Understanding Low Blood Pressure and the Role of Nutrition
Low blood pressure, medically known as hypotension, is a condition in which the force of blood against artery walls is too low to deliver adequate oxygen and nutrients throughout the body. While it might sound benign—especially when compared to high blood pressure—it can cause significant symptoms like dizziness, fainting, fatigue, and blurred vision. In more severe cases, hypotension can compromise organ perfusion, posing serious health risks. Understanding what to eat for low blood pressure is crucial, not only to alleviate these symptoms but also to address potential underlying causes such as hypovolemia, a condition defined by reduced blood volume.
You may also like: Top 15 Foods to Avoid with High Blood Pressure: What Not to Eat When Managing Hypertension
Diet plays a fundamental role in both the prevention and management of hypotension. For patients experiencing chronic low blood pressure or those with acute episodes linked to dehydration, blood loss, or medical treatments, adopting a targeted nutrition strategy can support hemodynamic stability. The best foods for low blood pressure are those that help retain fluids, boost blood volume, provide essential electrolytes, and improve vascular tone. At the same time, understanding how to help a patient with hypovolemia diet interventions requires a deeper look at fluid-salt balance, protein intake, and strategic meal planning.
This article explores the science-backed relationship between food and hypotension, offering practical, evidence-based insights into the best low bp food choices and the dietary needs of those with hypovolemia.
The Physiology of Hypotension and Hypovolemia
To fully grasp how food influences blood pressure, it’s essential to understand the physiological mechanisms behind hypotension and hypovolemia. Hypotension occurs when there is insufficient pressure to circulate blood efficiently, leading to reduced perfusion to vital organs. This can result from several factors, including reduced cardiac output, autonomic dysfunction, or decreased blood volume.
Hypovolemia, a common cause of low blood pressure, refers specifically to a drop in the circulating blood or plasma volume. It is frequently caused by dehydration, hemorrhage, or fluid loss through vomiting, diarrhea, or diuretics. When blood volume decreases, the heart has less material to pump, and systemic pressure drops. Thus, low blood pressure treatment food strategies must target the restoration of blood volume and electrolyte balance.
The hypovolemia diet should be carefully crafted to address both macronutrient and micronutrient needs. Sodium, potassium, fluid intake, and even protein can influence plasma osmolarity and fluid retention, which in turn affects blood pressure. For example, foods that promote water retention through sodium balance can be helpful, while those rich in iron and B vitamins support red blood cell production, critical in cases of blood loss.
Key Dietary Principles for Managing Low Blood Pressure
For individuals struggling with chronic hypotension or acute hypovolemia, tailoring dietary choices becomes a form of therapy. The low blood diet must consider not only what is consumed but also when and how often food is eaten. Large meals may cause postprandial hypotension, a drop in blood pressure after eating, while small, frequent meals can stabilize energy levels and reduce such risks.
The best foods for low blood pressure are typically those that support vascular tone, replenish fluid levels, and optimize electrolyte intake. Salty foods can temporarily raise blood pressure by increasing fluid retention, while fluids themselves—especially those with electrolytes—help expand blood volume. Meanwhile, foods rich in folate and vitamin B12 are essential to prevent certain forms of anemia that can exacerbate hypotension.
At the same time, clinicians and caregivers should consider how to help a patient with hypovolemia diet modifications that avoid exacerbating other conditions, such as heart failure or kidney disease. It is crucial to balance the need for sodium and fluid with a patient’s broader health profile. An individualized, evidence-based approach is key.

Salt and Electrolyte Intake: Strategic Use in Hypotension Management
Sodium is one of the most critical nutrients in the management of hypotension. It plays a direct role in water retention, thus increasing blood volume and pressure. In healthy individuals, high salt intake is often discouraged due to the risk of hypertension, but in cases of low blood pressure—particularly from hypovolemia—moderate increases in sodium can be beneficial. Foods such as olives, pickles, broth-based soups, and salted nuts are examples of low bp food options that provide both sodium and other nutrients.
For patients with hypovolemia, salt intake must also be balanced with fluid consumption to ensure rehydration. Simply increasing salt without fluids may lead to hypernatremia, a dangerous concentration of sodium in the blood. Therefore, hydration strategies that include electrolyte-rich drinks such as oral rehydration solutions, coconut water with a pinch of salt, or sports drinks can serve as both food to eat in low bp and hydration therapies.
Potassium, another key electrolyte, helps regulate heart rhythm and muscle function. While excessive potassium can lower blood pressure, moderate intake from natural sources like bananas, potatoes, and leafy greens supports cardiovascular health. The hypovolemia diet must be tailored to avoid imbalances, especially in patients taking diuretics or those with renal impairment.
Protein and Iron: Building Blocks for Blood Volume Restoration
Protein plays a vital role in vascular health and plasma oncotic pressure, which helps retain fluid within blood vessels. Albumin, the primary plasma protein, is synthesized from dietary protein and is critical in maintaining intravascular volume. For individuals recovering from hypovolemia, particularly due to trauma or surgery, adequate protein intake supports tissue repair and plasma volume restoration.
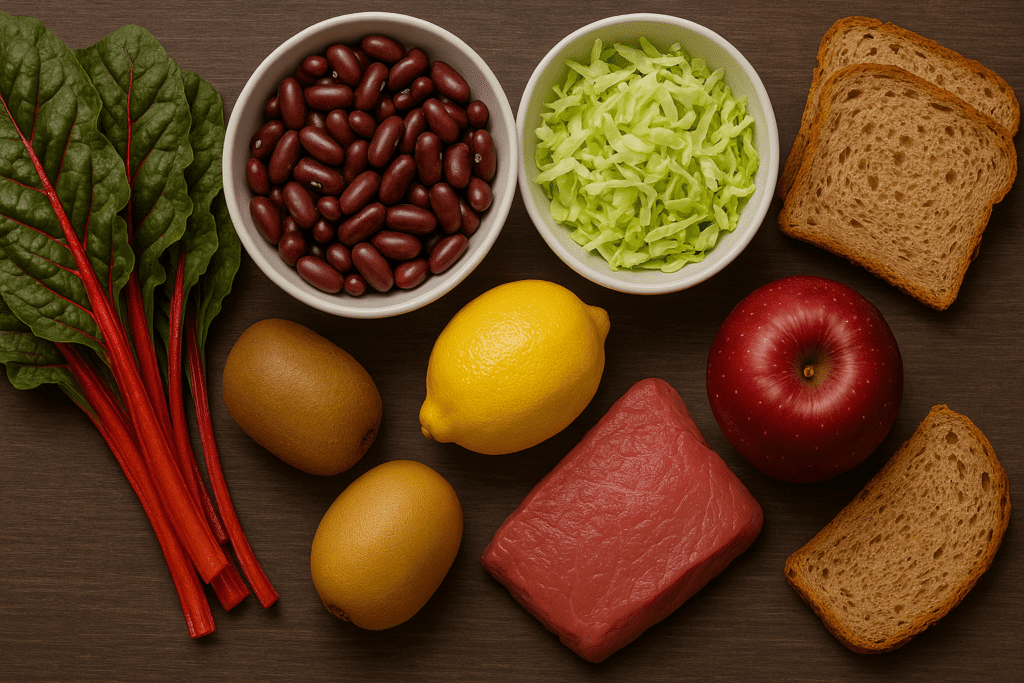
Lean meats, eggs, dairy, legumes, and tofu are excellent sources of high-quality protein and are among the best foods for low blood pressure in patients needing blood volume support. These foods also provide iron, which is essential for hemoglobin synthesis. Iron deficiency anemia is a known contributor to hypotension symptoms such as fatigue, dizziness, and pallor.
When exploring low blood pressure causes of food-related deficiencies, inadequate iron or vitamin B12 intake should be ruled out. Addressing these gaps through food rather than supplements may be more sustainable and less likely to cause gastrointestinal side effects. Incorporating iron-rich options like red meat, fortified cereals, and dark leafy greens, along with vitamin C to enhance absorption, can be a practical part of any low blood diet.
Fluid Intake: Optimizing Hydration for Circulatory Stability
While solid foods are essential, fluid intake is equally critical in managing hypotension. Dehydration is a major contributor to hypovolemia and can drastically lower blood pressure. As such, patients must understand not just how much to drink, but what types of fluids are most effective. Plain water, while beneficial, may not be sufficient for restoring electrolyte balance in all cases.
For individuals with recurring low blood pressure, especially those who experience orthostatic hypotension, drinking water with a pinch of salt before getting out of bed can prevent sudden drops in pressure. Herbal teas, diluted fruit juices, and homemade electrolyte drinks can also be classified as good food for hypotension when used correctly. These fluids should be spaced throughout the day to maintain consistent blood volume and prevent rapid fluctuations.
In the hypovolemia diet, the emphasis is often placed on combining hydration with mineral balance. For instance, broths provide both fluids and sodium, making them a dual-purpose remedy. In clinical settings, oral rehydration therapy is sometimes prescribed, particularly in patients with severe dehydration or gastrointestinal fluid losses. These medically formulated drinks contain an optimal ratio of glucose and sodium to enhance absorption and retention.
Small, Frequent Meals: Stabilizing Blood Pressure Through Meal Timing
Beyond the types of food consumed, the timing and frequency of meals can have a substantial impact on blood pressure regulation. Large meals can divert blood to the digestive system, leading to postprandial hypotension, particularly in older adults or individuals with autonomic dysfunction. As such, adopting a schedule of small, frequent meals can be a valuable strategy in a low blood diet plan.
Eating every three to four hours keeps energy levels stable and helps avoid sharp drops in pressure. Meals that combine complex carbohydrates with proteins and healthy fats provide sustained energy release and prevent sudden spikes or dips in insulin, which can indirectly affect blood pressure. Including snacks such as cheese with whole-grain crackers, yogurt with nuts, or hummus with vegetables can be helpful examples of what to eat for low blood conditions.
Meal planning also provides an opportunity to strategically incorporate low bp food options throughout the day. For example, a mid-morning snack of salted almonds, followed by a lunch rich in lean protein and leafy greens, can help manage symptoms while supporting long-term cardiovascular health. In this way, dietary planning becomes a proactive tool in managing hypotension.
Micronutrients That Support Vascular Tone and Circulatory Health
While macronutrients like protein and carbohydrates provide the bulk of energy and structure, micronutrients play a critical role in regulating vascular function. Magnesium, calcium, folate, and B vitamins are among the most important nutrients for maintaining optimal blood pressure and cardiovascular function. Deficiencies in any of these can contribute to hypotension symptoms and should be addressed through a carefully balanced diet.
Magnesium supports muscle contraction, including the heart, and may help stabilize blood pressure by influencing vascular tone. Foods such as avocados, pumpkin seeds, and dark chocolate are rich sources of magnesium and can be included in a good food for hypotension plan. Similarly, calcium, found in dairy products and leafy greens, contributes to vascular constriction and should not be overlooked.
Folate and vitamin B12 are essential for red blood cell production and preventing anemia-related hypotension. A deficiency in either nutrient can lead to megaloblastic anemia, which is characterized by large, dysfunctional red cells that impair oxygen delivery. Fortified grains, eggs, and lean meats can serve as foundational elements of a hypovolemia diet focused on red cell support and oxygenation.
Dietary Triggers to Avoid in Hypotension
While much attention is given to what to eat in low bp conditions, it is equally important to understand which foods may exacerbate symptoms. High-sugar foods, caffeine, and alcohol can all trigger blood pressure fluctuations. Sugar, in particular, may cause a rapid rise in insulin followed by a sudden drop in blood pressure, especially if consumed without fiber or protein.
Caffeine can have a temporary pressor effect, raising blood pressure slightly, but its diuretic properties may lead to fluid loss over time, which is counterproductive in hypovolemia. Similarly, alcohol dehydrates the body and can lower blood pressure significantly when consumed in large quantities. Individuals managing hypotension or following a hypovolemia diet should be mindful of these effects.
Moreover, very low-calorie or restrictive diets may lead to nutrient deficiencies and worsening symptoms. Eliminating entire food groups without medical supervision can increase the risk of low blood pressure causes of food-related imbalances. A balanced, evidence-based approach that emphasizes whole foods and adequate nutrition is essential.
How to Help a Patient with Hypovolemia Diet Strategies
Helping a patient manage hypovolemia through diet requires more than just nutritional advice—it involves clinical awareness, careful monitoring, and personalized planning. In acute cases, intravenous fluids may be necessary, but once stabilized, dietary strategies can play a restorative role. Encouraging regular intake of salty foods, adequate fluids, and nutrient-rich meals can prevent recurrence and support long-term recovery.
The hypovolemia diet must be adapted to the patient’s individual health status, comorbid conditions, and preferences. For example, patients with heart disease may require careful sodium management, while those with renal impairment may need to limit potassium intake. Monitoring weight, urine output, and vital signs can help determine the effectiveness of dietary changes.
Education is also key—patients and caregivers should understand the signs of dehydration and low blood volume and know what to eat in low bp situations to prevent complications. In outpatient settings, registered dietitians and physicians can collaborate to ensure that diet supports both symptom management and overall health outcomes.

Frequently Asked Questions (FAQ)
Focused on Diet for Low Blood Pressure and Hypovolemia Recovery
1. Can a hypovolemia diet include high-sodium processed foods, or are there healthier options?
While processed foods are often high in sodium, they may also contain harmful additives, trans fats, and excess sugars, which can undermine overall cardiovascular health. When considering how to help a patient with hypovolemia diet planning, it’s more beneficial to choose whole food sources of sodium such as lightly salted nuts, broths made from scratch, or pickled vegetables without artificial preservatives. These options support fluid retention while supplying micronutrients that contribute to vascular tone. Including these in a low blood diet helps avoid over-reliance on nutritionally empty, ultra-processed options. The best food for low bp should raise blood volume without increasing cardiovascular risk.
2. Are there specific herbs or spices that support blood pressure regulation in hypotension?
Certain herbs and spices may offer subtle cardiovascular benefits for those exploring what to eat for low blood. For instance, licorice root can temporarily raise blood pressure but should be used with caution and medical supervision due to potential potassium loss. Adaptogenic herbs like ashwagandha and rhodiola may help those with hypotension linked to adrenal fatigue or stress. When incorporated thoughtfully into a hypovolemia diet, these botanicals may support broader autonomic balance, especially in patients with postural hypotension. However, whole-food strategies remain the foundation of any good food for hypotension regimen.
3. How can meal composition impact symptoms of low blood pressure throughout the day?
Meal composition significantly influences post-meal blood pressure regulation. High-carb meals, especially those rich in refined sugars, can cause rapid insulin responses that lower blood pressure soon after eating. Balancing macronutrients by combining protein, fiber, and healthy fats with complex carbohydrates can prevent these crashes. Therefore, the best foods for low blood pressure include balanced meals like quinoa with chicken and vegetables or Greek yogurt with chia seeds and berries. Tailoring food to eat in low bp situations means planning meals that support sustained vascular tone across the day.
4. Can fasting or intermittent fasting worsen hypotension or hypovolemia symptoms?
Yes, prolonged fasting can exacerbate hypotension symptoms, particularly in individuals who already struggle with blood volume or autonomic regulation. Skipping meals may result in lower circulating glucose and fluid levels, contributing to dizziness and fatigue. For individuals on a low blood diet, it’s essential to maintain consistent food and fluid intake throughout the day to avoid volume depletion. When considering how to help a patient with hypovolemia diet adaptations, practitioners should discourage restrictive eating patterns unless medically justified and closely supervised.
5. How does climate and seasonal variation affect dietary needs in hypotension?
Hot and humid weather increases fluid loss through sweating, which can worsen hypovolemia and lower blood pressure. In such conditions, adjusting the hypovolemia diet to include more hydrating foods like watermelon, cucumber, and electrolyte-rich smoothies becomes especially important. During winter, blood vessels naturally constrict in response to cold, which may help raise blood pressure slightly, allowing for a bit more flexibility in sodium intake. Adapting what to eat in low bp conditions requires seasonal awareness to maintain circulatory stability. This includes adjusting fluid intake based on activity levels and weather patterns.
6. Are there specific cultural or regional diets that naturally support hypotension recovery?
Yes, several traditional diets contain elements beneficial for individuals seeking low bp food options. The Mediterranean diet, for instance, includes olives, cheeses, and anchovies, which naturally supply sodium, along with potassium-rich produce and healthy fats that support vascular tone. Similarly, Japanese miso-based soups provide a gentle sodium boost alongside probiotics and minerals. When applying cultural food knowledge to a hypovolemia diet, it’s important to identify regional staples that double as low blood pressure treatment food. Personalized care that incorporates cultural food preferences can enhance compliance and recovery.
7. How can caregivers support long-term adherence to a low blood diet in older adults?
For elderly individuals, especially those with cognitive decline or mobility limitations, maintaining adequate nutrition and hydration can be challenging. Caregivers can enhance adherence by preparing visually appealing meals that include best food for low bp management, such as egg-based dishes with leafy greens or warm broths with tender chicken and root vegetables. Flavor enhancement using herbs, citrus, or modest salt additions can also stimulate appetite. Encouraging regular meal routines and offering foods that are easy to chew and digest is crucial when thinking about how to help a patient with hypovolemia diet strategies tailored to older populations.
8. What role does emotional and psychological support play in hypotension management through diet?
Mental health significantly impacts dietary habits and adherence. Individuals dealing with chronic hypotension may experience fatigue and low mood, which in turn affect their motivation to eat regularly or prepare balanced meals. Stress can also influence gut health and nutrient absorption, further complicating the efficacy of a low blood diet. Providing emotional support and education around food choices can improve outcomes. When identifying what to eat for low blood conditions, integrating supportive counseling or nutritional coaching may be just as important as the food itself.
9. Is there any research on the gut microbiome’s role in blood pressure regulation in hypotensive individuals?
Emerging studies suggest that the gut microbiome may play a role in regulating blood pressure, primarily through its influence on inflammation, nutrient absorption, and nervous system signaling. For those following a hypovolemia diet, incorporating fermented foods like kefir, sauerkraut, and kimchi may help promote microbial diversity and better nutrient extraction. These foods also support immune function and digestion, enhancing overall resilience in hypotensive individuals. As research evolves, dietary interventions targeting the microbiome may become a novel pathway for developing good food for hypotension with added metabolic benefits.
10. How can someone track and personalize their response to different low bp food choices?
Keeping a symptom and nutrition journal is a practical method for understanding how various foods impact blood pressure throughout the day. Individuals can log meals, hydration, physical activity, and symptoms such as dizziness or fatigue. Over time, this data helps identify patterns, such as which best foods for low blood pressure lead to more energy or fewer symptoms. Personalized tracking empowers patients to make informed choices and refine their food to eat in low bp episodes. This self-awareness becomes an essential part of low blood pressure treatment food strategies, especially in patients with fluctuating or unpredictable symptoms.
Conclusion: Building a Stronger Circulatory System Through Diet
Choosing the best food for low bp is not simply about raising blood pressure temporarily—it’s about creating a sustainable nutritional foundation that supports cardiovascular health, fluid balance, and overall well-being. A well-formulated low blood diet that includes strategic salt and fluid intake, protein and iron-rich foods, and essential micronutrients can dramatically improve the quality of life for individuals with chronic hypotension or hypovolemia.
By understanding the relationship between nutrition and blood pressure regulation, patients and clinicians alike can make informed choices. Whether the goal is to manage symptoms, prevent future episodes, or support recovery from blood volume loss, the right dietary strategies can be as powerful as pharmacologic interventions—without the side effects.
As research continues to uncover new connections between diet and vascular health, the importance of personalized, evidence-based nutrition becomes increasingly clear. Knowing what to eat for low blood pressure, how to help a patient with hypovolemia diet changes, and which foods support circulatory strength offers a pathway not only to symptom relief but also to lasting wellness and resilience.
foods that raise blood pressure naturally, hydration and cardiovascular health, managing hypotension with nutrition, symptoms of low blood volume, dietary support for dizziness, salt and electrolyte balance, protein-rich meals for blood health, fluid retention foods, anemia and low blood pressure, vascular support through diet, nutrient deficiencies and hypotension, sodium and fluid regulation, iron-rich diet for fatigue, B12 and folate for blood health, healthy meals for orthostatic hypotension, postural hypotension diet tips, circulatory health foods, managing fatigue with nutrition, autonomic dysfunction and diet, blood pressure regulation strategies
Further Reading:
What to eat with low blood pressure
How to Manage Low Blood Pressure with Diet?
13 ways to raise blood pressure
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.


