Introduction: The Silent Threat of Vascular Calcification
Vascular calcification is a serious and often underestimated health concern that affects millions of people worldwide. It is a pathological condition characterized by the accumulation of calcium deposits within the blood vessels, particularly the arteries, leading to reduced elasticity, impaired blood flow, and increased cardiovascular risks. While calcification is often associated with aging, it is not merely a natural consequence of growing older. Instead, it is a complex process influenced by multiple factors, including metabolic disorders, chronic inflammation, and lifestyle choices. Understanding what causes calcium deposits in the vascular system, the distinctions between different types of calcification, and the potential health consequences is essential for preventing and managing this condition effectively.
You may also like: How to Naturally Clear Blocked Arteries and Improve Heart Health Without Surgery
The presence of vascular calcification has been strongly linked to cardiovascular diseases, particularly in individuals suffering from diabetes, chronic kidney disease, and atherosclerosis. This condition, often referred to as atherosclerotic calcification, can contribute to arterial stiffness, increased blood pressure, and a heightened risk of heart attack and stroke. Moreover, there is growing concern over the role of medical procedures in calcification development, leading to the question: Can cauterization cause calcification? Exploring the connection between medical interventions and vascular calcification is critical for both healthcare professionals and patients alike.
In this comprehensive article, we will explore the biological mechanisms behind vascular calcification, differentiate between various forms of calcium buildup, examine its risk factors, and discuss potential prevention and treatment strategies. Additionally, we will address common misconceptions, such as the cauterize vs calcification debate, and provide insights into how medical advancements may help mitigate the risks associated with this condition. By understanding what is calcification and what is calcified, individuals can take proactive steps toward maintaining vascular health and reducing their susceptibility to cardiovascular complications.
The Biological Mechanisms of Vascular Calcification
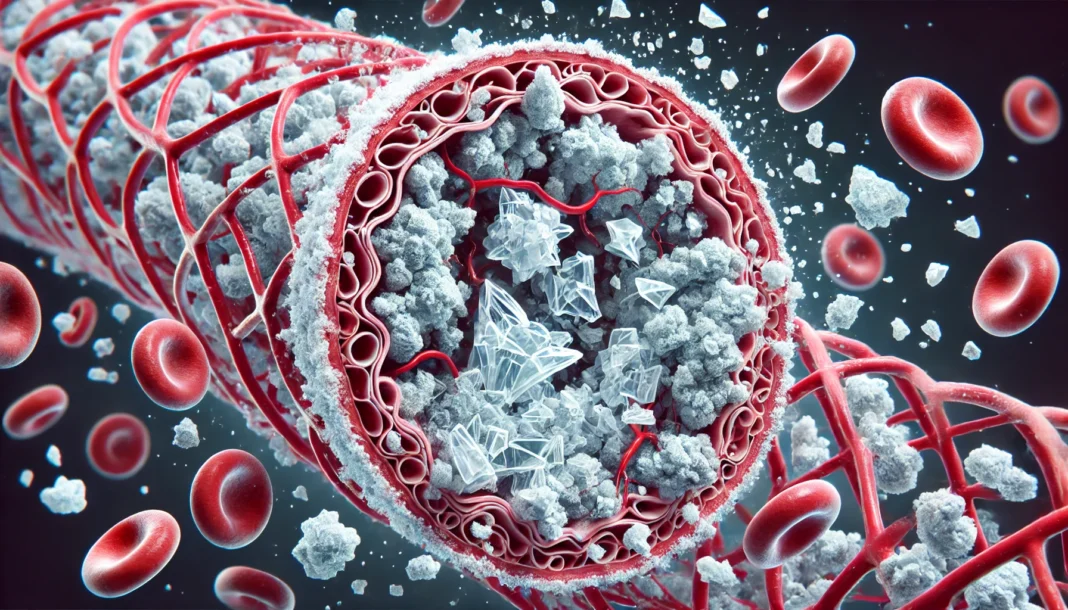
Vascular calcification is a highly regulated process that resembles bone formation, involving multiple cellular and molecular mechanisms. The deposition of calcium salts, particularly calcium phosphate, occurs within the arterial walls, leading to a progressive loss of vascular compliance. This process is mediated by vascular smooth muscle cells (VSMCs), endothelial cells, and inflammatory mediators that contribute to the pathological remodeling of the arterial walls.
One of the primary drivers of vascular calcification is the dysregulation of mineral metabolism. In conditions such as chronic kidney disease (CKD), the imbalance of phosphate and calcium homeostasis accelerates arterial calcification. Elevated phosphate levels induce the transformation of VSMCs into osteoblast-like cells, which then begin to deposit calcium within the arteries. This transformation mimics the bone mineralization process, underscoring the complexity of calcium buildup in the vascular system.
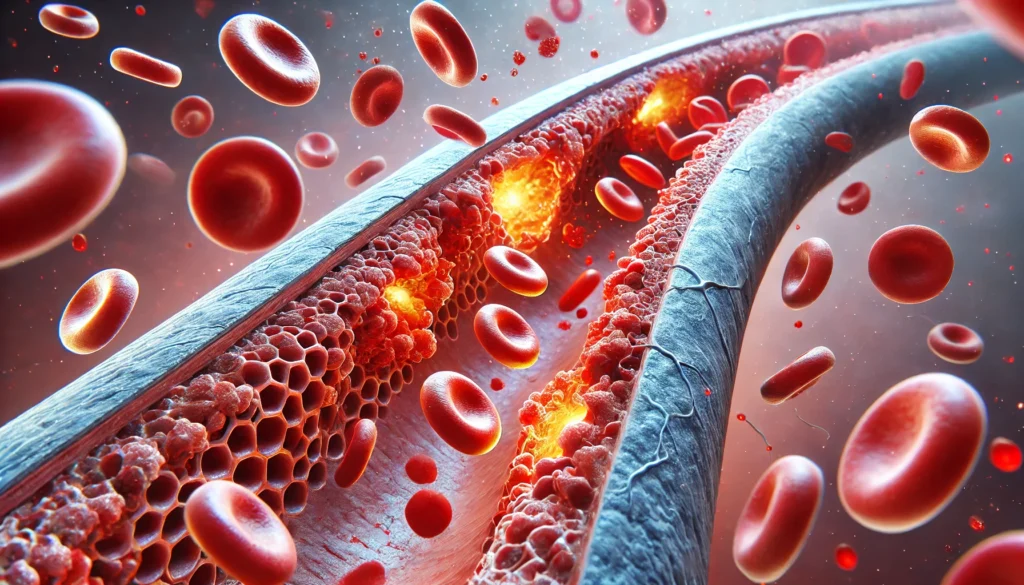
Another crucial factor is the role of inflammation in the calcification process. Inflammatory cytokines, oxidative stress, and immune system dysfunction can enhance the expression of calcification-promoting proteins while suppressing natural inhibitors of calcification. For instance, the downregulation of matrix Gla-protein (MGP) and fetuin-A, both of which are known inhibitors of calcification, allows calcium deposits to accumulate unchecked within the arterial walls.
Additionally, genetic predisposition plays a significant role in the susceptibility to vascular calcification. Variants in genes regulating bone metabolism, lipid metabolism, and vascular integrity can predispose individuals to excessive arterial calcium accumulation. As research continues to uncover the intricate pathways governing vascular calcification, new therapeutic targets may emerge to prevent and reverse this condition.

Risk Factors and Health Consequences of Vascular Calcification
The development of vascular calcification is influenced by a combination of genetic, metabolic, and environmental factors. While aging remains a significant contributor, other risk factors accelerate the process and increase its severity.
- Chronic Kidney Disease and Mineral Imbalance Patients with CKD are particularly prone to vascular calcification due to disruptions in calcium and phosphate metabolism. As kidney function declines, phosphate retention leads to secondary hyperparathyroidism, which further exacerbates calcium deposition in blood vessels.
- Diabetes and Insulin Resistance Individuals with diabetes are at heightened risk for atherosclerosis calcification due to chronic hyperglycemia and systemic inflammation. High blood sugar levels damage endothelial cells, leading to increased oxidative stress and enhanced vascular calcification.
- Hypertension and Atherosclerosis Persistent high blood pressure accelerates arterial damage, promoting calcium deposits in the arterial walls. The interplay between hypertension and atherosclerosis further compounds the risk of calcified atherosclerosis.
- Smoking and Poor Lifestyle Choices Smoking is a major contributor to vascular damage, as it induces oxidative stress and inflammation. Additionally, a sedentary lifestyle and poor dietary habits, particularly excessive intake of processed foods high in phosphates, contribute to calcium buildup in the arteries.
- Genetic and Epigenetic Factors Certain individuals inherit a genetic predisposition to vascular calcification, with familial hypercholesterolemia being one of the well-documented conditions linked to increased arterial calcium accumulation.
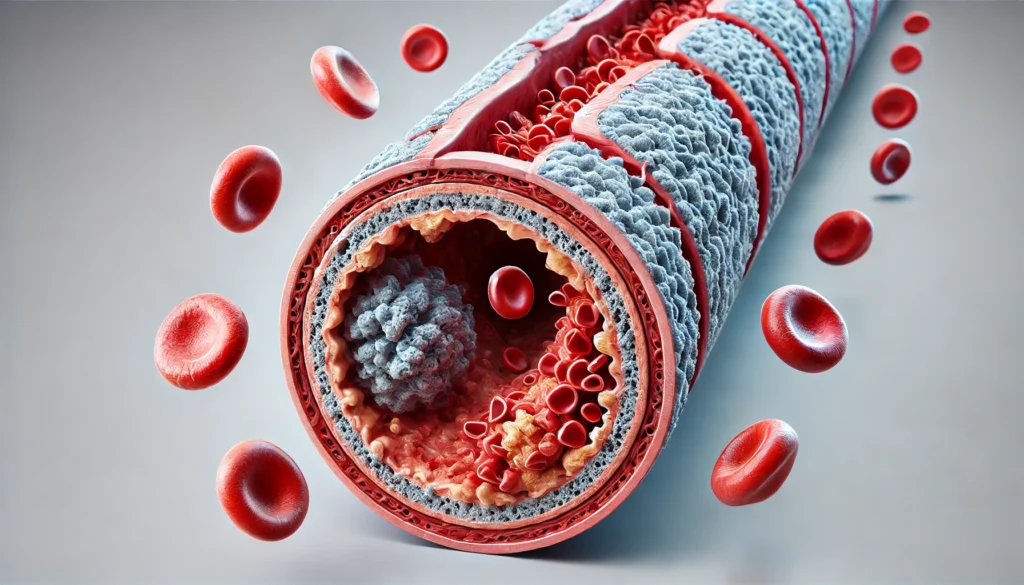
The consequences of vascular calcification are severe, ranging from reduced arterial flexibility to life-threatening cardiovascular events. The calcification of coronary arteries can lead to ischemic heart disease, while calcification in peripheral arteries contributes to conditions such as peripheral arterial disease (PAD), increasing the risk of limb amputation. Additionally, the calcification of heart valves, particularly the aortic valve, can result in aortic stenosis, necessitating surgical intervention.
Prevention and Treatment Strategies for Vascular Calcification
Given the significant health risks associated with vascular calcification, preventive and therapeutic approaches are crucial for maintaining cardiovascular health. While complete reversal of calcification remains challenging, several strategies can mitigate its progression and potential complications.
- Dietary and Lifestyle Modifications A diet rich in fruits, vegetables, and whole foods while minimizing processed foods and phosphate additives can help regulate mineral metabolism. Reducing sodium and sugar intake further supports vascular health by decreasing inflammation and oxidative stress.
- Pharmacological Interventions Medications such as phosphate binders, statins, and vitamin K2 supplements have shown promise in slowing down vascular calcification. Statins, in particular, help reduce inflammation and plaque buildup, indirectly lowering the risk of arterial calcium deposition.
- Medical Procedures and Their Implications Medical interventions, including surgical cauterization, have raised concerns about their potential role in promoting calcification. This has led to the question: Can cauterization cause calcification? While direct causation remains under investigation, certain medical procedures may contribute to vascular remodeling that predisposes patients to calcification over time.
- Emerging Therapies and Future Directions Advances in biotechnology, including gene therapy and regenerative medicine, offer potential avenues for reversing vascular calcification. Experimental approaches targeting osteogenic pathways within the vasculature may yield promising results in future clinical applications.
Frequently Asked Questions About Vascular Calcification
1. What distinguishes vascular calcification from other types of calcium deposits in the body?
Vascular calcification refers specifically to the accumulation of calcium deposits within blood vessels, particularly in the arteries, leading to reduced elasticity and increased cardiovascular risk. Unlike kidney stones or dental plaque, which also result from calcium buildup, vascular calcification involves complex biological pathways, often mimicking bone formation within the arterial walls. The distinction is crucial because while some calcium deposits in other tissues may be relatively harmless, atherosclerosis calcification contributes directly to heart disease, stroke, and high blood pressure. Factors such as chronic inflammation, metabolic imbalances, and genetic predisposition play a significant role in determining whether and where calcium buildup occurs. Understanding the differences between vascular calcification and other calcium-related conditions allows for targeted treatment strategies that address the specific risks associated with calcified atherosclerosis.
2. How does vascular calcification affect overall cardiovascular health?
Vascular calcification severely impacts cardiovascular function by stiffening the arteries and restricting blood flow, making the heart work harder to pump blood. This increased workload can lead to hypertension, left ventricular hypertrophy, and a higher likelihood of heart failure. Additionally, vascular calcification is a key contributor to ischemic events, such as heart attacks and strokes, as it often coincides with atherosclerosis calcification, which narrows the arteries and limits oxygen delivery to vital organs. The severity of cardiovascular complications depends on the extent and location of the calcium deposits, with coronary artery calcification posing one of the highest risks. Medical imaging techniques like CT scans and ultrasounds are often used to detect calcium buildup early, enabling timely interventions to mitigate cardiovascular damage.
3. What causes calcium deposits to form in blood vessels?
Calcium deposits in the vascular system are primarily triggered by disruptions in mineral metabolism, chronic inflammation, and endothelial damage. Conditions such as chronic kidney disease, diabetes, and high cholesterol can accelerate calcium buildup by altering the regulation of calcium and phosphate in the bloodstream. Additionally, prolonged exposure to oxidative stress and inflammatory cytokines promotes the transformation of vascular smooth muscle cells into osteoblast-like cells, which actively deposit calcium within the arteries. Dietary habits, including excessive phosphate intake from processed foods, may also contribute to the development of vascular calcification. Genetic predisposition plays a role as well, with certain individuals more likely to experience calcified atherosclerosis due to inherited metabolic disorders.
4. Can medical procedures like cauterization contribute to vascular calcification?
The relationship between medical procedures and vascular calcification is an area of ongoing research, particularly regarding whether cauterization can cause calcification. While direct causation has not been definitively established, some studies suggest that cauterization, which involves using heat to seal blood vessels, may induce local tissue changes that promote calcium buildup. The thermal injury from cauterization can trigger inflammatory responses and fibrosis, which, in some cases, may lead to vascular remodeling and calcification over time. Additionally, repeated medical interventions in the same area, such as those required for chronic conditions, may increase the likelihood of vascular complications. However, the benefits of cauterization often outweigh potential risks, particularly in life-threatening situations where controlling bleeding is essential.
5. How does atherosclerotic calcification differ from other forms of vascular calcification?
Atherosclerotic calcification specifically refers to calcium deposits that form within atherosclerotic plaques, which are fatty deposits lining the arteries. Unlike medial calcification, which affects the middle layer of the arterial wall and is more common in conditions like chronic kidney disease, atherosclerosis calcification directly contributes to plaque instability and cardiovascular events. The rupture of a calcified plaque can lead to the formation of a blood clot, which may result in heart attacks or strokes. Understanding these distinctions is crucial for developing effective treatment strategies, as therapies targeting atherosclerotic calcification often differ from those used to manage other types of vascular calcification. Advanced imaging techniques, such as coronary calcium scoring, can help assess the extent of arterial calcification and predict cardiovascular risk more accurately.
6. Are there lifestyle changes that can help prevent or slow down vascular calcification?
Yes, several lifestyle modifications can significantly reduce the risk of vascular calcification or slow its progression. Maintaining a heart-healthy diet rich in leafy greens, whole grains, and lean proteins while minimizing processed foods high in phosphates and trans fats can help regulate calcium metabolism. Regular exercise improves vascular flexibility and reduces systemic inflammation, both of which play key roles in preventing calcified atherosclerosis. Avoiding smoking and excessive alcohol consumption further supports arterial health by reducing oxidative stress and endothelial damage. Additionally, managing underlying health conditions, such as diabetes and hypertension, is crucial in preventing excessive calcium buildup in the arteries. While lifestyle changes alone may not reverse established vascular calcification, they are essential in minimizing further progression and associated complications.
7. What role does vitamin K2 play in preventing vascular calcification?
Vitamin K2 has gained attention for its potential role in inhibiting vascular calcification by activating proteins that regulate calcium deposition. Specifically, vitamin K2 activates matrix Gla-protein (MGP), which helps prevent calcium deposits from accumulating in the arteries. Studies suggest that individuals with lower vitamin K2 levels are more prone to vascular calcification, making dietary sources or supplementation a possible strategy for maintaining vascular health. Fermented foods, such as natto, and certain dairy products are excellent sources of vitamin K2. While research on vitamin K2 supplementation is still ongoing, early findings indicate that it may be a promising adjunct in preventing or slowing atherosclerosis calcification.
8. Can vascular calcification be reversed, or is it permanent?
While complete reversal of vascular calcification remains challenging, some treatments can slow its progression or reduce its impact on cardiovascular health. Certain medications, such as phosphate binders and statins, have been studied for their ability to manage calcium buildup in high-risk individuals. Emerging research suggests that targeting specific pathways involved in vascular calcification, such as the inhibition of osteogenic signaling in vascular cells, may hold promise for future treatments. Lifestyle interventions, including dietary modifications and regular physical activity, play a critical role in preventing further calcification. Advanced medical approaches, such as experimental gene therapies, are being explored to address calcified atherosclerosis at a cellular level, offering hope for more effective treatments in the future.
9. How does chronic kidney disease contribute to vascular calcification?
Chronic kidney disease (CKD) significantly increases the risk of vascular calcification due to impaired mineral metabolism. The kidneys regulate calcium and phosphate balance, but when kidney function declines, phosphate levels can rise, promoting calcium-phosphate deposition in the arteries. Secondary hyperparathyroidism, a common complication of CKD, further exacerbates calcium buildup by altering bone metabolism and increasing vascular osteogenesis. Many CKD patients experience medial vascular calcification, which differs from atherosclerotic calcification but still contributes to arterial stiffness and cardiovascular complications. Managing phosphate levels through diet, medications, and dialysis can help reduce the risk of excessive vascular calcification in CKD patients.
10. Is there ongoing research on new treatments for vascular calcification?
Yes, ongoing research is focused on developing innovative treatments to prevent and manage vascular calcification more effectively. Scientists are investigating gene therapy approaches aimed at modifying the expression of calcification-related proteins to slow down or reverse arterial calcium buildup. Additionally, new pharmaceutical agents targeting specific inflammatory pathways involved in vascular calcification are undergoing clinical trials. Biomarker research is also advancing, with efforts to identify early indicators of vascular calcification for more precise risk assessment. As medical technology progresses, novel treatments may emerge that offer more targeted and effective ways to combat calcified atherosclerosis and its associated health risks.
Conclusion: A Proactive Approach to Vascular Health
Vascular calcification is a complex and multifaceted condition that demands a proactive approach for prevention and management. By understanding what causes calcium deposits and the biological mechanisms underlying atherosclerotic calcification, individuals and healthcare professionals can take informed steps to mitigate its risks. Lifestyle interventions, pharmacological strategies, and emerging medical treatments all play a role in addressing this condition. With continued research and medical advancements, the hope remains that new solutions will emerge to combat vascular calcification effectively, improving cardiovascular health outcomes worldwide.
arterial calcification, heart disease risk factors, calcium metabolism disorders, chronic kidney disease complications, cardiovascular plaque buildup, artery hardening prevention, endothelial dysfunction, blood vessel health, vascular inflammation, lifestyle changes for heart health, managing high blood pressure, diabetes and heart disease, dietary impact on arteries, oxidative stress in blood vessels, anti-inflammatory nutrition, coronary artery disease prevention, role of vitamin K2 in heart health, advanced heart imaging techniques, emerging cardiovascular treatments, genetic factors in vascular health
Further Reading:
Peripheral arterial calcification: Prevalence, mechanism, detection, and clinical implications
Dietary antioxidants and vascular calcification: From pharmacological mechanisms to challenges
Medial vascular calcification revisited: review and perspectives
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.