors That Increase the Likelihood of a Widowmaker Heart Attack
Several risk factors contribute to the likelihood of developing a widowmaker heart attack. These factors include both lifestyle choices and genetic predispositions. Some of the most common risk factors include:
- High Cholesterol Levels: Excess cholesterol can lead to the buildup of plaque within the arteries, increasing the risk of a widowmaker heart problem.
- Hypertension (High Blood Pressure): Elevated blood pressure can damage arterial walls, making them more susceptible to plaque accumulation.
- Diabetes: Uncontrolled blood sugar levels can contribute to the hardening and narrowing of the arteries.
- Obesity and Sedentary Lifestyle: A lack of physical activity and poor dietary choices can accelerate cardiovascular disease.
- Smoking: Tobacco use significantly increases the risk of arterial blockages, including those in the LAD artery.
- Genetics and Family History: A family history of cardiovascular disease increases an individual’s risk of suffering from a widowmaker heart attack.
- Chronic Stress and Poor Sleep: Persistent stress and inadequate sleep can negatively impact heart health, making individuals more vulnerable to heart attacks.
Understanding these risk factors and taking proactive measures—such as maintaining a heart-healthy diet, engaging in regular exercise, and monitoring blood pressure and cholesterol levels—can help reduce the likelihood of experiencing a widowmaker heart attack.

Symptoms of a Widowmaker Heart Attack
Recognizing the early symptoms of a widowmaker heart attack is crucial for seeking immediate medical attention. While some individuals experience sudden cardiac arrest without prior warning, others may exhibit several key symptoms leading up to the event. These symptoms include:
- Severe Chest Pain or Discomfort: Often described as a crushing or squeezing sensation in the center or left side of the chest, which may radiate to the jaw, neck, shoulders, or arms.
- Shortness of Breath: Difficulty breathing or feeling out of breath, even without physical exertion.
- Excessive Sweating: Unexplained cold sweats, which may be accompanied by dizziness or lightheadedness.
- Nausea and Vomiting: Gastrointestinal symptoms can sometimes be mistaken for indigestion or heartburn.
- Extreme Fatigue: Feeling unusually tired, weak, or experiencing a sense of impending doom.
- Pain in the Upper Body: Discomfort in the back, shoulders, or stomach that does not subside.
Understanding how to tell if arteries are clogged and being aware of these symptoms can prompt individuals to seek urgent medical intervention, significantly increasing their chances of survival.
How Medical Professionals Diagnose a Widowmaker Heart Attack
Accurate and timely diagnosis is essential for the successful treatment of a widowmaker heart attack. Medical professionals employ several diagnostic tools to determine whether an individual is experiencing an LAD artery blockage. Some of the most common diagnostic procedures include:
- Electrocardiogram (ECG): This test records the electrical activity of the heart and can reveal abnormalities indicative of a heart attack.
- Blood Tests: Measuring levels of cardiac enzymes, such as troponin, helps determine whether there has been damage to the heart muscle.
- Coronary Angiography: A specialized imaging technique that provides a detailed picture of the widow maker artery, allowing doctors to assess blockages.
- Stress Tests: Evaluating how the heart responds to physical exertion can help identify potential blood flow restrictions.
- CT Angiography: A non-invasive imaging test used to detect the presence and severity of artery blockages.
Timely diagnosis allows medical professionals to initiate appropriate treatment strategies to restore blood flow and minimize heart damage.
Life-Saving Treatment Options for a Widowmaker Heart Attack
Prompt treatment is essential for increasing the chances of survival following a widowmaker heart attack. Some of the most effective life-saving interventions include:
- Emergency Angioplasty and Stent Placement: During a coronary angioplasty, a small balloon is inserted into the blocked artery and inflated to restore blood flow. A stent may also be placed to keep the artery open.
- Coronary Artery Bypass Grafting (CABG): In cases where angioplasty is not feasible, a bypass procedure may be performed to create an alternative pathway for blood flow.
- Thrombolytic Therapy: Clot-busting medications are sometimes used to dissolve blood clots obstructing the artery.
- Medications: Blood-thinning drugs, beta-blockers, and statins may be prescribed to manage symptoms and prevent future heart attacks.
For many patients, long-term lifestyle modifications, such as dietary changes and regular physical activity, play a crucial role in preventing recurrent heart attacks.

Frequently Asked Questions (FAQ) About Widowmaker Heart Attacks
1. What makes a widowmaker heart attack different from other heart attacks?
A widowmaker heart attack is unique because it involves a critical blockage in the left anterior descending (LAD) artery, which supplies a significant portion of the heart with oxygen-rich blood. Unlike other types of heart attacks that may involve partial blockages or smaller arteries, a complete LAD blockage can cause the heart to stop suddenly. This makes it one of the deadliest types of cardiac events, as there is little time to seek medical intervention once symptoms arise. Without immediate treatment, the lack of blood flow can lead to extensive heart muscle damage or even sudden cardiac arrest. Understanding how to tell if arteries are clogged and being proactive about heart health can significantly reduce the risk of experiencing this life-threatening condition.
2. What are the early warning signs of a widowmaker heart attack?
While a widowmaker heart attack can strike suddenly, some people may experience warning signs in the days or weeks leading up to the event. Symptoms such as persistent chest discomfort, unusual fatigue, and shortness of breath should not be ignored. Some individuals may also notice dizziness, nausea, or pain radiating to the arms, neck, or jaw. These symptoms can be more subtle in women, often presenting as indigestion or back pain, making it more difficult to recognize a heart attack. Knowing how to tell if arteries are clogged early can provide an opportunity for preventative care before a widowmaker artery becomes fully obstructed.
3. Can lifestyle changes prevent a widowmaker heart attack?
Yes, making heart-healthy lifestyle choices can significantly reduce the risk of a widowmaker heart attack. Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help prevent LAD artery blockage by reducing cholesterol buildup. Regular exercise, particularly activities that promote cardiovascular endurance, helps maintain healthy blood circulation and prevents plaque accumulation in the arteries. Avoiding smoking and excessive alcohol consumption can also lower the chances of developing a widowmaker heart problem. Additionally, managing stress levels and ensuring adequate sleep contribute to overall heart health and reduce the likelihood of sudden cardiac events.
4. How do doctors diagnose a blocked widow maker artery?
Medical professionals use a combination of diagnostic tests to determine whether a widow maker artery is blocked. An electrocardiogram (ECG) is often the first test performed to detect abnormal heart rhythms that may indicate an obstruction. Blood tests measuring cardiac enzymes like troponin can reveal heart muscle damage. Coronary angiography, an advanced imaging technique, provides a detailed picture of the widow maker artery, allowing doctors to assess the severity of the blockage. In some cases, a CT angiogram may be used to non-invasively examine the arteries and determine if immediate intervention is needed. Recognizing how to tell if arteries are clogged through early testing can lead to life-saving treatments.
5. What does a blocked artery feel like, and is it always painful?
A blocked artery can cause various symptoms, and while severe chest pain is a classic sign, it is not always present. Some individuals may experience a heavy or squeezing sensation in the chest, while others report discomfort in their arms, shoulders, or jaw. Shortness of breath, dizziness, and cold sweats can also indicate a blockage, especially if these symptoms occur during physical exertion. Some people may mistake mild symptoms for heartburn or indigestion, delaying medical intervention. Understanding how to tell if arteries are clogged based on subtle warning signs can prevent a fatal heart attack.
6. Which artery is the worst to be blocked, and why?
The LAD artery is considered the worst artery to be blocked because it supplies blood to a large portion of the heart muscle. An LAD blockage restricts blood flow to the left ventricle, the heart’s primary pumping chamber, leading to a widowmaker heart attack. Since the LAD artery is critical for maintaining heart function, a blockage here often results in severe damage or even sudden death. Unlike blockages in smaller arteries, which may allow some collateral circulation to develop over time, an LAD blockage typically occurs abruptly, leaving little time for the heart to adapt. This makes immediate medical attention crucial for survival.
7. Can the widow maker artery be stented, and how effective is it?
Yes, the widow maker artery can be treated with a stent, a small mesh tube that helps keep the artery open and allows blood to flow freely. During an emergency angioplasty, a catheter is inserted into the blocked artery, and a balloon is inflated to clear the obstruction. Once the artery is widened, a stent is placed to prevent future blockages. Stenting is highly effective in restoring blood flow, and most patients experience significant improvement in heart function after the procedure. However, lifestyle modifications and medication are often necessary to prevent re-narrowing of the artery and to maintain long-term cardiovascular health.
8. Does it hurt when a blood vessel gets clogged, and how severe is the pain?
The pain associated with a clogged blood vessel varies from person to person. Some individuals describe it as a sharp, stabbing pain, while others feel a dull, squeezing pressure in the chest. Pain can also radiate to the arms, back, or neck, sometimes mimicking muscle strain or indigestion. In certain cases, especially in diabetics, a heart attack may occur with minimal or no pain at all, a condition known as a “silent” heart attack. Since symptoms are not always clear-cut, understanding how do you know if you have a blocked artery requires paying close attention to subtle changes in physical health and seeking medical evaluation when in doubt.
9. Can a widowmaker heart attack occur without prior symptoms?
Yes, a widowmaker heart attack can occur suddenly without warning, which is why it is considered one of the most dangerous cardiovascular events. In some cases, individuals may have underlying risk factors such as high cholesterol, hypertension, or diabetes but remain asymptomatic until the blockage reaches a critical level. This is why routine check-ups and heart screenings are crucial, especially for those with a family history of cardiovascular disease. Advanced imaging techniques, such as a coronary calcium scan, can help identify early signs of artery blockage before symptoms develop. Recognizing how do you know if your artery is blocked before it leads to a heart attack can save lives.
10. How can you tell if your arteries are blocked without experiencing a heart attack?
There are several ways to assess arterial health before a heart attack occurs. One of the earliest indicators of a blockage is reduced exercise tolerance—if you feel unusually fatigued, short of breath, or experience chest discomfort during physical activity, it may signal a circulatory problem. Medical tests such as a stress test, echocardiogram, or coronary angiogram can detect blockages before they become life-threatening. Paying attention to symptoms such as cold extremities, frequent dizziness, or unexplained high blood pressure can also provide clues about arterial health. Being proactive and learning how can you tell if your arteries are blocked through regular screenings and lifestyle modifications can significantly lower the risk of a widowmaker heart attack.
Conclusion: Taking Control of Your Heart Health
A widowmaker heart attack is a life-threatening medical emergency that requires immediate attention. By understanding the causes, symptoms, and treatment options, individuals can take proactive steps to safeguard their heart health. Recognizing early warning signs, seeking timely medical intervention, and making heart-healthy lifestyle choices are key to preventing cardiovascular complications. If you or a loved one experience symptoms suggestive of a heart attack, seeking emergency care without delay could be lifesaving.
heart attack prevention, cardiac health tips, coronary artery disease risk, signs of heart blockage, myocardial infarction symptoms, emergency heart care, heart disease awareness, cardiovascular wellness, heart attack recovery, blood circulation issues, healthy arteries guide, cholesterol and heart disease, heart stent procedure, cardiac rehabilitation tips, recognizing heart disease early, lifestyle changes for heart health, cardiac arrest survival, understanding heart function, plaque buildup in arteries, preventing arterial blockages
Further Reading:
Widowmaker Heart Attack: Causes, Signs, and Life-Saving Tips
A Doctor Explains What Makes a Heart Attack a ‘Widowmaker’
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.