What New Research Reveals About Tirzepatide for Diabetes: Can It Lower Blood Sugar Without Acting Like Insulin?
In the evolving landscape of diabetes treatment, tirzepatide has emerged as a novel contender, sparking considerable interest among researchers and clinicians alike. With rising global concerns about type 2 diabetes and prediabetes, particularly as rates continue to climb among adults and younger populations, the arrival of innovative therapies is both timely and necessary. Tirzepatide, a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist, represents a significant step forward in how we approach blood sugar management. While traditional diabetes medications often target insulin production directly, tirzepatide’s mechanism appears distinct, leading many to ask: does tirzepatide lower blood sugar without acting like insulin?
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
As the body of evidence grows, medical professionals are beginning to grasp the scope of tirzepatide for diabetes treatment. This article will explore what current research reveals about tirzepatide, how it compares to existing therapies, its relevance in prediabetes management, and the implications of its unique pharmacological action. By analyzing scientific findings, clinical trials, and expert insights, we aim to answer key questions about tirzepatide’s role in managing glycemic control, its risks, and its potential to redefine how we approach type 2 diabetes.
Understanding Tirzepatide’s Dual Action Mechanism
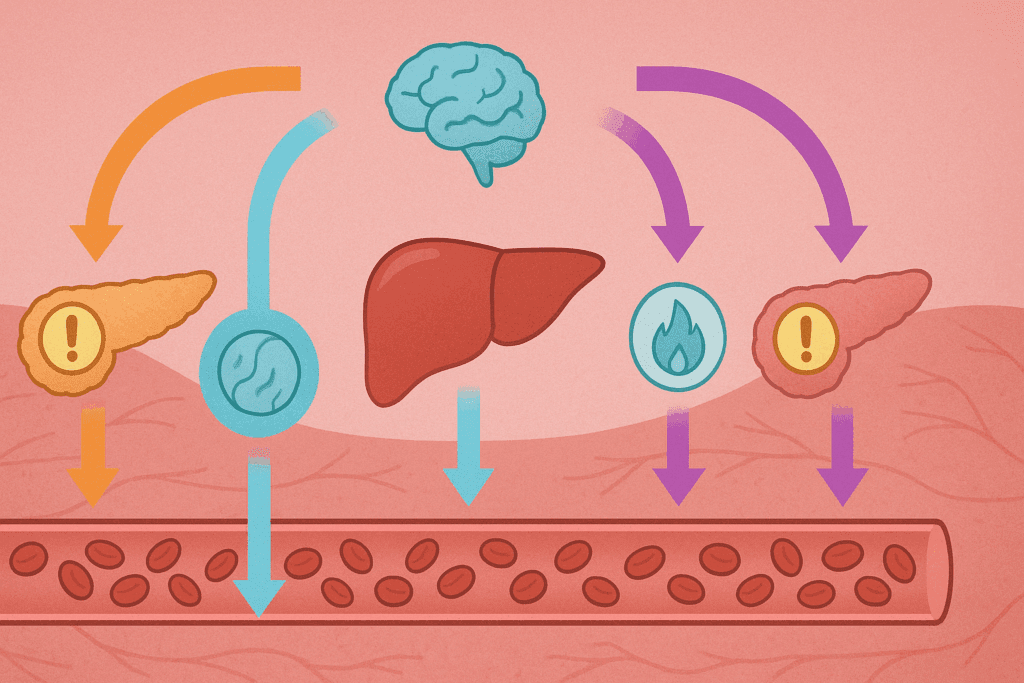
Tirzepatide’s uniqueness lies in its dual agonist mechanism, which activates both GIP and GLP-1 receptors. This combination allows for greater efficacy in lowering blood glucose compared to therapies that stimulate only GLP-1. Rather than functioning as synthetic insulin or prompting the pancreas to release excessive amounts of insulin, tirzepatide works by enhancing the body’s own hormonal responses to glucose intake. This means that while it improves insulin sensitivity and stimulates insulin secretion when needed, it does not mimic insulin in the traditional sense, leading many to ask: is tirzepatide insulin, or something entirely different? The distinction matters, especially for patients who struggle with insulin-related side effects or who are insulin-resistant.
Clinical trials have shown that tirzepatide improves beta-cell function and reduces insulin resistance, particularly in individuals with type 2 diabetes. Moreover, because it modulates appetite and delays gastric emptying, tirzepatide contributes to weight loss, a critical component in managing diabetes. Unlike direct insulin injections that can promote weight gain, tirzepatide tends to have the opposite effect, which further enhances glycemic control. This multifaceted mechanism is particularly promising for individuals with prediabetes, where early intervention can prevent the progression to full-blown diabetes.
Recent Trials Confirm Tirzepatide Lowers Blood Sugar
Several high-profile clinical studies have established that tirzepatide significantly lowers blood glucose levels. In the SURPASS trials, for instance, tirzepatide outperformed semaglutide, another GLP-1 receptor agonist, in reducing hemoglobin A1c (HbA1c) levels. Participants treated with tirzepatide experienced reductions in HbA1c levels ranging from 1.87% to 2.07%, depending on the dosage. These findings demonstrate that tirzepatide for diabetes management offers robust efficacy, often exceeding the performance of comparable agents.
Importantly, these reductions occurred without the drug functioning like traditional insulin. The implications are profound. For patients who require tighter glucose control but are hesitant to begin insulin therapy due to the fear of injections, weight gain, or hypoglycemia, tirzepatide offers an effective alternative. This distinction further clarifies why the question “does tirzepatide lower blood sugar” is so relevant in current clinical discussions. It certainly does—but through a pathway that is arguably safer and more physiologically aligned with the body’s natural processes.
The Role of Tirzepatide in Prediabetes and Early Intervention
Prediabetes, often overlooked or underestimated, is a critical stage where intervention can drastically reduce the risk of developing type 2 diabetes. The emergence of treatments like tirzepatide provides new hope for individuals in this early phase. Recent studies are beginning to explore the use of Mounjaro (tirzepatide’s brand name) in prediabetic populations. In what is becoming a popular clinical discussion, the term “prediabetes Mounjaro” is increasingly searched by both patients and practitioners seeking early intervention strategies.
Preliminary findings suggest that tirzepatide may help restore normoglycemia in individuals with prediabetes, especially when combined with lifestyle changes. Weight loss plays a crucial role in this process, and tirzepatide has been shown to induce substantial reductions in body weight—sometimes exceeding 10-15% of baseline body mass. This dual effect of lowering both blood sugar and weight offers a comprehensive approach that is particularly appealing in preventive medicine.
Addressing the Risk of Low Blood Sugar with Tirzepatide
One of the central concerns for any diabetes treatment is the potential for hypoglycemia, or low blood sugar. Understandably, patients and providers frequently ask: can tirzepatide cause low blood sugar, and how does this risk compare to other treatments? According to current evidence, tirzepatide carries a relatively low risk of hypoglycemia, particularly when used as monotherapy or in combination with medications that do not independently lower glucose levels.
However, when tirzepatide is used alongside sulfonylureas or insulin, the risk of hypoglycemia can increase. This underscores the importance of careful medication management and individualized treatment planning. Nevertheless, compared to traditional insulin therapy, the incidence of tirzepatide low blood sugar events is notably lower. Its glucose-dependent mechanism ensures that insulin secretion only occurs when glucose levels are elevated, reducing the risk of overshooting into hypoglycemic territory.
Tirzepatide’s Impact on Weight and Cardiometabolic Health
Beyond glycemic control, tirzepatide has demonstrated remarkable effects on weight reduction and cardiometabolic risk factors. Obesity is a known contributor to insulin resistance, and losing weight can significantly enhance insulin sensitivity. Tirzepatide’s ability to facilitate weight loss while simultaneously improving glycemic control makes it a compelling choice in the broader management of type 2 diabetes and prediabetes.
In the SURMOUNT trials, participants experienced weight reductions comparable to those seen with bariatric surgery, especially when higher doses of tirzepatide were used. The resulting improvements in blood pressure, lipid profiles, and markers of inflammation further illustrate the systemic benefits of this therapy. Thus, while many continue to wonder, “does tirzepatide lower blood sugar,” the broader question may be: what else can it improve in the metabolic health equation?
How Tirzepatide Differs from Insulin and GLP-1 Agonists
Although both GLP-1 receptor agonists and insulin have long histories in diabetes care, tirzepatide introduces a new paradigm. Unlike insulin, which provides exogenous hormone replacement, tirzepatide enhances endogenous mechanisms already present in the body. This internal regulation creates a smoother, more physiological blood sugar response. Compared to GLP-1 agonists alone, tirzepatide’s dual receptor activity provides a more pronounced effect on glucose metabolism and appetite suppression.
Because of its distinct pharmacological profile, tirzepatide offers advantages in reducing not only fasting blood glucose but also postprandial spikes, which are critical in long-term glycemic control. These unique features contribute to the ongoing debate around “is tirzepatide insulin”—a question that has a clear answer: no. It is not insulin, nor does it act in a similar manner. Instead, it may represent the next evolution of incretin-based therapies, offering a novel and effective way to control diabetes without the burden associated with insulin injections.

Ongoing Research and Future Directions
The scientific community remains actively engaged in studying tirzepatide’s full potential. Ongoing research is investigating its long-term cardiovascular outcomes, durability of weight loss, and its role in preserving pancreatic beta-cell function. Given the growing interest in preventing type 2 diabetes, studies are increasingly focusing on the prediabetes population and the potential for tirzepatide to reverse early glycemic abnormalities before they progress.
Emerging data also explore how tirzepatide might interact with other chronic conditions common in people with diabetes, such as non-alcoholic fatty liver disease (NAFLD) and polycystic ovary syndrome (PCOS). These investigations are expanding the drug’s relevance well beyond blood sugar control, indicating that its benefits may reach into broader areas of metabolic dysfunction. In this way, the phrase “tirzepatide for diabetes” may soon become a misnomer, as its utility extends to a wider range of endocrine and cardiometabolic disorders.
Patient Considerations and Clinical Decision-Making
While the evidence supporting tirzepatide is compelling, clinical decision-making must still be individualized. Not every patient will be an ideal candidate, and factors such as kidney function, gastrointestinal tolerance, and medication costs must be considered. For those in the early stages of disease or struggling with weight management, tirzepatide offers a promising alternative to traditional therapies.
Clinicians should evaluate whether the benefits—such as reduced HbA1c, weight loss, and low risk of hypoglycemia—outweigh any potential side effects or financial burdens. Discussions around “prediabetes Mounjaro” are particularly important in primary care, where early interventions can produce lifelong benefits. Patient education plays a vital role in ensuring compliance and successful outcomes, especially when new medications challenge conventional understanding.
Clarifying Misconceptions: Tirzepatide Is Not a Form of Insulin
Despite its impressive glycemic effects, tirzepatide should not be mistaken for insulin. The persistent query “is tirzepatide insulin” reflects a broader need for public education about how modern medications work. While insulin therapy replaces a hormone that the pancreas is no longer able to produce in sufficient amounts, tirzepatide enhances the body’s ability to regulate glucose through its own hormonal pathways.
This clarification is critical, especially for patients who fear insulin initiation or believe that their treatment signals a worsening of disease. The availability of agents like tirzepatide redefines that narrative, showing that high-level glucose control can be achieved without jumping directly to insulin therapy. It also alleviates concerns around hypoglycemia, as tirzepatide low blood sugar risks remain minimal under most regimens. Understanding these differences allows patients and providers to make informed, confident treatment choices.
Practical Implications for Healthcare Providers
For healthcare professionals, the emergence of tirzepatide signals a shift in therapeutic strategies. With strong efficacy in both glycemic control and weight reduction, it becomes an attractive option not only for endocrinologists but also for primary care physicians managing a growing population of patients with metabolic syndrome. Incorporating tirzepatide into treatment algorithms requires a thorough understanding of its mechanism and patient eligibility criteria.
Providers should also be prepared to address common concerns such as “can tirzepatide cause low blood sugar” and whether it acts like insulin. Accurate, evidence-based communication is essential for helping patients navigate their treatment choices. As more data emerges and real-world usage grows, providers will gain better insights into how tirzepatide performs outside of controlled clinical environments. This will further refine best practices and help establish its role in long-term diabetes care.
Why Tirzepatide Represents a New Era in Diabetes Care
The significance of tirzepatide cannot be overstated. It represents not just another medication but a paradigm shift in how diabetes may be treated going forward. Its ability to lower blood sugar without acting like insulin challenges long-held assumptions about the progression of diabetes and the necessity of insulin therapy at certain stages. With its dual-action mechanism, impressive clinical outcomes, and favorable safety profile, tirzepatide is carving out a unique and important place in the diabetes treatment landscape.
Patients, particularly those with newly diagnosed type 2 diabetes or with prediabetes, stand to benefit the most from this innovative approach. As research continues to validate its long-term safety and effectiveness, tirzepatide could become a foundational element of metabolic disease management. Its dual focus on glycemic control and weight reduction makes it a versatile tool in combating a condition that remains a leading cause of morbidity and mortality worldwide.
Frequently Asked Questions (FAQ): Expert Insights on Tirzepatide and Blood Sugar Management
1. How does tirzepatide affect long-term blood sugar stability beyond initial treatment?
Tirzepatide for diabetes has shown promising results not just in immediate blood glucose control but also in promoting long-term glycemic stability through sustained action on multiple metabolic pathways. Its dual agonist mechanism influences both insulin secretion and glucagon suppression, helping to reduce postprandial glucose spikes and fasting glucose levels consistently. Unlike some other medications, tirzepatide appears to “retrain” pancreatic beta-cell responsiveness over time, potentially improving endogenous insulin function. This means that even after months of use, patients may experience more predictable glucose fluctuations, which is essential in managing chronic conditions like type 2 diabetes. For those wondering, does tirzepatide lower blood sugar long-term—the answer is yes, with the added benefit of supporting metabolic equilibrium over extended periods.
2. Can tirzepatide be effective for individuals with prediabetes, or is it strictly for diagnosed diabetes?
Although tirzepatide is officially approved for managing type 2 diabetes, emerging evidence suggests it may be beneficial for people with prediabetes as well. In fact, many clinicians are now exploring prediabetes Mounjaro use off-label, especially for high-risk individuals with obesity and insulin resistance. Its ability to improve insulin sensitivity, lower fasting glucose, and aid in weight loss creates a metabolic environment less conducive to diabetes progression. While lifestyle changes remain the first-line intervention for prediabetes, adding tirzepatide might delay or even prevent full-blown diabetes when used judiciously under medical supervision. It’s essential to consult an endocrinologist before initiating treatment, but the proactive use of tirzepatide in prediabetes is an area of growing interest in preventative endocrinology.
3. Is tirzepatide a form of insulin or does it work differently?
Many patients wonder, is tirzepatide insulin? The answer is no—tirzepatide is not insulin. It belongs to a class of drugs called dual GIP and GLP-1 receptor agonists. Unlike insulin, which directly lowers blood sugar by facilitating glucose uptake, tirzepatide enhances the body’s own insulin response only when blood sugar levels are elevated. This targeted action reduces the risk of hypoglycemia compared to exogenous insulin therapy. It also slows gastric emptying and promotes satiety, offering metabolic benefits that insulin does not provide. Understanding the distinction between the two helps patients make informed decisions about their diabetes treatment options.
4. What should patients know about the risk of low blood sugar when taking tirzepatide?
Though tirzepatide is less likely than insulin or sulfonylureas to cause hypoglycemia, it’s still possible under certain conditions. For instance, can tirzepatide cause low blood sugar? Yes—but primarily when used in combination with other glucose-lowering agents or during periods of calorie restriction. People on tirzepatide who fast, skip meals, or engage in intense physical activity without adjusting their dosing may experience symptoms of hypoglycemia. These can include sweating, dizziness, shakiness, and confusion. Patients using tirzepatide should be educated on recognizing tirzepatide low blood sugar symptoms and carry quick sources of glucose for emergencies.
5. How does tirzepatide compare with GLP-1 monotherapy in terms of blood sugar control?
Tirzepatide for diabetes is often compared to GLP-1 receptor agonists such as semaglutide, and current evidence shows that it generally leads to superior A1C reductions. Its dual mechanism—activating both GIP and GLP-1 receptors—enhances insulin secretion while also suppressing glucagon more effectively. This duality allows for more nuanced and potent blood glucose regulation across various meal types and times of day. For those asking, does tirzepatide lower blood sugar better than GLP-1-only drugs, the answer appears to be yes, especially for patients with significant insulin resistance or higher baseline A1C levels. Clinical trials like SURPASS have confirmed these findings, making tirzepatide a powerful tool in modern diabetes management.
6. Are there unique psychological effects associated with tirzepatide treatment?
One underexplored but clinically relevant aspect of tirzepatide treatment is its psychological impact. Patients who previously struggled with uncontrolled blood glucose often report improved mood, increased energy, and reduced anxiety once their levels stabilize with tirzepatide. The question can tirzepatide cause low blood sugar can be anxiety-inducing for some, particularly those with a history of hypoglycemia, but education and careful dosing can alleviate these concerns. Furthermore, the weight loss commonly seen with tirzepatide often improves body image and self-esteem, which are crucial factors in chronic disease self-management. These psychological benefits may enhance adherence, making the medication’s success partly behavioral as well as physiological.
7. What are some real-world use cases of tirzepatide in prediabetes management?
Outside clinical trials, practitioners are using prediabetes Mounjaro therapy in innovative ways. For example, in weight loss clinics, tirzepatide is being paired with intensive lifestyle interventions for patients with metabolic syndrome and prediabetes. These individuals often show significant improvements in fasting glucose and insulin sensitivity within weeks. In some cases, they even revert to normoglycemia—meaning their blood sugar returns to normal, non-prediabetic levels. While FDA approval is pending for this indication, real-world use cases are shaping how providers approach metabolic prevention with tirzepatide for diabetes and prediabetes alike.
8. How can patients avoid low blood sugar episodes while using tirzepatide?
To prevent tirzepatide low blood sugar events, patients should be mindful of their overall treatment regimen. Combining tirzepatide with insulin or sulfonylureas raises the risk, so dose adjustments may be necessary. Also, patients should maintain consistent meal patterns and monitor blood sugar closely during times of dietary change or increased physical activity. Knowing the answer to can tirzepatide cause low blood sugar prepares patients to recognize early signs like fatigue and trembling before a severe episode occurs. Informed, proactive patients can often use tirzepatide safely without major disruptions to daily life.
9. What future developments are expected for tirzepatide in metabolic health?
Looking ahead, tirzepatide may play a role far beyond diabetes. Researchers are studying its use in prediabetes Mounjaro protocols, as well as its potential benefits for cardiovascular and renal outcomes. There is growing interest in how tirzepatide for diabetes could evolve into a cornerstone therapy for metabolic syndrome, addressing hypertension, dyslipidemia, and inflammation alongside blood sugar control. Advanced formulations may extend its dosing interval or reduce gastrointestinal side effects. As studies continue to answer does tirzepatide lower blood sugar under varied conditions, its role in integrated metabolic care is poised to expand significantly.
10. How does tirzepatide fit into a comprehensive diabetes management plan?
Tirzepatide is not a stand-alone solution but works best when integrated into a broader care strategy that includes diet, physical activity, stress management, and regular monitoring. While tirzepatide for diabetes can drastically improve glucose control, long-term outcomes depend on patient engagement and lifestyle habits. Providers must still educate patients about nutrition, the importance of sleep, and how to interpret blood sugar trends. Addressing concerns like is tirzepatide insulin or can tirzepatide cause low blood sugar also helps build trust and ensure proper usage. Ultimately, when used as part of a personalized, holistic plan, tirzepatide can significantly improve both metabolic health and quality of life.
Conclusion: Tirzepatide for Diabetes—A Promising Breakthrough That Lowers Blood Sugar Without Being Insulin
In reviewing the latest scientific findings, it is clear that tirzepatide for diabetes offers a compelling combination of efficacy, safety, and innovation. It addresses the pressing question that many are asking—does tirzepatide lower blood sugar—by providing an unequivocal yes, supported by rigorous clinical data. Yet it does so without acting like insulin, which marks a significant advancement in diabetes therapy.
Patients and clinicians alike can be reassured by the evidence indicating that tirzepatide not only improves glycemic control but also contributes to meaningful weight loss and reduced cardiometabolic risk. While concerns remain regarding the potential for low blood sugar, particularly in combination therapies, the overall safety profile is favorable. As terms like “tirzepatide low blood sugar” and “prediabetes Mounjaro” become more familiar in clinical discussions and patient education, they underscore a growing awareness of this therapy’s expansive potential.
As our understanding of tirzepatide continues to deepen, it’s likely to play an increasingly central role in the treatment of both diabetes and prediabetes. The dual benefits it offers—controlling blood sugar and addressing obesity—align perfectly with modern approaches to chronic disease management. In this way, tirzepatide is not only answering today’s clinical questions but also shaping the future of metabolic health.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Tirzepatide outperforms insulin in controlling diabetes and promoting weight loss in clinical trials
Perspectives on weight control in diabetes – Tirzepatide
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.