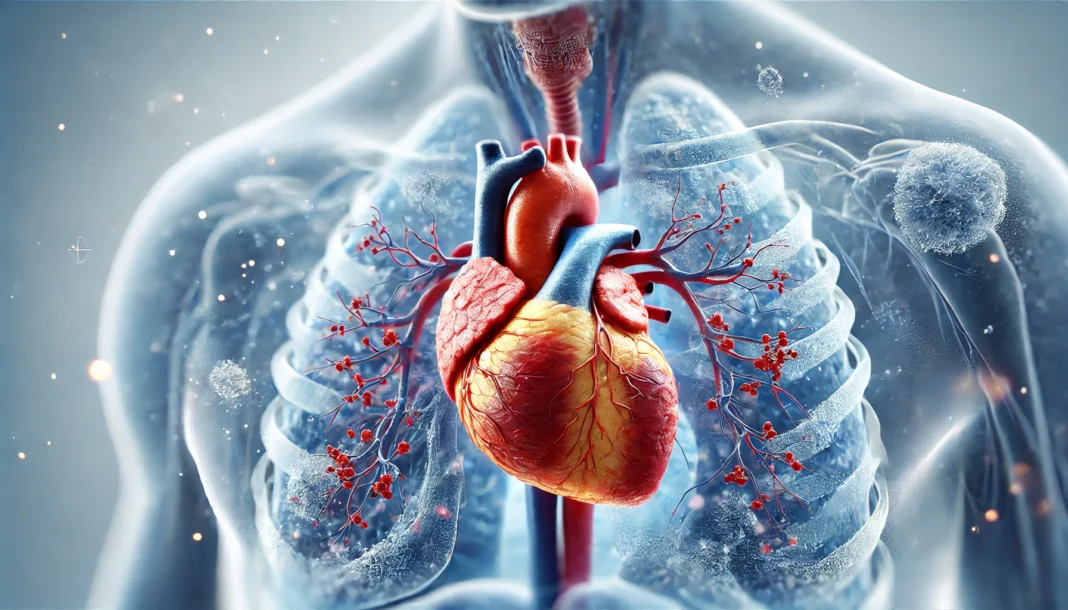
Cardiopulmonary disease refers to a broad category of medical conditions that affect both the heart and lungs, often leading to severe health complications and diminished quality of life. The intricate interplay between the cardiovascular and respiratory systems makes it essential to understand how disorders in one system can significantly impact the other. Whether acute or chronic, cardiopulmonary diseases can lead to substantial morbidity and mortality worldwide. In recent years, increasing awareness of these conditions has driven medical research aimed at improving early detection, prevention, and treatment strategies.
You may also like: 5 Modern Treatments for Heart Disease: Advancements in Cardiac Care
The Interdependence of the Cardiovascular and Respiratory Systems
The human body relies on a well-coordinated relationship between the heart and lungs to maintain oxygen supply and circulation. The heart pumps oxygenated blood received from the lungs to the rest of the body, ensuring that tissues receive the necessary nutrients to function properly. When either system fails, the consequences can be life-threatening. Cardiopulmonary diseases often arise due to various factors, including genetic predisposition, environmental influences, and lifestyle choices such as smoking, poor diet, and lack of physical activity. Understanding how these diseases manifest can aid in early intervention and improve patient outcomes.
Common Types of Cardiopulmonary Diseases
1. Chronic Obstructive Pulmonary Disease (COPD)
COPD is a progressive lung disease characterized by airway obstruction and difficulty breathing. It encompasses conditions such as chronic bronchitis and emphysema, both of which result in impaired airflow and reduced oxygen exchange. Smoking remains the leading cause of COPD, although environmental pollutants and genetic factors also play significant roles. Patients with COPD often experience persistent coughing, wheezing, and shortness of breath. Over time, the increased strain on the lungs can lead to complications such as right-sided heart failure, a condition known as cor pulmonale.
2. Pulmonary Hypertension
Pulmonary hypertension is a type of high blood pressure that affects the arteries in the lungs and the right side of the heart. It arises when the pulmonary arteries become narrowed or blocked, leading to increased resistance to blood flow. The heart must work harder to pump blood through the lungs, eventually causing heart muscle weakness and failure. Symptoms include shortness of breath, chest pain, and fainting episodes. While some cases of pulmonary hypertension are idiopathic, others are secondary to conditions such as COPD, sleep apnea, or connective tissue disorders.
3. Acute Cardiopulmonary Disease
Acute cardiopulmonary disease refers to sudden, severe conditions that impair heart and lung function. Examples include acute respiratory distress syndrome (ARDS), pulmonary embolism, and acute heart failure. These conditions often develop rapidly and require immediate medical intervention. For instance, pulmonary embolism occurs when a blood clot travels to the lungs, blocking circulation and leading to potentially fatal consequences. ARDS, on the other hand, results from severe lung inflammation, leading to fluid buildup and decreased oxygen exchange. Timely diagnosis and aggressive treatment are crucial for survival.
4. Congestive Heart Failure (CHF) and Its Pulmonary Implications
Congestive heart failure occurs when the heart is unable to pump blood effectively, leading to fluid buildup in the lungs and other tissues. This condition results in symptoms such as shortness of breath, fatigue, and swelling in the extremities. Left-sided heart failure commonly leads to pulmonary congestion, as fluid leaks into the alveoli, causing respiratory distress. Managing CHF often involves medication, lifestyle changes, and in some cases, surgical interventions such as pacemaker implantation or heart transplants.

Causes and Risk Factors of Cardiopulmonary Disease
Several factors contribute to the development of cardiopulmonary diseases. While some are genetic, many are modifiable through lifestyle changes and preventive measures.
- Smoking and Tobacco Use: Cigarette smoking remains the primary cause of many cardiopulmonary diseases, including COPD and lung cancer. The harmful chemicals in tobacco damage lung tissue and contribute to inflammation and airway constriction.
- Obesity and Sedentary Lifestyle: Excess weight places additional strain on the heart and lungs, increasing the risk of conditions such as hypertension, obstructive sleep apnea, and heart failure. Regular physical activity can mitigate these risks by improving cardiovascular fitness and lung function.
- Environmental Exposures: Long-term exposure to air pollution, industrial chemicals, and allergens can lead to chronic respiratory conditions. Workers in hazardous environments, such as coal miners and construction workers, face an increased risk of developing lung diseases.
- Genetic Predisposition: Some individuals inherit genetic conditions that predispose them to cardiopulmonary diseases. Alpha-1 antitrypsin deficiency, for example, is a hereditary disorder that increases the likelihood of developing COPD, even in non-smokers.
- Pre-existing Medical Conditions: Hypertension, diabetes, and chronic kidney disease are known to contribute to the development and progression of cardiopulmonary diseases. Managing these conditions effectively can reduce associated risks.
Symptoms and Diagnosis
Symptoms of cardiopulmonary diseases vary depending on the specific condition but often include shortness of breath, chest discomfort, fatigue, and fluid retention. Early recognition of these symptoms can lead to prompt medical evaluation and intervention. Diagnostic tools used to assess cardiopulmonary health include:
- Pulmonary Function Tests (PFTs): These tests measure lung capacity and airflow, aiding in the diagnosis of conditions like COPD and asthma.
- Electrocardiogram (ECG): An ECG records electrical activity in the heart, helping to detect abnormalities such as arrhythmias and ischemia.
- Echocardiogram: This imaging test assesses heart function and structure, providing valuable information about cardiac performance.
- Chest X-rays and CT Scans: Imaging studies help visualize lung and heart structures, identifying issues such as fluid accumulation or pulmonary embolism.
- Blood Tests: Markers such as brain natriuretic peptide (BNP) and arterial blood gases (ABGs) can provide insights into heart failure and respiratory function.
Treatment Options
Treatment for cardiopulmonary diseases depends on the underlying condition but generally includes a combination of medications, lifestyle modifications, and medical procedures.
- Medications: Commonly prescribed drugs include bronchodilators for COPD, anticoagulants for pulmonary embolism, and beta-blockers for heart failure.
- Oxygen Therapy: Patients with severe lung disease may require supplemental oxygen to improve breathing and enhance quality of life.
- Surgical Interventions: In advanced cases, procedures such as lung transplants, valve replacements, or coronary artery bypass grafting (CABG) may be necessary.
- Lifestyle Changes: Smoking cessation, weight management, and a heart-healthy diet play crucial roles in disease management.

Frequently Asked Questions About Cardiopulmonary Disease
1. How does acute cardiopulmonary disease differ from chronic conditions?
Acute cardiopulmonary disease develops suddenly, often triggered by infections, trauma, or rapid deterioration of heart and lung function. Conditions such as acute respiratory distress syndrome (ARDS) or pulmonary embolism require immediate medical intervention to prevent severe complications. Unlike chronic cardiopulmonary diseases, which progress over time, acute cases can emerge within hours or days, posing life-threatening risks if untreated. Medical professionals prioritize swift diagnosis using imaging and blood tests to determine the underlying cause. In contrast, chronic cardiopulmonary diseases, like chronic obstructive pulmonary disease (COPD) or congestive heart failure, develop gradually and require long-term management to control symptoms and prevent exacerbations.
2. What are some early warning signs of cardiopulmonary disease that people often overlook?
Many individuals dismiss early symptoms of cardiopulmonary disease, attributing them to aging or lack of fitness. Subtle warning signs include mild shortness of breath during routine activities, persistent fatigue, and unexplained swelling in the ankles or legs. Some people experience chest discomfort that comes and goes, which can be mistaken for indigestion rather than a cardiovascular issue. Chronic coughing, particularly with mucus production, may indicate underlying pulmonary dysfunction, even in nonsmokers. Recognizing these early symptoms and seeking medical evaluation can lead to timely interventions that improve long-term health outcomes.
3. Can acute cardiopulmonary disease be prevented, or is it unavoidable?
While some cases of acute cardiopulmonary disease arise unpredictably, preventive measures can significantly lower the risk. Avoiding tobacco smoke and air pollution helps protect lung function, reducing the likelihood of acute respiratory distress syndrome or sudden exacerbations of existing conditions. Managing blood pressure and cholesterol levels decreases the chance of developing acute cardiovascular events, such as a heart attack or stroke. Individuals prone to clot formation can benefit from blood-thinning medications to prevent pulmonary embolisms. Regular exercise, a heart-healthy diet, and stress management also contribute to overall cardiopulmonary resilience, helping the body withstand sudden health challenges more effectively.
4. What lifestyle changes can help manage chronic cardiopulmonary disease?
Long-term management of cardiopulmonary disease involves strategic lifestyle modifications to slow disease progression and enhance daily functioning. Smoking cessation is paramount, as tobacco smoke exacerbates both cardiac and pulmonary conditions. Dietary adjustments, including reducing sodium intake and increasing consumption of antioxidant-rich foods, help manage blood pressure and inflammation. Regular, moderate exercise strengthens the heart and lungs without overexertion, improving oxygen utilization. Patients often benefit from pulmonary rehabilitation programs that teach controlled breathing techniques and energy conservation strategies. Emotional well-being is also crucial, as anxiety and depression can worsen physical symptoms, making stress reduction techniques like meditation or therapy valuable components of comprehensive care.
5. How does air quality impact the progression of cardiopulmonary disease?
Environmental factors play a significant role in both the development and progression of cardiopulmonary diseases. Poor air quality, particularly in urban areas with high pollution levels, can trigger inflammation in the lungs, worsening respiratory conditions such as COPD and asthma. Long-term exposure to pollutants, including fine particulate matter and industrial chemicals, increases the risk of developing pulmonary hypertension. Seasonal variations, such as increased pollen or extreme humidity, can further strain the cardiopulmonary system, leading to symptom flare-ups. Individuals with preexisting conditions should monitor air quality indexes and take precautions, such as wearing masks or using indoor air purifiers, to minimize exposure to harmful environmental triggers.
6. What role does sleep quality play in cardiopulmonary health?
Sleep is a critical yet often overlooked component of cardiopulmonary health. Conditions like obstructive sleep apnea (OSA) can significantly impact both heart and lung function, leading to intermittent oxygen deprivation during the night. Over time, untreated OSA contributes to high blood pressure, irregular heart rhythms, and increased risk of heart failure. Poor sleep quality also weakens immune function, making individuals more susceptible to respiratory infections that can exacerbate cardiopulmonary disease. Establishing good sleep hygiene, seeking evaluation for potential sleep disorders, and using continuous positive airway pressure (CPAP) therapy when necessary can greatly enhance overall health outcomes.
7. Are there emerging treatments for cardiopulmonary disease that show promise?
Advancements in medical research are continuously improving treatment options for cardiopulmonary diseases. Stem cell therapy is being explored for its potential to regenerate damaged heart and lung tissues, offering hope for patients with severe disease. Novel drug therapies targeting inflammation and fibrosis may slow disease progression in conditions like pulmonary fibrosis and chronic heart failure. Minimally invasive surgical techniques, such as transcatheter aortic valve replacement (TAVR), provide less risky alternatives for high-risk patients needing valve repairs. Wearable technology and remote monitoring devices allow real-time tracking of vital signs, enabling early detection of complications. As research progresses, these innovations may revolutionize how cardiopulmonary diseases are managed and treated.
8. How do mental health and stress influence cardiopulmonary conditions?
Psychological well-being plays a crucial role in managing cardiopulmonary diseases, yet it is frequently underestimated. Chronic stress triggers the release of stress hormones like cortisol, which can elevate blood pressure and increase heart rate, putting additional strain on the cardiovascular system. Anxiety and panic disorders can cause hyperventilation, leading to respiratory distress in individuals with compromised lung function. Depression is also common among those with chronic illness, sometimes reducing motivation for medication adherence and healthy lifestyle choices. Integrating mental health support into cardiopulmonary care—such as counseling, mindfulness practices, and support groups—can improve overall treatment adherence and quality of life.
9. How does acute cardiopulmonary disease affect different age groups?
Acute cardiopulmonary disease manifests differently across various age groups due to physiological and lifestyle differences. In younger adults, conditions like myocarditis (heart inflammation) and spontaneous pneumothorax (collapsed lung) can occur suddenly, often linked to infections or genetic predispositions. Middle-aged individuals are more likely to experience acute cardiovascular events, such as heart attacks or pulmonary embolisms, often due to prolonged lifestyle-related risk factors. Older adults, particularly those with preexisting health conditions, face a higher risk of complications from pneumonia, congestive heart failure, or acute respiratory distress syndrome. Understanding age-specific vulnerabilities allows healthcare providers to tailor prevention and treatment strategies accordingly.
10. What steps should someone take if they suspect they have cardiopulmonary disease?
If someone experiences persistent symptoms like breathlessness, chest pain, or chronic fatigue, they should seek medical evaluation promptly. Consulting a primary care physician or specialist, such as a cardiologist or pulmonologist, can help identify underlying conditions through diagnostic tests like electrocardiograms, pulmonary function tests, or imaging studies. Keeping a symptom diary can assist healthcare providers in recognizing patterns that may indicate an emerging cardiopulmonary issue. Early intervention is key, as timely treatment can prevent complications and improve long-term outcomes. In emergencies, such as sudden chest pain or difficulty breathing, immediate medical attention should be sought to rule out life-threatening conditions like a heart attack or pulmonary embolism.
Conclusion
Cardiopulmonary diseases represent a significant global health burden, requiring ongoing research and public health initiatives to improve prevention and treatment. By understanding the causes, symptoms, and available treatment options, individuals can take proactive steps toward managing their health. Early detection and lifestyle modifications remain critical in mitigating risks and enhancing quality of life. As advancements in medical research continue, the outlook for individuals with cardiopulmonary diseases will improve, offering hope for better health outcomes and increased longevity.
cardiovascular health, pulmonary disorders, heart and lung disease, respiratory failure, chronic lung conditions, cardiac dysfunction, pulmonary rehabilitation, oxygen therapy benefits, cardiopulmonary wellness, heart failure management, lung disease prevention, pulmonary circulation issues, heart-lung connection, respiratory therapy, chronic bronchitis treatment, pulmonary embolism risks, heart disease symptoms, COPD management, improving lung capacity, hypertension and heart health
Further Reading:
Types of Cardiovascular Diseases: Symptoms Prevention and Treatment
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.