Understanding the Silent Signals of the Heart
The human heart is not just a muscular pump—it is a messenger of health, often giving subtle clues when something is amiss. Before a heart attack strikes, the body frequently tries to alert us. The question many ask is, how will your heart feel before a heart attack? The answer lies in decoding symptoms that are often dismissed, misunderstood, or mistaken for less severe issues. Recognizing these early warnings can mean the difference between timely intervention and irreversible damage. In this article, we will explore the physical sensations and emotional signals that may accompany an impending cardiac event, demystify what is a pre heart attack, and equip readers with evidence-based strategies for identifying and responding to early signs of cardiac distress.
You may also like: 5 Ways to Keep Your Heart Healthy and Prevent Cardiovascular Disease
Defining a Heart Attack and the Concept of a Pre Heart Attack
To understand how your heart might feel before a heart attack, it’s vital to grasp the physiological mechanics of a myocardial infarction. Commonly known as a heart attack, this occurs when blood flow to a part of the heart muscle is blocked, usually by a blood clot. This blockage leads to oxygen deprivation, resulting in damage or death to cardiac tissue. While many associate heart attacks with sudden, dramatic chest pain, the actual onset is often far more subtle.
What is a pre heart attack? The term refers to the period leading up to a heart attack, sometimes called unstable angina or a prodromal phase. During this time, plaque in the coronary arteries may become unstable or begin to rupture, triggering reduced blood flow but not yet causing permanent damage. The symptoms in this phase may wax and wane, presenting intermittently over hours, days, or even weeks. Though not every individual experiences a clearly defined pre heart attack period, those who do often describe it retrospectively as a time of strange or persistent discomfort that felt “off” but not alarming enough to seek immediate help.
The Sensory Experience: How Will Your Heart Feel Before a Heart Attack?
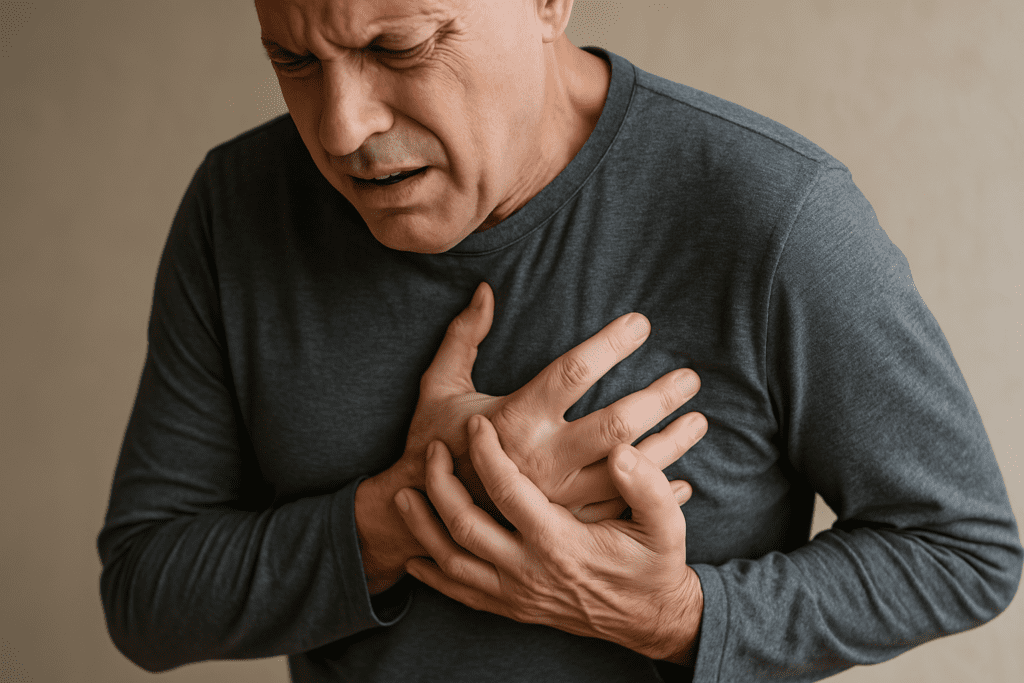
Before a full-blown cardiac event, people may notice unusual sensations that defy the stereotypical image of sudden, crushing chest pain. In fact, how your heart will feel before a heart attack often varies greatly depending on age, gender, and individual health conditions. For some, there is a heaviness or pressure in the chest—not sharp pain, but a sensation like a weight pressing down. This discomfort may come and go and is sometimes confused with indigestion, anxiety, or muscle strain.
Others report radiating pain that travels from the chest to the shoulders, arms, neck, jaw, or back. Women, in particular, are more likely to experience atypical symptoms such as fatigue, nausea, or shortness of breath without overt chest pain. Palpitations, lightheadedness, and cold sweats may also precede a cardiac event. Importantly, these feelings are not merely discomfort—they are distress signals that the heart is under strain.
Understanding how your heart feels before a heart attack also involves being attuned to changes in stamina, energy levels, and physical exertion tolerance. A sudden decline in your ability to perform routine activities—like climbing stairs or carrying groceries—can be a red flag. If your heart is laboring under reduced blood flow, you may feel a sense of impending doom or restlessness that doesn’t have an obvious cause. These experiences are your body’s attempt to communicate urgent dysfunction.
Unstable Angina: The Critical Clue in a Pre Heart Attack State
Unstable angina is often the clinical explanation behind the question, “What is a pre heart attack?” This condition involves chest pain or discomfort that occurs unpredictably, often at rest or with minimal exertion. Unlike stable angina, which follows a predictable pattern and typically resolves with rest or medication, unstable angina is erratic and may persist despite intervention. It is considered a medical emergency because it signifies that the coronary arteries are dangerously narrowed or intermittently blocked.
The pain from unstable angina may mimic a full heart attack but doesn’t cause permanent damage—yet. It’s a pivotal warning sign. Individuals experiencing this pre heart attack state may feel tightness in the center of the chest or a choking sensation in the throat. They may be awakened from sleep by discomfort or feel suddenly weak or dizzy during everyday tasks. Recognizing these symptoms and seeking immediate medical evaluation can prevent progression to a complete myocardial infarction.
Emotional and Psychological Signals of Cardiac Distress
Cardiac symptoms are not limited to the physical domain. Many individuals report psychological shifts in the days or hours before a heart attack. A heightened sense of anxiety, panic, or a vague feeling that something is wrong can precede a cardiac event. Though these symptoms are easy to attribute to stress or fatigue, they are sometimes an emotional reflection of physiological strain on the heart.
The body’s autonomic nervous system is closely tied to cardiac function, and distress in one often signals distress in the other. When people ask, “How will your heart feel before a heart attack?” they may not expect that the answer could involve dread, confusion, or emotional unease. These sensations are legitimate signs and should be taken seriously, particularly when paired with any form of chest discomfort or breathing difficulty.
Gender Differences in Pre Heart Attack Symptoms
One of the most critical dimensions of understanding what is a pre heart attack lies in recognizing how symptoms manifest differently between men and women. While men often experience the “classic” signs of chest pressure and left arm pain, women are more likely to report non-specific symptoms such as indigestion, extreme fatigue, or pain in the back and jaw. This divergence in symptom presentation contributes to delayed diagnosis and treatment in women, increasing their risk of complications.
A woman asking herself how her heart will feel before a heart attack might not immediately link her symptoms to cardiac issues. She may feel breathless after light activity, notice irregular heartbeats, or develop insomnia accompanied by inexplicable anxiety. Because these signs are less well-known and often overlap with benign conditions, women frequently downplay or ignore them until the situation becomes critical. Public health education must bridge this gender gap to ensure early intervention for all.

Recognizing Risk Factors That Increase Vulnerability
No discussion of how your heart will feel before a heart attack is complete without considering individual risk profiles. People with hypertension, diabetes, high cholesterol, obesity, or a family history of heart disease are at increased risk. Smoking, sedentary lifestyle, and chronic stress further compound these risks. In these individuals, even subtle symptoms can carry serious implications.
Understanding what is a pre heart attack in the context of risk factors allows for proactive monitoring. For example, a diabetic individual may have blunted pain perception, experiencing little or no chest discomfort even as ischemia progresses. In such cases, symptoms like unexplained fatigue, shortness of breath, or gastrointestinal distress become even more significant. Awareness of personal risk factors enhances the ability to interpret and respond to early signs appropriately.
Diagnostic Tools for Identifying a Pre Heart Attack
When individuals present with symptoms suggestive of a pre heart attack, healthcare professionals rely on a combination of clinical evaluation and diagnostic testing. Electrocardiograms (ECGs) are often the first step, revealing electrical abnormalities that may indicate ischemia. Blood tests such as troponin levels can detect even minor damage to heart muscle cells, supporting early diagnosis.
Stress testing, echocardiography, and coronary angiography provide additional insight, particularly when symptoms are intermittent or ambiguous. Advanced imaging techniques can reveal areas of reduced blood flow or blocked arteries before irreversible injury occurs. Identifying the pre heart attack phase through these tools allows for aggressive treatment, including medications, lifestyle changes, and possibly surgical interventions to restore blood flow and prevent future events.
What to Do If You Suspect You’re in a Pre Heart Attack State
If you’re experiencing symptoms and wondering how your heart might feel before a heart attack, the most crucial step is to take action—do not wait for symptoms to become unbearable. Call emergency services if you feel persistent chest discomfort, shortness of breath, lightheadedness, or any of the signs described earlier. Time is muscle, as cardiologists say: the sooner you receive care, the better your chances of full recovery.
Aspirin may help reduce clot formation and can be taken while awaiting medical help, but it should never replace professional evaluation. Avoid driving yourself to the hospital. Instead, alert someone nearby or call an ambulance. Once in a clinical setting, rapid assessment and intervention can stabilize your condition and prevent a minor episode from evolving into a full-scale heart attack.
Prevention: Listening to Your Heart Before It Cries Out
Preventing a heart attack begins long before the first symptom. It involves cultivating heart-healthy habits, understanding your risk factors, and paying close attention to bodily cues. Regular checkups, routine blood work, and open communication with your healthcare provider create a foundation for cardiovascular wellness.
Lifestyle interventions such as maintaining a balanced diet, engaging in regular physical activity, managing stress, and avoiding tobacco use have a profound impact. Additionally, understanding how your heart may feel before a heart attack empowers you to recognize early warnings. Being attuned to small changes in how your body responds to exertion, stress, and rest can help you act swiftly when necessary.
The Role of Patient Education in Reducing Heart Attack Mortality
Patient awareness and education play a central role in preventing death from heart attacks. Studies show that individuals who understand what is a pre heart attack and can identify early warning signs are more likely to seek timely medical attention, improving survival rates. Public health campaigns, clinician-patient conversations, and accessible online resources all contribute to this awareness.
Incorporating education about gender-specific symptoms, silent warning signs, and the variability of pre heart attack presentations is crucial. Equipping patients with knowledge demystifies the experience and removes the stigma or fear that might otherwise delay action. Ultimately, informed individuals are empowered individuals—capable of responding to their body’s messages with clarity and urgency.
Frequently Asked Questions: Early Signs of Cardiac Distress and Pre Heart Attack Awareness
1. Can emotional stress make it harder to recognize how your heart will feel before a heart attack?
Yes, emotional stress can blur the perception of early cardiac symptoms. When individuals are under chronic stress, they often normalize symptoms such as fatigue, tightness in the chest, or difficulty breathing—assuming these are merely psychological rather than physiological. This overlap can delay recognition of how your heart will feel before a heart attack, particularly when the sensations are subtle or intermittent. Psychological stress can also elevate cortisol and adrenaline levels, which may mask or intensify cardiovascular symptoms, making it harder to discern a true emergency. This complex interaction underscores the need for emotional self-awareness and stress management, especially in individuals with known cardiovascular risk factors.
2. How do night-time symptoms influence the identification of a pre heart attack?
Some individuals experience worsening cardiac symptoms during sleep or while lying down, which complicates recognition of what is a pre heart attack. Nocturnal angina, characterized by chest discomfort that awakens a person from sleep, can be mistakenly attributed to anxiety or gastrointestinal issues like acid reflux. However, disrupted sleep accompanied by chest heaviness, shortness of breath, or a racing heartbeat could be the body’s early signal of compromised cardiac function. These nighttime episodes should not be dismissed, particularly if they occur repeatedly or in conjunction with daytime fatigue. Keeping a log of symptoms and discussing them with a healthcare provider can lead to earlier detection of cardiovascular instability.
3. Can wearable health technology help detect how your heart will feel before a heart attack?
Yes, modern wearable devices—such as smartwatches and fitness bands—are becoming valuable tools in identifying irregularities that reflect how your heart may feel before a heart attack. Features like heart rate variability tracking, ECG monitoring, and sleep quality analysis can provide real-time insights into cardiac health. While these devices are not diagnostic, they can alert users to abnormal heart rhythms, elevated resting heart rates, or persistent fatigue—all potential signs of a pre heart attack. The key is not to rely solely on the device, but to use it as a complementary tool alongside professional medical advice. Increased consumer access to cardiac biometrics may revolutionize early detection strategies in the near future.
4. Why do some people feel flu-like symptoms before a heart attack?
Flu-like symptoms—such as fatigue, body aches, chills, and even mild nausea—can sometimes precede a cardiac event, especially in women. These signs often go unrecognized as indicators of how your heart will feel before a heart attack. Inflammation plays a major role in cardiovascular distress, and the immune response triggered during a pre heart attack phase may manifest similarly to that of a viral infection. These misleading symptoms can result in patients delaying care or misattributing their condition to non-cardiac causes. Understanding this overlap can empower patients to seek timely medical evaluation, particularly when such symptoms are accompanied by shortness of breath or chest discomfort.
5. What role does gut health play in how your heart might feel before a heart attack?
Recent research suggests that the gut-heart connection may influence how your heart will feel before a heart attack. Gut microbiota imbalances can contribute to systemic inflammation and metabolic dysfunction, both of which are linked to the progression of atherosclerosis. Some individuals report gastrointestinal symptoms—such as bloating, indigestion, or nausea—during the pre heart attack stage, especially when cardiac output is reduced. These symptoms are not purely digestive in origin but may reflect diminished blood flow to the abdominal organs. Greater public awareness of this physiological crossover could help reduce misdiagnosis and delay in seeking cardiac care.
6. How do medications for other conditions influence symptoms of a pre heart attack?
Many medications prescribed for unrelated conditions may mask or alter the symptoms of a pre heart attack. For instance, beta blockers used for anxiety or high blood pressure can blunt the heart’s stress response, muting the palpitations or elevated heart rate that might otherwise raise alarm. Similarly, pain relievers and anti-inflammatory drugs may dull the chest discomfort typically associated with how your heart will feel before a heart attack. Patients using these medications should remain vigilant about subtler cues such as breathlessness, dizziness, or unexplained fatigue. Open communication with a healthcare provider about all medications being used can aid in more accurate risk assessment.
7. Is it possible to experience symptoms of a pre heart attack without having blocked arteries?
Yes, not all pre heart attack symptoms stem from traditional plaque-based blockages. A condition known as coronary microvascular dysfunction affects the small vessels of the heart and can produce symptoms similar to those caused by major artery disease. In such cases, individuals may still describe how their heart will feel before a heart attack—experiencing pressure, tightness, or fatigue—even though standard angiography may not detect any obstruction. This form of cardiovascular distress is more common in women and often goes underdiagnosed due to limitations in conventional testing. Emerging imaging technologies and advanced diagnostics are improving detection of these subtle, yet serious, vascular changes.
8. How can people with limited healthcare access recognize what is a pre heart attack and act effectively?
For individuals without easy access to healthcare, education becomes the most vital tool for identifying what is a pre heart attack. Community health programs, mobile clinics, and digital health platforms can provide lifesaving knowledge about the early signs of cardiac distress. Simple tools like a symptom journal, blood pressure cuff, or community-based screenings can help detect meaningful changes in cardiovascular status. Learning how your heart will feel before a heart attack empowers individuals to make timely decisions—such as seeking emergency care or avoiding strenuous activity—even without immediate medical oversight. Grassroots efforts to expand health literacy are essential for bridging gaps in cardiac care access.
9. Are there cultural differences in how people describe heart attack symptoms?
Absolutely. Cultural background can shape how individuals interpret and describe how their heart will feel before a heart attack. Some cultures may use metaphors or localized terms—like “bad wind” or “heartburn of the soul”—to describe pressure, tightness, or fatigue, which can obscure clinical interpretation. Additionally, cultural beliefs about stoicism or mistrust of medical systems can lead to delayed reporting of symptoms. Recognizing these nuances is crucial for healthcare providers aiming to deliver culturally competent care and improve outcomes. Encouraging open, respectful communication can help bridge the gap between patient expression and accurate diagnosis.
10. What lifestyle changes can sharpen your awareness of how your heart feels before a heart attack?
Enhancing body awareness through mindfulness, regular exercise, and journaling can significantly improve one’s ability to detect how the heart feels before a heart attack. Practices such as yoga or tai chi cultivate attention to breath and bodily sensations, helping individuals notice subtle shifts in energy or heart rate. Regular cardiovascular activity—when done safely—can also establish a baseline for what feels normal, making it easier to spot deviations during a pre heart attack state. Additionally, keeping a log of physical and emotional fluctuations over time can reveal patterns that might otherwise go unnoticed. Empowering people to listen to their own physiology is a powerful form of preventive medicine.
Conclusion: Listening to the Heart’s Early Warnings Could Save Your Life
Knowing how your heart will feel before a heart attack is not just an exercise in curiosity—it’s a potentially lifesaving insight. These sensations, though subtle or atypical, often carry critical meaning. By understanding what is a pre heart attack and how symptoms might present differently based on personal risk factors, age, and gender, individuals can intervene early, seeking care before permanent damage occurs.
The journey to better cardiovascular health begins with awareness. When the heart speaks in whispers—through fatigue, discomfort, breathlessness, or anxiety—it is asking to be heard. Ignoring those whispers can lead to tragedy; responding to them can alter the course of a life. Let this knowledge serve as both shield and compass, guiding you toward informed, proactive care and a heart that beats strong for years to come.
early warning signs of heart attack, cardiac event symptoms, heart disease awareness, chest discomfort causes, silent heart attack signs, women and heart disease, unstable angina symptoms, heart attack prevention tips, cardiovascular emergency signs, symptoms of poor circulation, heart health monitoring, subtle signs of heart trouble, prodromal heart attack symptoms, early signs of myocardial infarction, cardiac risk factors, stress and heart health, fatigue and heart problems, recognizing heart distress, warning signs before a heart attack, psychological signs of heart issues
Further Reading:
How to recognize the signs of a heart attack and what to do
Early Warning Signs of a Heart Attack
Warning Signs of a Heart Attack
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.