Atherosclerotic heart disease of the native coronary artery without angina pectoris is a condition that presents a significant challenge in cardiovascular medicine. Unlike more commonly recognized forms of coronary artery disease (CAD) that manifest with chest pain or discomfort, this condition often progresses silently, making early detection and management crucial. The presence of mild soft plaque within the coronary arteries can contribute to this disease, potentially leading to severe cardiovascular complications if left unaddressed.
You may also like: How to Naturally Clear Blocked Arteries and Improve Heart Health Without Surgery
The Pathophysiology of Atherosclerotic Heart Disease
Atherosclerosis is a chronic, progressive condition characterized by the accumulation of lipids, inflammatory cells, and fibrous elements within the arterial walls. This process begins with endothelial dysfunction, which can result from various risk factors, including hypertension, hyperlipidemia, smoking, and diabetes mellitus. Once the endothelium is compromised, low-density lipoprotein (LDL) cholesterol infiltrates the arterial wall, becoming oxidized and triggering an inflammatory response.
Macrophages attempt to clear the oxidized LDL by engulfing it, forming foam cells. Over time, these foam cells accumulate, contributing to the formation of atherosclerotic plaques. In cases where mild soft plaque is present, the arterial lumen remains relatively open, allowing blood flow to continue without inducing symptoms like angina pectoris. However, this does not imply an absence of risk, as these plaques can rupture, leading to thrombosis and acute coronary syndromes.
Risk Factors and Contributing Conditions
Atherosclerotic heart disease of the native coronary artery without angina pectoris is influenced by a combination of genetic predisposition and modifiable risk factors. Age, family history of cardiovascular disease, and genetic lipid disorders play significant roles in disease development. However, lifestyle factors remain primary contributors to disease progression.
Uncontrolled hypertension exerts excessive pressure on the arterial walls, exacerbating endothelial injury and accelerating plaque formation. Similarly, dyslipidemia, particularly elevated levels of LDL cholesterol and low levels of high-density lipoprotein (HDL) cholesterol, enhances atherogenesis. Smoking introduces oxidative stress and inflammation, further impairing endothelial function.
Diabetes mellitus is another critical factor, as chronic hyperglycemia promotes glycation of proteins, endothelial dysfunction, and increased oxidative stress. Obesity, particularly visceral adiposity, contributes to systemic inflammation and insulin resistance, compounding cardiovascular risk. A sedentary lifestyle further exacerbates these risk factors by impairing lipid metabolism and promoting arterial stiffness.

Clinical Implications and Challenges in Diagnosis
One of the primary challenges in managing this condition is the absence of overt symptoms. Patients without angina pectoris may not seek medical evaluation until significant disease progression has occurred. This underscores the importance of screening and early detection, particularly in high-risk populations.
Diagnostic modalities include coronary artery calcium (CAC) scoring, which provides an assessment of calcified plaques, and computed tomography angiography (CTA), which offers detailed visualization of coronary anatomy. Carotid intima-media thickness (CIMT) measurement is another non-invasive method used to evaluate subclinical atherosclerosis.
Invasive coronary angiography remains the gold standard for definitive assessment, although it is typically reserved for cases where intervention is being considered. Blood biomarkers, including high-sensitivity C-reactive protein (hs-CRP) and lipoprotein(a), can provide additional risk stratification, guiding preventive strategies.
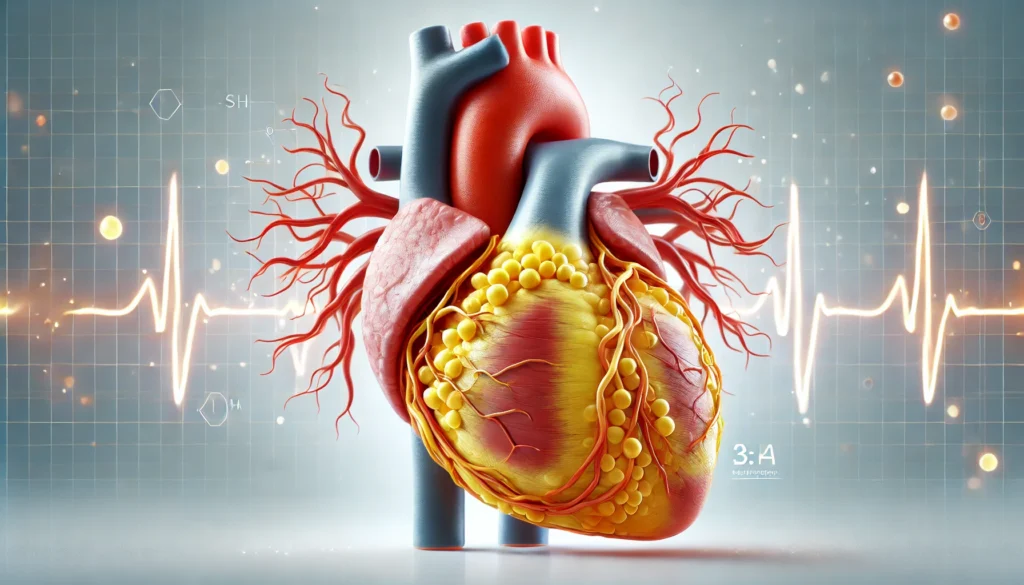
The Role of Mild Soft Plaque in Disease Progression
Mild soft plaque, though less obstructive than calcified or fibrous plaques, carries its own set of risks. These plaques are more prone to rupture due to their lipid-rich core and thin fibrous cap. When rupture occurs, it can precipitate platelet aggregation and thrombus formation, leading to myocardial infarction or sudden cardiac death.
Because these plaques do not always cause luminal narrowing significant enough to induce ischemia, traditional stress testing may not detect them. This makes imaging techniques such as CTA and intravascular ultrasound (IVUS) valuable tools in identifying vulnerable plaque features.
Strategies for Risk Reduction and Management
Management of atherosclerotic heart disease without angina pectoris involves a multifaceted approach aimed at reducing cardiovascular risk and preventing disease progression.
1. Lifestyle Modifications: Adopting a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins is fundamental. The Mediterranean diet, which emphasizes healthy fats from sources like olive oil and nuts, has been shown to improve lipid profiles and reduce inflammation. Regular physical activity, including aerobic and resistance training, enhances endothelial function, promotes weight management, and lowers blood pressure.
2. Pharmacological Interventions: Lipid-lowering therapy with statins remains a cornerstone of treatment. Statins not only reduce LDL cholesterol levels but also possess pleiotropic effects, including anti-inflammatory and plaque-stabilizing properties. For patients with statin intolerance or persistent dyslipidemia, alternative agents such as ezetimibe or proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors may be considered.
Antihypertensive medications, including angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs), provide vascular protection beyond blood pressure control. Antiplatelet therapy with aspirin or P2Y12 inhibitors may be indicated in select high-risk patients to reduce thrombotic events.
3. Regular Monitoring and Follow-Up: Given the silent nature of this condition, routine monitoring is essential. Periodic lipid panels, blood pressure assessments, and glucose monitoring aid in tracking risk factor modification. Advanced imaging at regular intervals may be warranted in patients with progressive disease markers.
4. Emerging Therapeutic Approaches: Novel therapies targeting inflammation, such as interleukin-1 beta inhibitors, show promise in reducing residual cardiovascular risk. Additionally, research into RNA-based therapies offers potential avenues for precision medicine in lipid management.
Frequently Asked Questions (FAQ) on Atherosclerotic Heart Disease of Native Coronary Artery Without Angina Pectoris
1. Can atherosclerotic heart disease of the native coronary artery without angina pectoris be detected through routine check-ups?
Yes, but detecting atherosclerotic heart disease of the native coronary artery without angina pectoris through routine check-ups requires a proactive approach. Standard physical exams and basic blood tests may not reveal the presence of mild soft plaque unless more specific diagnostic tools are employed. Advanced imaging techniques such as coronary artery calcium (CAC) scoring, computed tomography angiography (CTA), and carotid intima-media thickness (CIMT) measurement are often necessary to identify early-stage atherosclerosis. Additionally, blood markers like high-sensitivity C-reactive protein (hs-CRP) and lipoprotein(a) can offer insights into an individual’s cardiovascular risk. If a patient has multiple risk factors, their physician may recommend periodic screening to detect subtle yet significant changes in coronary artery health.
2. How does mild soft plaque differ from calcified plaque in coronary arteries?
Mild soft plaque differs from calcified plaque primarily in its composition and behavior within the coronary arteries. While calcified plaque contains hardened deposits of calcium, making it more stable and less likely to rupture, mild soft plaque is lipid-rich and more vulnerable to sudden rupture. This instability poses a significant risk for thrombus formation, which can lead to acute coronary events even in the absence of severe artery narrowing. Unlike calcified plaque, which is easily detectable through CAC scoring, mild soft plaque often requires more advanced imaging techniques such as intravascular ultrasound (IVUS) or optical coherence tomography (OCT) to be accurately assessed. Because of its potential to contribute to silent atherosclerosis, early identification and management of mild soft plaque are crucial for long-term cardiovascular health.
3. What lifestyle modifications can slow the progression of atherosclerosis in patients without angina pectoris?
Slowing the progression of atherosclerosis in patients without angina pectoris involves several lifestyle interventions tailored to reduce cardiovascular risk. A heart-healthy diet rich in fiber, lean proteins, and healthy fats, such as those found in the Mediterranean diet, can help lower LDL cholesterol and reduce inflammation. Regular physical activity, including both aerobic exercises and resistance training, has been shown to improve endothelial function and support arterial health. Stress management is also crucial, as chronic stress can lead to increased cortisol levels and exacerbate inflammation within the arteries. Additionally, quitting smoking and moderating alcohol intake can significantly reduce the burden on the cardiovascular system. Patients should work closely with healthcare providers to implement these changes effectively and sustain long-term cardiovascular health.
4. Can mild soft plaque be reversed or eliminated from the arteries?
While complete elimination of mild soft plaque is unlikely, its progression can be halted or even regressed with aggressive lifestyle modifications and pharmacological interventions. Statins, for example, not only lower LDL cholesterol but also have anti-inflammatory properties that can stabilize plaque and reduce the risk of rupture. Newer treatments, such as PCSK9 inhibitors and anti-inflammatory agents like interleukin-1 beta inhibitors, are showing promise in further reducing plaque burden. Regular exercise, weight management, and dietary adjustments play a crucial role in slowing plaque accumulation. Though mild soft plaque may not entirely disappear, these interventions can significantly lower the risk of future cardiovascular complications and enhance overall vascular health.
5. How does diabetes impact atherosclerotic heart disease of the native coronary artery without angina pectoris?
Diabetes is a major risk factor for atherosclerotic heart disease of the native coronary artery without angina pectoris because it accelerates vascular damage through multiple mechanisms. Chronically elevated blood glucose levels promote endothelial dysfunction, oxidative stress, and increased inflammation, all of which contribute to plaque development. Diabetics often have higher levels of small, dense LDL particles, which are more atherogenic and prone to oxidation. Additionally, diabetes can lead to autonomic dysfunction, reducing the perception of ischemic symptoms such as angina, making silent atherosclerosis even more dangerous. Proper blood sugar control through medication, dietary management, and regular monitoring is essential in preventing and managing the progression of atherosclerotic disease in diabetic patients.
6. Why do some people with atherosclerosis not experience angina or other symptoms?
Many individuals with atherosclerotic heart disease of the native coronary artery without angina pectoris remain asymptomatic due to the gradual nature of plaque accumulation and the development of collateral circulation. The body sometimes compensates for narrowed arteries by forming new blood vessels to bypass blockages, reducing the likelihood of noticeable ischemia. Additionally, mild soft plaque may not always cause significant luminal obstruction, meaning that blood flow remains adequate under normal conditions. However, these patients are still at risk for plaque rupture, which can lead to sudden cardiovascular events without prior warning. Regular cardiovascular evaluations are essential to monitor disease progression in asymptomatic individuals.
7. How does hypertension contribute to the development of mild soft plaque?
Hypertension is a significant contributor to the formation and progression of mild soft plaque due to its damaging effects on the arterial walls. Elevated blood pressure exerts excessive mechanical stress on the endothelium, leading to microtears and increased permeability to lipoproteins such as LDL cholesterol. Over time, this process encourages the infiltration of inflammatory cells and the buildup of lipid-rich plaque. Hypertension also promotes arterial stiffness and impairs the ability of blood vessels to dilate properly, further exacerbating cardiovascular risk. Effective blood pressure management through lifestyle modifications and medication therapy is essential in preventing plaque progression and reducing the likelihood of adverse cardiovascular events.
8. What role does inflammation play in the progression of atherosclerosis?
Inflammation is a central driver of atherosclerosis and significantly influences the stability of mild soft plaque. When the endothelium is damaged, the body initiates an immune response that involves white blood cells, cytokines, and inflammatory mediators. This response contributes to the formation of foam cells, which aggregate within arterial walls and further propagate inflammation. Chronic inflammation weakens the fibrous cap of plaques, increasing the risk of rupture and thrombus formation. Anti-inflammatory treatments, such as statins and targeted biologic therapies, aim to reduce systemic inflammation and stabilize vulnerable plaques. Lifestyle factors, including stress reduction and an anti-inflammatory diet, also play a critical role in mitigating inflammation-driven plaque progression.
9. What are the latest advancements in detecting and managing atherosclerotic heart disease without angina?
Recent advancements in detecting and managing atherosclerotic heart disease of the native coronary artery without angina pectoris have focused on precision medicine and improved imaging technologies. Artificial intelligence (AI) and machine learning are being used to analyze imaging data and detect early signs of plaque vulnerability. Novel lipid-lowering agents, such as bempedoic acid and inclisiran, provide additional options for patients with statin intolerance. Additionally, research into anti-inflammatory therapies targeting interleukin pathways is expanding the scope of cardiovascular risk reduction. Emerging non-invasive tests, such as blood-based biomarkers for endothelial function, may soon allow for earlier and more personalized cardiovascular risk assessments. As research progresses, these advancements will enhance early detection and improve long-term cardiovascular outcomes.
10. How should individuals with mild soft plaque adjust their long-term health strategy?
Individuals with mild soft plaque should adopt a comprehensive, long-term strategy focused on prevention and cardiovascular risk reduction. This includes maintaining optimal lipid levels, controlling blood pressure, and managing other risk factors such as diabetes and obesity. Engaging in regular medical follow-ups, including advanced imaging when appropriate, can help track disease progression and adjust treatment plans accordingly. Emerging therapies and personalized medicine approaches will continue to refine management strategies in the coming years. By staying informed and proactive, individuals can significantly reduce their risk of developing serious cardiovascular events associated with undetected or unmanaged atherosclerosis.
Conclusion: Addressing the Hidden Threat of Silent Atherosclerosis
Atherosclerotic heart disease of the native coronary artery without angina pectoris presents a unique challenge in cardiovascular health. Despite its silent progression, it poses a substantial risk for adverse events, necessitating proactive identification and management. The presence of mild soft plaque underscores the importance of advanced diagnostic techniques and targeted therapeutic interventions. By emphasizing risk factor modification, early detection, and personalized treatment strategies, healthcare providers can mitigate the burden of this condition and improve long-term cardiovascular outcomes.
Ongoing research continues to refine our understanding of atherosclerosis and its subclinical manifestations. As diagnostic tools become more sophisticated and treatment options expand, the ability to intervene earlier and more effectively will shape the future of cardiovascular medicine. Patients and clinicians alike must remain vigilant in addressing this hidden but significant threat to heart health.
coronary artery disease management, cardiovascular health strategies, heart disease prevention tips, early signs of heart disease, silent heart disease risks, cholesterol and heart health, plaque buildup in arteries, heart disease without chest pain, coronary artery screening methods, managing heart disease risk factors, inflammation and heart disease, lifestyle changes for heart health, advanced heart disease treatments, coronary artery imaging techniques, endothelial dysfunction and atherosclerosis, mild coronary artery disease, heart attack risk factors, cardiovascular disease progression, non-invasive heart disease diagnosis, heart health optimization
Further Reading:
Atherosclerosis and Coronary Artery Disease
Atherosclerotic cardiovascular disease risk assessment
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.