Understanding the Emerging Link Between Pancreatitis and Diabetes
In recent years, the complex relationship between pancreatitis and diabetes has garnered increasing attention from researchers, clinicians, and public health professionals. While historically considered distinct conditions, new evidence suggests a significant overlap between the two. This intersection raises a fundamental question: does pancreatitis cause diabetes, or is it merely a signal of broader pancreatic dysfunction affecting blood sugar regulation? Understanding this connection is not merely academic—it has direct implications for diagnosis, prevention, and patient management.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
The pancreas serves critical roles in both digestion and glucose metabolism. When inflammation occurs, as seen in pancreatitis, these functions can be disrupted in ways that contribute to or mimic diabetic pathophysiology. Patients recovering from acute or chronic pancreatitis often experience changes in glucose tolerance, and some ultimately develop diabetes as a result. This specific form, often referred to as pancreatic diabetes or type 3c diabetes, has unique characteristics that distinguish it from traditional type 1 or type 2 diabetes. Consequently, understanding the nature of this overlap is essential for timely and appropriate medical care.
Pancreatic Physiology and Blood Sugar Regulation
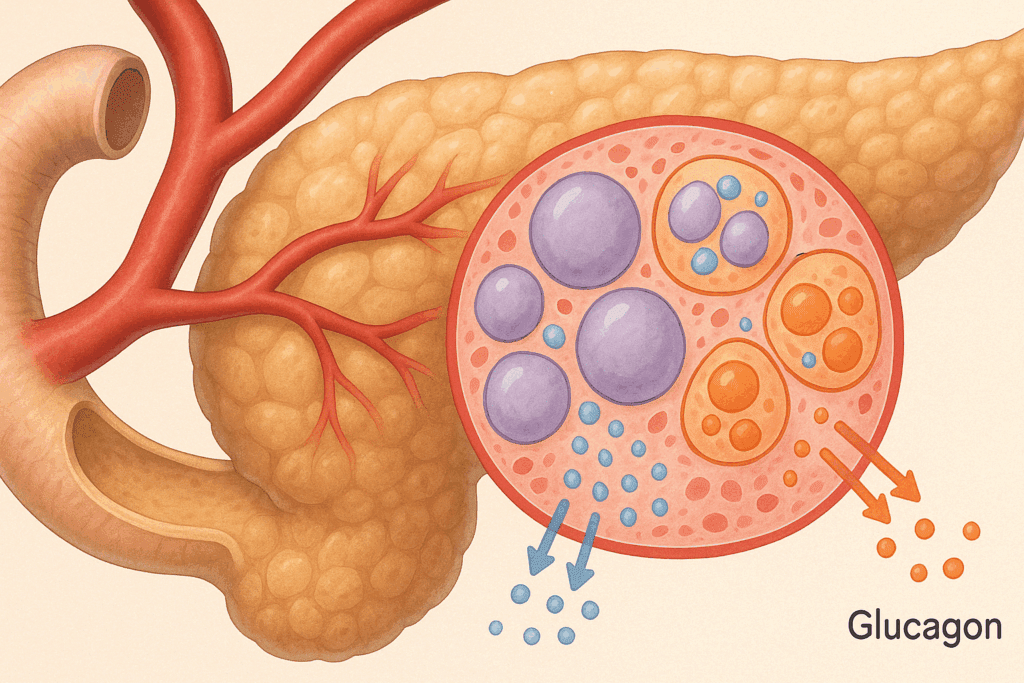
To grasp the link between pancreatitis and diabetes, one must first appreciate the pancreas’s role in regulating glucose. The pancreas houses the islets of Langerhans, clusters of cells that produce insulin, glucagon, and other hormones crucial to maintaining blood sugar balance. Insulin, secreted by beta cells, lowers blood glucose by facilitating its uptake into tissues, while glucagon raises it by stimulating glycogen breakdown in the liver. This hormonal interplay keeps blood sugar levels within a narrow, healthy range.
When the pancreas becomes inflamed, as in pancreatitis, the damage is not limited to the digestive enzyme-producing exocrine tissue. The endocrine cells responsible for hormonal control can also be injured or destroyed. In chronic cases, this damage can be progressive, leading to long-term impairment of insulin production. As a result, the pancreas and blood sugar balance become increasingly difficult to maintain, and hyperglycemia may develop. This dysfunction is more than a side effect—it may be the early warning sign of a new, complex diabetic subtype.
Does Pancreatitis Cause Diabetes or Reveal Hidden Vulnerability?
The key question—does pancreatitis cause diabetes—has no singular answer. Research suggests that the relationship is multifactorial and depends on the type, severity, and recurrence of pancreatic inflammation. Acute pancreatitis may cause temporary insulin resistance or reduced insulin output, but in many cases, glucose metabolism returns to normal after recovery. In contrast, chronic pancreatitis is associated with irreversible damage to pancreatic tissue, including the hormone-secreting islets, which significantly increases the likelihood of developing long-term diabetes.
In some patients, diabetes following pancreatitis may emerge even in the absence of traditional risk factors like obesity or family history. This observation has led researchers to investigate whether pancreatitis uncovers a latent susceptibility to endocrine dysfunction. Genetic predisposition, environmental toxins, and metabolic stressors may all play a role in weakening pancreatic resilience. Thus, while pancreatitis may not directly cause diabetes in every instance, it often serves as a catalyst that accelerates existing vulnerabilities in pancreatic function and blood sugar control.
Defining Pancreatic Diabetes as a Distinct Clinical Entity
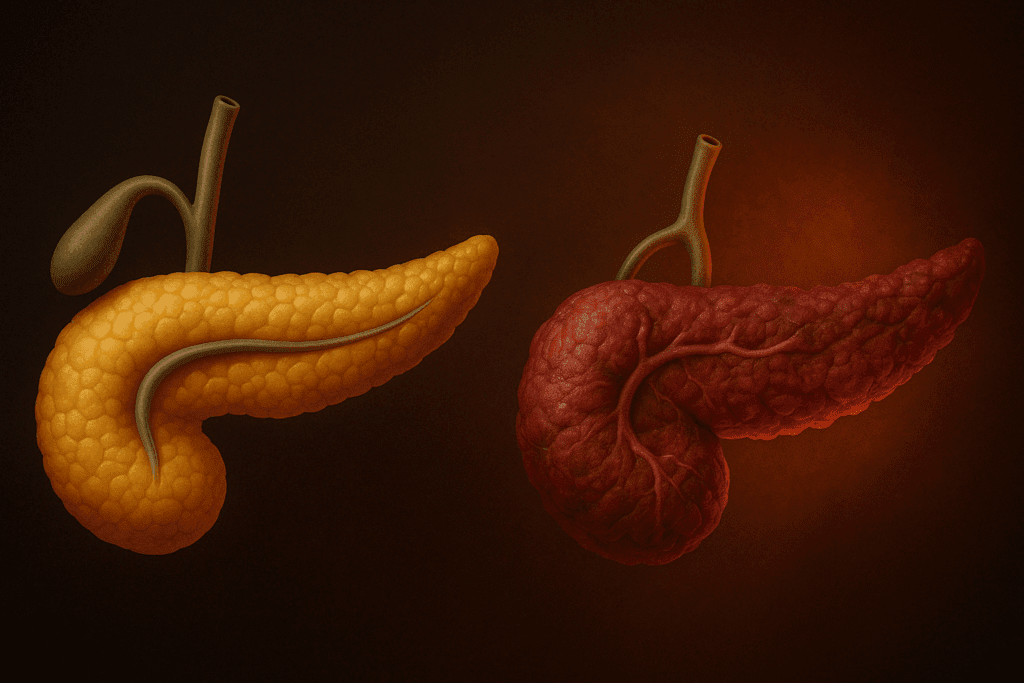
As more cases of post-pancreatitis diabetes are documented, clinicians are recognizing pancreas diabetes—also termed type 3c diabetes—as a clinically unique condition. Unlike type 1 diabetes, which results from autoimmune destruction of beta cells, or type 2 diabetes, which is typically associated with insulin resistance, pancreatic diabetes arises from direct damage to the pancreas due to inflammation, surgery, trauma, or tumor. Patients with pancreatic diabetes may exhibit features of both insulin deficiency and insulin resistance, often accompanied by digestive disturbances from exocrine insufficiency.
Diagnosis can be challenging, as pancreatic diabetes is frequently misclassified as type 2 diabetes. However, there are key differences that clinicians must recognize. Individuals with pancreatic diabetes often have a history of pancreatitis, unexplained weight loss, steatorrhea (fatty stools), and a need for pancreatic enzyme replacement therapy. Their insulin requirements can be unpredictable, and they may be more prone to hypoglycemia due to impaired glucagon secretion. Recognizing these patterns is essential for delivering effective care and preventing complications.
New Research Supporting the Diabetes-Pancreatitis Link
Recent studies have provided robust evidence supporting the link between pancreatitis and diabetes. A large cohort study published in The Lancet examined over 120,000 patients and found a substantially increased incidence of diabetes among those who had experienced acute or chronic pancreatitis. The risk persisted for several years after the initial pancreatic event, suggesting a lasting impact on endocrine function. These findings were independent of traditional diabetes risk factors, underscoring the unique pathophysiology involved.
Further research has explored the biological mechanisms underlying this association. Chronic inflammation in the pancreas can lead to fibrosis, calcification, and destruction of islet cells. Proinflammatory cytokines released during pancreatitis episodes can impair beta-cell function or trigger their apoptosis. These mechanisms reduce the pancreas’s ability to regulate blood sugar, shifting the metabolic equilibrium toward a diabetic state. This accumulating evidence supports the assertion that pancreatic injury is a potent contributor to diabetes development.
The Role of the Gut-Pancreas Axis in Metabolic Regulation
An emerging area of interest in understanding pancreas diabetes is the interaction between the gut microbiome and the pancreas. Researchers have discovered that imbalances in gut flora, commonly observed in patients with pancreatitis, may influence metabolic processes and exacerbate inflammation. Certain bacterial species can trigger immune responses that further damage pancreatic tissue, while others may play a protective role.
Moreover, disruptions in the gut-brain-pancreas axis can alter appetite regulation, insulin sensitivity, and nutrient absorption. For example, short-chain fatty acids produced by gut bacteria affect insulin secretion and glucose utilization. These findings point to a broader, systemic network in which the pancreas and blood sugar metabolism are intimately tied to digestive and microbial health. Understanding this axis opens new doors for therapeutic interventions that go beyond traditional insulin-focused strategies.
Implications for Diagnosis and Patient Monitoring
Given the growing recognition of pancreatic diabetes, there is an urgent need to refine diagnostic protocols. Current diabetes classification systems do not adequately account for cases resulting from pancreatic injury. Patients with a history of pancreatitis should undergo more frequent and comprehensive glucose monitoring, especially in the years following acute episodes. Oral glucose tolerance tests, hemoglobin A1c levels, and fasting glucose tests should be supplemented with pancreatic imaging and enzyme level assessments.
Early identification of glucose abnormalities allows for timely intervention, potentially slowing or preventing the transition to full-blown diabetes. Clinicians must be trained to recognize atypical diabetes presentations and to consider pancreas diabetes in patients with both metabolic and digestive symptoms. Multidisciplinary collaboration between endocrinologists, gastroenterologists, and primary care providers is essential for holistic patient care.
Treatment Strategies for Pancreatic Diabetes
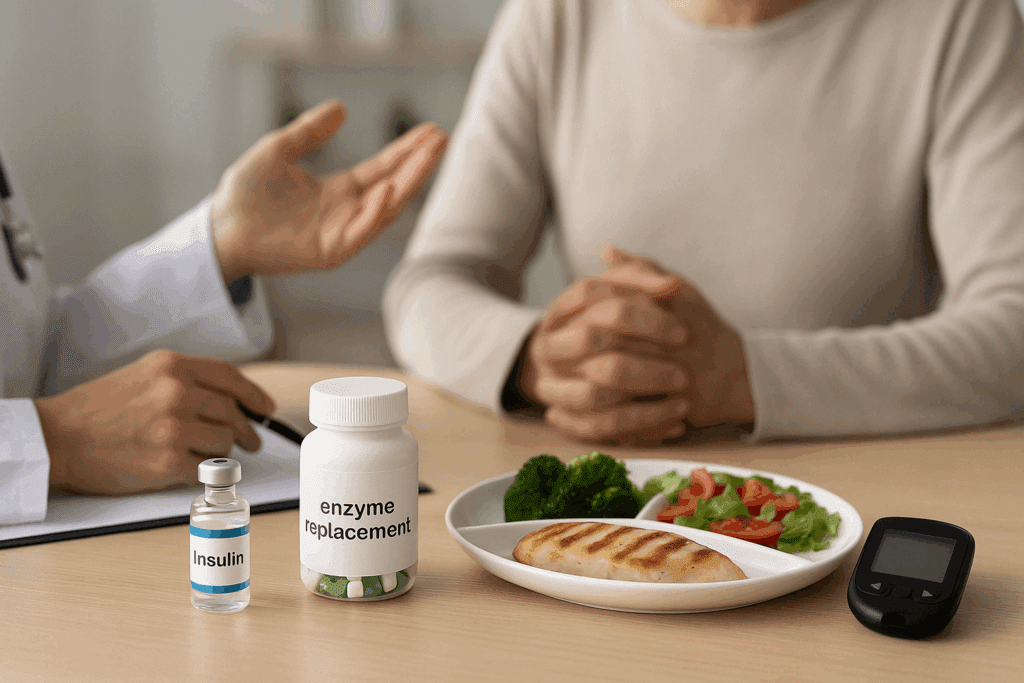
Managing pancreatic diabetes requires an individualized and multifaceted approach. Unlike standard type 2 diabetes, where oral medications and lifestyle modifications are often effective, pancreatic diabetes may necessitate both insulin therapy and enzyme replacement. Blood sugar management is complicated by the variability in insulin secretion and the impaired glucagon response to hypoglycemia. As such, patients must be carefully educated on how to recognize and respond to low blood sugar events.
Dietary interventions also play a critical role. Nutritional strategies should focus on balanced meals that support both glycemic control and digestive health. Patients may benefit from small, frequent meals that are low in fat and high in complex carbohydrates and protein. Supplementation with fat-soluble vitamins (A, D, E, and K) may be necessary due to malabsorption. These considerations highlight the importance of personalized nutrition plans in the long-term management of pancreas diabetes.
Preventing Diabetes After Pancreatitis: Is It Possible?
While not all cases of diabetes after pancreatitis can be prevented, emerging research suggests that proactive strategies can reduce risk. Avoiding known triggers of pancreatitis—such as excessive alcohol consumption, gallstones, high triglyceride levels, and certain medications—can minimize pancreatic injury. For individuals with recurrent pancreatitis or genetic predispositions, regular follow-ups and lifestyle modifications are crucial.
In patients who have already experienced pancreatitis, early intervention may involve anti-inflammatory medications, antioxidants, or lifestyle therapies aimed at preserving pancreatic function. Managing comorbid conditions like obesity, hypertension, and dyslipidemia also reduces metabolic stress on the pancreas. These prevention-focused approaches are grounded in a deeper understanding of how the pancreas and blood sugar systems are dynamically connected.
Psychological and Quality-of-Life Considerations
Living with both pancreatitis and diabetes imposes a substantial psychological burden. The daily challenges of managing digestive symptoms, fluctuating blood sugar, and dietary restrictions can lead to anxiety, depression, and social withdrawal. Mental health support should be integrated into the care model for individuals with pancreatic diabetes to improve adherence and long-term outcomes.
Patients may benefit from counseling, support groups, and educational programs that empower them to manage their conditions more effectively. Incorporating behavioral health into routine care not only enhances psychological well-being but also supports better glycemic control. Recognizing the emotional toll of this dual diagnosis is a critical aspect of delivering comprehensive, compassionate care.
Future Research and Innovations in Management
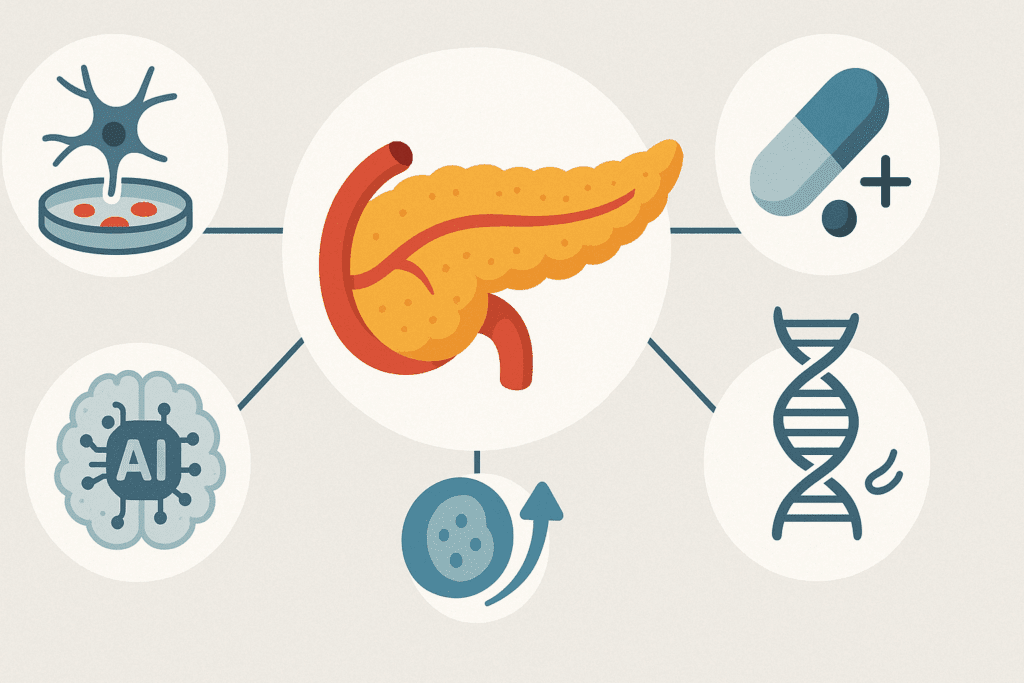
As our understanding of pancreatic diabetes evolves, so too do the possibilities for novel diagnostics and therapies. Ongoing research into regenerative medicine aims to restore damaged pancreatic tissue using stem cells or bioengineered beta cells. Immunomodulatory drugs that limit inflammation without impairing immunity are also being explored. In parallel, artificial intelligence tools are being developed to identify early biomarkers of pancreatic dysfunction in high-risk populations.
Personalized medicine approaches—guided by genetic, epigenetic, and metabolic profiling—may eventually allow for more precise prediction of which patients are likely to develop diabetes after pancreatitis. These advancements underscore a paradigm shift in how we view the pancreas and blood sugar relationship—not as a binary dysfunction but as a spectrum of interrelated abnormalities requiring nuanced solutions.
The Role of Public Health in Raising Awareness
Despite the growing evidence base, awareness of pancreatic diabetes remains limited among both healthcare providers and the general public. Public health campaigns focused on early recognition of pancreatitis symptoms, coupled with education about long-term risks, could lead to earlier diagnoses and better outcomes. Incorporating pancreas diabetes into national diabetes guidelines would also encourage more consistent screening and treatment practices.
Additionally, healthcare systems must allocate resources for multidisciplinary care models that can address the complex needs of this patient population. Training programs for medical professionals should include education on pancreas and blood sugar interactions, emphasizing the subtleties of this emerging condition. Informed policy and educational outreach are essential to bridging the current knowledge gap.
Frequently Asked Questions (FAQ): New Research on Pancreatitis and Diabetes
1. Can lifestyle changes reduce the risk of developing pancreatic diabetes after pancreatitis?
Absolutely, adopting targeted lifestyle changes can significantly influence the likelihood of developing pancreatic diabetes after an episode of pancreatitis. While the physiological damage from pancreatitis may predispose an individual to disruptions in insulin secretion, factors such as maintaining a nutrient-dense, low-inflammatory diet and reducing alcohol consumption can help preserve residual pancreatic function. Evidence suggests that incorporating antioxidants and omega-3 fatty acids into the diet may offer protective benefits to pancreatic tissue. Since the link between the pancreas and blood sugar regulation is so direct, any steps that stabilize glucose levels—such as routine exercise and stress management—can delay or reduce the onset of glucose intolerance. These approaches do not necessarily reverse pancreas diabetes but can mitigate its progression and improve quality of life.
2. Are there early warning signs that suggest a person may develop diabetes after pancreatitis?
In many cases, subtle symptoms can precede a formal diagnosis of diabetes following pancreatitis. These may include increased fatigue after meals, mild yet persistent digestive disturbances, or unexplained fluctuations in energy levels, all of which hint at disruptions in the pancreas and blood sugar equilibrium. Unlike traditional type 1 or type 2 diabetes, pancreatic diabetes often develops more insidiously and may be mistaken for general recovery symptoms from pancreatitis. Monitoring post-prandial glucose levels and assessing for declining pancreatic enzyme activity can serve as early clinical indicators. Identifying these changes early may enable clinicians to implement interventions that reduce the long-term impact of pancreas diabetes on metabolic health.
3. How is the psychological burden of pancreas diabetes different from other forms of diabetes?
The psychological impact of pancreatic diabetes can be profound, partly because it often occurs alongside chronic gastrointestinal symptoms and a sense of diminished vitality. Unlike type 2 diabetes, which is frequently associated with lifestyle choices, patients with pancreatic diabetes may struggle with feelings of helplessness, especially if their condition stems from unavoidable causes like hereditary pancreatitis or trauma. Additionally, the overlap of digestive symptoms with blood sugar fluctuations creates a unique management challenge that can lead to emotional exhaustion. Psychological support tailored to individuals coping with dual burdens of pancreatitis and diabetes is crucial, as it enhances treatment adherence and promotes emotional resilience. The bidirectional stress between mental health and metabolic regulation also underscores the intricate relationship between the pancreas and blood sugar systems.
4. What new technologies are being explored to diagnose pancreas diabetes earlier?
Emerging diagnostic tools are making it increasingly feasible to detect pancreas diabetes in its early stages. Advanced imaging modalities such as secretin-stimulated MRI and elastography are being refined to assess subtle changes in pancreatic structure and function. Furthermore, researchers are developing blood-based biomarkers that reflect early beta-cell stress or apoptosis, offering non-invasive indicators of endocrine dysfunction. Machine learning algorithms are also being employed to analyze large datasets from patients with pancreatitis to predict who is most likely to develop diabetes. These innovations are grounded in a deeper appreciation of how closely the pancreas and blood sugar regulation systems interact, opening the door for preemptive care rather than reactive treatment.
5. How does pancreatic diabetes affect nutritional status and what can be done about it?
Pancreatic diabetes often presents alongside exocrine pancreatic insufficiency, meaning that individuals have difficulty digesting and absorbing nutrients. This can lead to deficiencies in fat-soluble vitamins (A, D, E, and K), as well as unintended weight loss and muscle wasting. Unlike in other forms of diabetes, patients with pancreas diabetes must be vigilant not only about blood sugar but also about nutritional balance. Enzyme replacement therapy can alleviate some digestive challenges, and individualized nutrition plans rich in easily digestible proteins and complex carbohydrates can help maintain stable energy levels. Addressing both endocrine and exocrine functions simultaneously is essential for restoring metabolic balance in pancreatic diabetes.
6. Does pancreatitis cause diabetes directly, or are other factors involved?
While it is clear that pancreatitis increases the risk of developing diabetes, whether it causes the disease directly depends on several factors including the severity, frequency, and duration of inflammation. In severe cases, does pancreatitis cause diabetes through direct destruction of islet cells that produce insulin? Yes, but it’s also true that genetic predispositions, coexisting metabolic conditions, and environmental triggers can mediate this process. Therefore, a comprehensive evaluation is necessary to determine if pancreatic inflammation is the sole contributor. Recognizing this complexity is vital, especially since interventions must be customized to reflect not only the damage caused by pancreatitis but also the broader metabolic profile of the individual.
7. How should healthcare providers distinguish pancreatic diabetes from type 1 and type 2 diabetes?
Differentiating pancreatic diabetes from other diabetes types requires a multi-modal approach that considers both endocrine and digestive function. Healthcare providers should look for clinical clues such as a history of pancreatitis, presence of exocrine insufficiency, and atypical glycemic patterns that don’t fit classic diagnostic molds. Testing for pancreatic enzymes and conducting imaging to assess pancreatic morphology can provide important diagnostic clarity. The challenge lies in the fact that many guidelines still lack a dedicated framework for diagnosing pancreas diabetes, which often leads to misclassification. Increasing awareness and educating clinicians about the nuances of the pancreas and blood sugar relationship is key to improving diagnostic accuracy.
8. What role does the gut microbiome play in the progression of pancreatic diabetes?
Recent research suggests that the gut microbiome may play an underappreciated role in the progression and management of pancreatic diabetes. In individuals with chronic pancreatitis, altered gut flora may exacerbate inflammation and compromise nutrient absorption, indirectly influencing glucose metabolism. Dysbiosis has also been linked to impaired gut barrier function, which can promote systemic inflammation and further disrupt the pancreas and blood sugar axis. Probiotic therapy and dietary interventions targeting microbiome health may hold promise as adjunct strategies in managing pancreas diabetes. While this area is still under investigation, the implications for personalized medicine are substantial and deserve further exploration.
9. Are there occupational or environmental exposures that raise the risk of pancreatic diabetes?
Yes, certain environmental and occupational exposures may increase the risk of both pancreatitis and subsequent diabetes. Long-term exposure to industrial solvents, heavy metals, and persistent organic pollutants has been implicated in pancreatic inflammation. Workers in industries such as metal manufacturing, chemical processing, and agriculture may face elevated risks, particularly if protective protocols are not strictly followed. These exposures can initiate inflammatory pathways that disrupt both the exocrine and endocrine functions of the pancreas, potentially leading to pancreas diabetes. Public health initiatives that emphasize workplace safety and early screening for at-risk populations could help reduce these environmentally mediated cases.
10. What are some promising therapies being researched to prevent diabetes after pancreatitis?
Several promising therapies are under investigation to prevent the transition from pancreatitis to diabetes. Anti-inflammatory agents that specifically target pancreatic tissue are being studied for their potential to limit damage during acute episodes. Additionally, regenerative therapies using stem cells to restore insulin-producing beta cells are in early phases of research. Some pharmacological compounds are being explored for their ability to modulate the pancreas and blood sugar dynamics without the adverse side effects of traditional glucose-lowering drugs. Personalized medicine approaches—guided by genetic and metabolic profiling—are also showing promise in tailoring prevention strategies. These efforts reflect a growing recognition of the unique clinical challenges posed by pancreatic diabetes and a commitment to advancing care beyond conventional paradigms.
Conclusion: Why the Pancreas-Diabetes Connection Deserves More Attention
The question of whether pancreatitis causes diabetes or signals a deeper dysfunction in glucose regulation reflects a broader truth: the pancreas is a central, though often underappreciated, player in metabolic health. As research continues to reveal the depth of the connection between pancreas and blood sugar systems, the need for more sophisticated diagnostic tools, personalized therapies, and public awareness becomes increasingly clear. Pancreatic diabetes is not simply a complication of another disease—it is a distinct and challenging condition that demands attention from the full spectrum of healthcare disciplines. For clinicians, researchers, and patients alike, acknowledging and addressing this condition could dramatically improve outcomes and quality of life for a growing and underserved population.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Diabetes mellitus as a consequence of acute severe pancreatitis: Unraveling the mystery
Impact of Serum Glucose Levels on Outcomes in Acute Pancreatitis: A Retrospective Analysis
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.