Introduction: Connecting the Breath and the Heart
When we think about heart health, we often picture blood pressure, cholesterol levels, or physical activity. Yet, there’s a hidden factor that significantly affects cardiovascular health, often flying under the radar: sleep apnea. This sleep-related breathing disorder is more than just loud snoring or restless nights. It’s a serious condition with the potential to harm the heart, disrupt the vascular system, and contribute to long-term cardiovascular problems. As research continues to evolve, the medical community increasingly recognizes the deep and intricate relationship between sleep apnea and heart health. Understanding this connection is vital not only for diagnosis but also for effective prevention and management of heart disease.
You may also like: 5 Ways to Keep Your Heart Healthy and Prevent Cardiovascular Disease
Sleep apnea heart problems are not just theoretical associations; they are supported by growing evidence from epidemiological, clinical, and physiological studies. From increased risks of hypertension and arrhythmias to heart failure and stroke, sleep apnea casts a wide net over cardiovascular health. For millions who suffer from this condition, awareness is the first step toward recovery. In this article, we’ll explore the mechanisms through which sleep apnea affects the heart, examine the types of cardiovascular issues it contributes to, and highlight strategies to mitigate these effects.
What Is Sleep Apnea? A Closer Look at This Breathing Disorder
Sleep apnea is a chronic disorder characterized by repeated interruptions in breathing during sleep. The most common form, obstructive sleep apnea (OSA), occurs when the muscles at the back of the throat fail to keep the airway open. Central sleep apnea, on the other hand, stems from the brain’s failure to send proper signals to the muscles that control breathing. In some individuals, a combination of both forms—known as complex sleep apnea—may occur.
These breathing interruptions often last 10 seconds or more and can occur dozens or even hundreds of times per night. As a result, oxygen levels in the blood drop, and sleep becomes fragmented and poor in quality. Many people with sleep apnea are unaware of these episodes, though they may experience symptoms such as excessive daytime sleepiness, morning headaches, irritability, or difficulty concentrating.
Left untreated, sleep apnea leads to more than just fatigue. It contributes to metabolic disturbances, inflammatory responses, and increased cardiovascular strain—all of which set the stage for serious heart conditions. The impact is not just theoretical; sleep apnea heart problems have been documented across multiple clinical studies, confirming that this disorder is a significant, independent risk factor for cardiovascular disease.
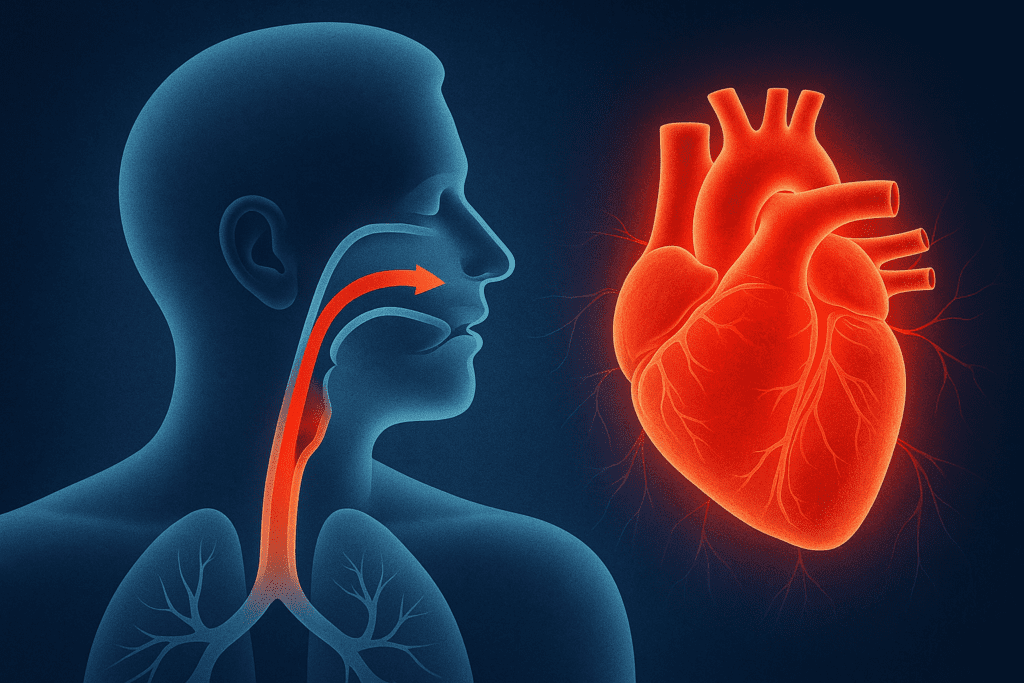
The Physiological Impact: How Sleep Apnea Stresses the Cardiovascular System
To understand the connection between sleep apnea and cardiovascular issues, we must look at what happens in the body during an apneic event. When breathing stops, oxygen levels in the blood fall—a condition known as hypoxemia. Simultaneously, carbon dioxide builds up, triggering a stress response. The body releases stress hormones such as adrenaline and cortisol, which elevate heart rate and blood pressure in an effort to restore oxygen balance.
These repeated stress responses activate the sympathetic nervous system—the same system responsible for the “fight or flight” response. Over time, chronic activation of this system increases baseline blood pressure, disrupts heart rhythm, and damages blood vessel walls. In short, sleep apnea doesn’t just interrupt sleep; it acts as a nightly assault on the heart and circulatory system.
Furthermore, the abrupt surges in blood pressure that accompany each breathing pause can cause shear stress on arteries, leading to endothelial dysfunction. This dysfunction impairs the ability of blood vessels to dilate properly, contributing to the development of atherosclerosis. As the vascular system becomes increasingly compromised, the heart must work harder to circulate blood, setting the stage for long-term cardiovascular complications.
Hypertension and Sleep Apnea: A Dangerous Duo
One of the most well-established links between sleep apnea and heart health is the relationship with hypertension. Studies have shown that up to 50% of people with sleep apnea also have high blood pressure, and vice versa. This bidirectional relationship suggests a shared pathophysiology involving chronic inflammation, sympathetic overactivity, and oxidative stress.
Sleep apnea causes blood pressure to spike during sleep due to repeated drops in oxygen levels and arousal from sleep. These nocturnal surges contribute to a phenomenon known as “non-dipping” blood pressure—a lack of the typical nighttime decrease in blood pressure. Non-dipping status has been linked with higher risks of cardiovascular events, including heart attacks and strokes.
Treating sleep apnea with continuous positive airway pressure (CPAP) therapy has been shown to help lower blood pressure, particularly in individuals with resistant hypertension. This underscores the importance of screening patients with high blood pressure for possible sleep apnea, especially when traditional antihypertensive treatments fail to achieve target blood pressure levels. Addressing sleep apnea heart problems can be a crucial component of effective blood pressure management.
Sleep Apnea and Heart Rhythm Disorders: Atrial Fibrillation and Beyond
Heart rhythm disturbances, especially atrial fibrillation (AFib), are another significant concern in individuals with sleep apnea. AFib is characterized by rapid and irregular beating of the atrial chambers of the heart, and it significantly increases the risk of stroke and heart failure.
Research has shown that individuals with sleep apnea are more likely to develop AFib, and those who already have AFib are more prone to recurrence if their sleep apnea goes untreated. The mechanisms behind this include intermittent hypoxia, inflammation, increased atrial pressure, and structural remodeling of heart tissue due to frequent arousals and blood pressure surges.
Other arrhythmias associated with sleep apnea include bradycardia (abnormally slow heart rate) and ventricular ectopy (irregular heartbeats). These arrhythmias often occur during episodes of apnea and can result in poor perfusion and sudden cardiac events. Addressing the underlying breathing disorder can often improve or even resolve these rhythm abnormalities, highlighting the interplay between sleep apnea heart issues and electrical conduction in the heart.

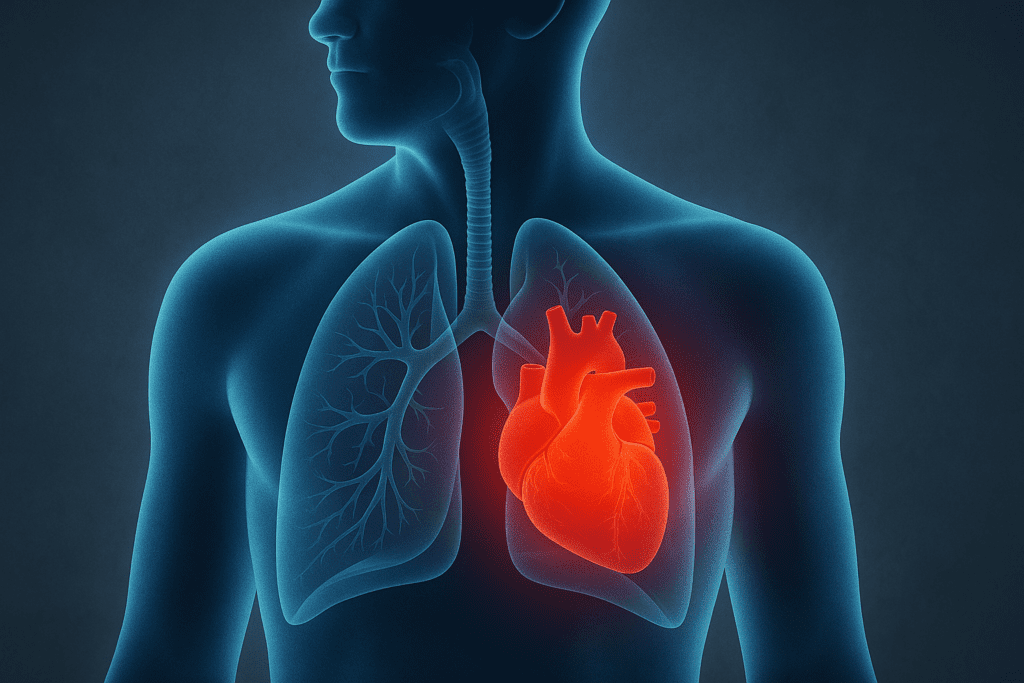
The Threat of Heart Failure: How Sleep Apnea Weakens the Heart Over Time
Sleep apnea does not merely coexist with heart failure—it can actively contribute to its development and progression. Both obstructive and central sleep apnea are highly prevalent among individuals with heart failure. In fact, studies estimate that over 50% of heart failure patients suffer from some form of sleep-disordered breathing.
The recurrent oxygen desaturation and surges in sympathetic activity strain the heart, particularly the left ventricle, which is responsible for pumping oxygenated blood throughout the body. Over time, this strain can lead to left ventricular hypertrophy (thickening of the heart muscle), reduced cardiac output, and fluid retention—hallmarks of heart failure.
Moreover, central sleep apnea is especially common in individuals with heart failure and often presents as Cheyne-Stokes respiration, a distinctive breathing pattern marked by waxing and waning ventilation. This form of sleep apnea indicates poor cardiac function and is associated with worse outcomes and higher mortality rates.
Effective treatment of sleep apnea in heart failure patients, such as CPAP or adaptive servo-ventilation, has been shown to improve cardiac function, quality of life, and exercise tolerance. Recognizing and addressing sleep apnea heart issues in these patients can therefore play a critical role in comprehensive heart failure management.
Stroke Risk and Cerebrovascular Complications
Beyond the heart, sleep apnea also poses a significant threat to the brain. Individuals with sleep apnea have an increased risk of stroke, even after adjusting for traditional risk factors such as age, sex, smoking, and hypertension. The mechanisms driving this risk include endothelial dysfunction, hypercoagulability (increased blood clotting tendency), and systemic inflammation—all consequences of untreated sleep apnea.
Nocturnal hypoxia and repeated blood pressure spikes can damage small blood vessels in the brain, making them more prone to rupture or blockage. Furthermore, the fragmentation of sleep caused by frequent awakenings impairs glucose metabolism and elevates stress hormones, creating a metabolic environment conducive to cerebrovascular events.
Importantly, stroke survivors with untreated sleep apnea often have worse recovery outcomes, reduced neuroplasticity, and higher rates of recurrent stroke. For this reason, many stroke centers now include sleep apnea screening as part of their post-stroke evaluation protocols. The recognition of sleep apnea heart problems is thus extending to the broader vascular system, emphasizing the systemic impact of this disorder.
Diagnosis and Screening: Identifying Sleep Apnea Early to Protect the Heart
Despite its serious implications, sleep apnea remains underdiagnosed. Many individuals are unaware they have the condition, attributing symptoms like fatigue, snoring, or nighttime awakenings to stress or aging. This lack of awareness delays intervention and increases the risk of heart complications.
Polysomnography, or a sleep study, remains the gold standard for diagnosing sleep apnea. Home sleep apnea tests (HSATs) have become increasingly accessible and reliable, offering a convenient alternative for many patients. Risk assessment tools such as the STOP-Bang questionnaire can help clinicians identify individuals at high risk who should undergo further testing.
Importantly, cardiologists and primary care providers should maintain a high index of suspicion in patients with resistant hypertension, arrhythmias, or unexplained heart failure. Early diagnosis and treatment of sleep apnea can significantly alter the trajectory of cardiovascular health and reduce long-term risks.
Treatment Strategies: Managing Sleep Apnea for a Healthier Heart
Continuous positive airway pressure (CPAP) therapy remains the most effective and widely used treatment for obstructive sleep apnea. By delivering a steady stream of air to keep the airway open, CPAP prevents apneic events and stabilizes oxygen levels during sleep. For many patients, this leads to significant improvements in blood pressure, heart rhythm, and overall cardiovascular health.
Alternative treatments include mandibular advancement devices, weight loss, positional therapy, and, in some cases, surgery. Lifestyle interventions such as reducing alcohol consumption, quitting smoking, and managing weight are also critical in improving both sleep apnea and heart health.
Adherence to treatment is key. Many patients initially struggle with CPAP but find success with proper support, mask fitting, and education. When sleep apnea is effectively managed, the burden on the cardiovascular system decreases, demonstrating how directly sleep apnea heart problems can be improved with targeted intervention.
Frequently Asked Questions: How Sleep Apnea Affects Heart Health
1. Can sleep apnea worsen existing heart conditions even if it’s mild?
Yes, even mild cases of sleep apnea can subtly but steadily contribute to cardiovascular decline. While severe cases often draw medical attention, low-grade sleep apnea can still provoke intermittent oxygen deprivation, triggering low-level inflammation and sympathetic nervous system activation. Over time, these effects accumulate and can exacerbate pre-existing heart conditions like arrhythmias or hypertensive heart disease. Mild sleep apnea heart problems are often underestimated, yet studies show they may accelerate vascular aging and disrupt normal blood pressure regulation. Regular monitoring and lifestyle interventions are crucial, even in seemingly “mild” cases.
2. Are people with sleep apnea more prone to developing high cholesterol and metabolic syndrome?
Emerging research suggests a strong correlation between sleep apnea and metabolic dysregulation, including elevated LDL cholesterol and insulin resistance. This metabolic dysfunction can increase the likelihood of developing atherosclerosis, compounding sleep apnea heart problems over time. The repeated episodes of nocturnal hypoxia associated with sleep apnea stimulate systemic inflammation and oxidative stress, which interfere with lipid metabolism. Moreover, disrupted sleep affects hormonal balance, particularly cortisol and leptin, further promoting fat accumulation and dyslipidemia. Thus, managing sleep apnea effectively may help reduce the cardiometabolic burden and lower the long-term risk of cardiovascular disease.
3. How do emotional and psychological factors interact with sleep apnea and heart health?
The triad of poor sleep, emotional stress, and cardiovascular strain creates a self-perpetuating cycle. Individuals with untreated sleep apnea often experience mood disorders such as anxiety and depression, which in turn elevate stress hormone levels like cortisol and adrenaline. These hormones raise heart rate and blood pressure, deepening the physiological imprint of sleep apnea heart problems. Additionally, poor emotional regulation may discourage adherence to treatment like CPAP therapy, further worsening outcomes. Integrating mental health support into sleep apnea management can offer a more holistic and effective approach to protecting heart health.
4. Can exercise reverse or reduce the cardiovascular impact of sleep apnea?
While exercise alone doesn’t cure sleep apnea, it can significantly reduce the cardiovascular risks associated with it. Regular aerobic activity improves endothelial function, reduces systemic inflammation, and enhances parasympathetic tone, which helps counteract the hyperactive sympathetic drive caused by sleep apnea. These effects collectively diminish the severity of sleep apnea heart problems. Additionally, exercise often contributes to weight loss, which is a major modifiable risk factor for both sleep apnea and heart disease. Patients with sleep apnea are encouraged to combine CPAP therapy with structured physical activity for optimal cardiovascular benefit.
5. Are certain populations more vulnerable to the cardiovascular consequences of sleep apnea?
Yes, certain groups face heightened risk from sleep apnea heart complications. Postmenopausal women, for example, may lose the cardioprotective benefits of estrogen and become more susceptible to both sleep apnea and heart disease. African American populations often experience higher rates of both sleep apnea and hypertension, leading to more pronounced sleep apnea heart problems. Additionally, individuals with diabetes or chronic kidney disease face compounded risks due to overlapping inflammatory and vascular mechanisms. Recognizing these vulnerabilities allows for targeted screening and early intervention in high-risk populations.
6. How does sleep apnea affect cardiac rehabilitation outcomes after a heart attack or surgery?
Sleep apnea can interfere with the body’s recovery processes after major cardiac events or surgeries. Poor oxygenation during sleep slows tissue repair, while sleep fragmentation impairs immune function and neurocognitive recovery. Many patients unknowingly continue to suffer from untreated sleep apnea postoperatively, which may increase their risk of recurrent heart events. In cardiac rehabilitation programs, addressing sleep apnea heart problems early on can enhance recovery, improve energy levels, and support long-term cardiac function. Integrating sleep studies into post-surgical care plans is becoming an increasingly accepted best practice.
7. What emerging technologies are helping detect sleep apnea-related heart risks more effectively?
Recent advancements in wearable technology and machine learning are opening new doors in sleep apnea and heart health monitoring. Devices like smartwatches and sleep trackers now offer pulse oximetry, heart rate variability data, and even real-time arrhythmia alerts. These tools can help identify early signs of sleep apnea heart problems before formal diagnosis. Meanwhile, artificial intelligence algorithms are being trained to detect abnormal sleep-breathing patterns using data from smartphones or contactless sensors. While these innovations don’t replace polysomnography, they offer promising adjuncts to broaden access to screening and early intervention.
8. Can improving sleep hygiene make a measurable difference in heart-related symptoms linked to sleep apnea?
Yes, optimizing sleep hygiene can reduce the severity of symptoms and complement other treatments. While sleep hygiene alone won’t eliminate apneic episodes, it can improve sleep architecture and decrease nighttime arousals. This results in fewer heart rate spikes and better autonomic regulation, which may reduce the intensity of sleep apnea heart problems. Strategies such as maintaining a consistent sleep schedule, limiting caffeine and alcohol, and creating a dark, quiet sleep environment help enhance restorative sleep quality. These practices are especially important for patients who are awaiting treatment initiation or struggling with CPAP adherence.
9. What role does altitude play in the severity of sleep apnea and its cardiac effects?
Higher altitudes can exacerbate both sleep apnea and its cardiovascular impacts due to lower ambient oxygen levels. At elevations above 5,000 feet, the body’s oxygen saturation naturally decreases, which can worsen hypoxic episodes during sleep. For individuals with existing sleep apnea heart conditions, this added stress may elevate blood pressure further and increase the risk of arrhythmias. Central sleep apnea is also more prevalent at altitude, particularly in those with underlying heart failure. Travelers or residents in mountainous areas with sleep apnea should be evaluated more closely, and sometimes may require altitude-adjusted CPAP settings or supplemental oxygen.
10. Is there a connection between gut health and sleep apnea-related heart risks?
Though still an emerging field, research into the gut microbiome suggests it may play a role in mediating the cardiovascular effects of sleep apnea. Intermittent hypoxia alters the composition of gut bacteria, leading to increased intestinal permeability and systemic inflammation. This inflammatory state is a known contributor to sleep apnea heart problems, compounding risks for atherosclerosis and metabolic syndrome. Additionally, disruptions in gut-derived neurotransmitters may influence sleep regulation and sympathetic tone. While more human studies are needed, the gut-heart-sleep axis is an exciting area of exploration that could yield novel therapies in the future.
Conclusion: Prioritizing Sleep for Cardiovascular Protection
The relationship between sleep apnea and heart health is no longer a medical curiosity—it is a critical area of clinical focus. As mounting research reveals, untreated sleep apnea heart problems can manifest as hypertension, arrhythmias, heart failure, and stroke. This breathing disorder acts not in isolation but as a systemic disruptor, affecting vascular function, autonomic regulation, and cardiac workload.
For individuals at risk, early recognition, timely diagnosis, and consistent treatment can significantly reduce cardiovascular morbidity and mortality. Sleep should be regarded not as a luxury but as a pillar of heart health, alongside diet, exercise, and medical therapy. Clinicians must remain vigilant in screening for sleep apnea in patients with heart disease, while individuals must be empowered to recognize symptoms and seek care.
Ultimately, breathing well during sleep is one of the most powerful—and often overlooked—ways to protect the heart. By addressing sleep apnea, we not only improve rest but also lay the foundation for a longer, healthier life free from many of the burdens associated with cardiovascular disease.
sleep-related cardiovascular risk, breathing disorders and heart disease, cardiovascular complications of poor sleep, obstructive sleep disorder effects, nocturnal oxygen desaturation, hypertension and sleep disorders, heart strain during sleep, arrhythmia and breathing issues, CPAP therapy benefits, chronic sleep disruption and health, cardiovascular consequences of apnea, low oxygen sleep risks, sleep-breathing connection, autonomic dysfunction and sleep, inflammatory response to apnea, cardiopulmonary sleep conditions, cardiac arrhythmias and sleep cycles, metabolic effects of poor sleep, endothelial dysfunction in sleep disorders, lifestyle strategies for better heart sleep health
Further Reading:
Sleep Apnea: Types, Mechanisms, and Clinical Cardiovascular Consequences
Sleep apnoea as an independent risk factor for cardiovascular disease
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.


