Understanding Diabetes as a Chronic Condition
Diabetes is not a temporary ailment; it is a lifelong condition that demands continuous attention and adaptation. As research progresses, our understanding of diabetes has expanded, revealing that individuals can indeed live full, healthy lives despite the diagnosis. However, this requires a nuanced understanding of how diabetes affects the body, how it evolves over time, and the importance of early and ongoing intervention. Diabetes is a metabolic disorder characterized by persistent hyperglycemia due to either insufficient insulin production, impaired insulin action, or both. The condition is commonly categorized into type 1 diabetes, type 2 diabetes, and gestational diabetes, with type 2 diabetes being the most prevalent globally.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
While a diabetes diagnosis may initially feel overwhelming, it is crucial to recognize that it does not equate to a death sentence. In fact, advancements in medicine, digital health tools, and lifestyle interventions have radically transformed the diabetes prognosis in recent decades. Living with diabetes today is markedly different from what it was just a generation ago. With a combination of education, personalized treatment, and sustained effort, individuals can navigate the challenges of diabetes and reduce the risk of complications significantly.
Can You Live with Diabetes? A Question of Adaptation and Awareness
The question “Can you live with diabetes?” speaks not only to the survivability of the condition but also to the quality of life that can be achieved while managing it. This question underscores a broader inquiry into how people can adapt to chronic illness and thrive despite ongoing medical demands. Research has consistently shown that individuals who maintain consistent routines in monitoring blood sugar, following prescribed treatment plans, and making informed lifestyle choices often experience a favorable diabetes prognosis.
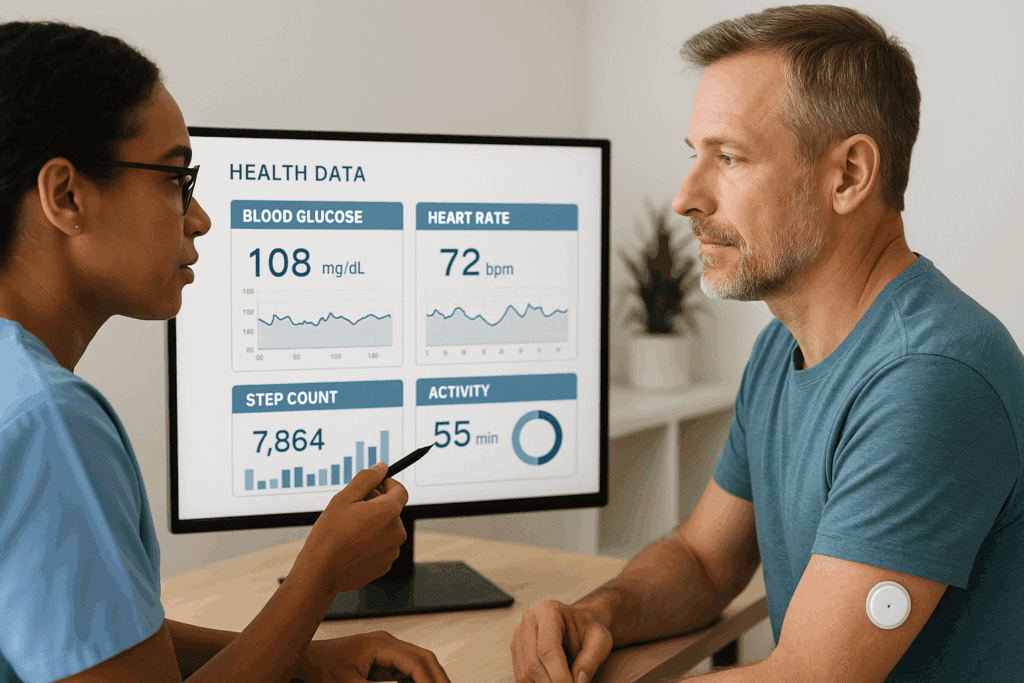
Indeed, the concept of living with diabetes should be reframed from mere survival to sustainable well-being. The prognosis for individuals who adhere to comprehensive diabetes management strategies is increasingly optimistic. The integration of technology, such as continuous glucose monitors (CGMs) and insulin pumps, has revolutionized self-care. These tools not only improve glycemic control but also empower patients with real-time insights, allowing for informed decisions that prevent complications and enhance daily life. As a result, the phrase “can you live with diabetes” becomes a starting point for exploring how to thrive with it, rather than just cope.
Reassessing Type 2 Prognosis in the Era of Personalized Medicine
Type 2 diabetes was once viewed as a progressive disease with an inevitable decline in pancreatic function and rising dependency on insulin therapy. However, the narrative surrounding type 2 prognosis is evolving. Recent research into metabolic flexibility, beta-cell preservation, and the potential for diabetes remission challenges long-held assumptions about the trajectory of this condition. Early intervention remains key, but the window for significant improvement often extends beyond initial diagnosis.
One of the most promising developments in improving type 2 prognosis is the emergence of precision medicine. By leveraging genetic, biomarker, and behavioral data, healthcare providers can now tailor interventions that are more effective and better suited to individual needs. For instance, certain patients respond exceptionally well to specific types of exercise, dietary patterns, or medication regimens based on their genetic profiles or insulin resistance patterns. These advancements not only alter the expected course of diabetes 2 prognosis but also give patients a renewed sense of agency in managing their condition.
Strategies for Long-Term Diabetes Management
Long-term diabetes management is more than just a checklist of daily tasks; it is an evolving strategy that adjusts to the person’s age, lifestyle, medical history, and psychosocial context. The cornerstone of effective diabetes management lies in maintaining optimal blood glucose levels through a triad of medication, nutrition, and physical activity. However, within this framework, nuances emerge that distinguish successful management from suboptimal care.
Nutrition remains foundational, but the approach has moved beyond simply avoiding sugar. Contemporary dietary strategies emphasize glycemic load, nutrient density, and meal timing. Individuals are encouraged to adopt sustainable eating habits rather than restrictive diets. Coupled with this is the role of physical activity, which improves insulin sensitivity, supports weight management, and enhances cardiovascular health. Moreover, newer classes of medications, such as GLP-1 receptor agonists and SGLT2 inhibitors, have demonstrated cardiovascular and renal benefits in addition to glycemic control, redefining the goals of diabetes management.
Behavioral and psychological aspects are equally important. Studies show that emotional resilience, motivation, and support systems play pivotal roles in long-term outcomes. Thus, diabetes education programs are increasingly incorporating cognitive-behavioral techniques, peer support, and digital coaching platforms. By addressing the human experience behind the numbers, these programs improve adherence and empower patients to take control of their health.
The Role of Early Detection and Proactive Monitoring
Timely diagnosis and vigilant monitoring are critical components in shaping a favorable diabetes prognosis. Early detection of both type 1 and type 2 diabetes allows for the implementation of strategies that can delay disease progression, prevent complications, and improve quality of life. With the growing awareness around prediabetes, more individuals are being identified at risk and are initiating preventive measures before full-blown diabetes develops.
Technological innovations have played a transformative role in monitoring. Continuous glucose monitoring and digital health applications enable real-time data collection, which facilitates proactive adjustments to lifestyle and treatment. This real-time feedback loop has not only improved clinical outcomes but also helped patients feel more connected and in control of their condition. Furthermore, advancements in wearable technologies now allow for the detection of hypoglycemia or hyperglycemia before symptoms become severe, preventing emergencies and hospitalizations.
Regular screenings for comorbid conditions—such as hypertension, dyslipidemia, and kidney disease—are vital in comprehensive diabetes management. These screenings inform clinicians about potential risks and enable the early deployment of interventions. As a result, the overall diabetes prognosis improves not only in terms of longevity but also in preserving quality of life. Patients who engage in consistent monitoring often report better symptom control, fewer complications, and greater peace of mind.
Lifestyle Interventions That Transform Prognosis
While pharmacological treatments are crucial, lifestyle modifications remain the most impactful and sustainable interventions in diabetes care. The evidence supporting lifestyle-based strategies is overwhelming. Weight loss, even as modest as 5–10% of total body weight, has been shown to improve insulin sensitivity and, in many cases, lead to remission of type 2 diabetes. Programs such as the Diabetes Prevention Program (DPP) have demonstrated that lifestyle interventions can outperform medication in delaying or preventing diabetes onset.
Dietary changes that prioritize whole, minimally processed foods, increased fiber intake, and healthy fats have been associated with improved glycemic control and cardiovascular outcomes. Intermittent fasting, low-carbohydrate diets, and plant-based eating are being explored as viable strategies depending on individual preferences and metabolic responses. These approaches are not one-size-fits-all; rather, they reflect the growing movement toward personalized nutrition in diabetes management.
Physical activity also plays a critical role. Aerobic exercise, resistance training, and even light daily movement have been linked to improved glucose metabolism and reduced insulin resistance. Importantly, the psychological benefits of regular physical activity—such as stress reduction, improved sleep, and enhanced mood—contribute indirectly to better management outcomes. As the connection between lifestyle and health becomes increasingly clear, patients are empowered to make changes that not only extend life but enrich it.
Reframing Diabetes 2 Prognosis in the Context of Remission
Perhaps one of the most hopeful shifts in diabetes discourse is the possibility of remission, particularly for those with type 2 diabetes. Though traditionally seen as irreversible, new evidence suggests that with sustained weight loss, lifestyle changes, and, in some cases, bariatric surgery, individuals can achieve normoglycemia without ongoing medication. This paradigm shift redefines what we understand as a successful diabetes 2 prognosis.
Remission, however, is not a cure. It requires continued vigilance and ongoing lifestyle management to maintain. Yet the mere possibility of reversing the disease process is a powerful motivator for many patients. Studies such as the DiRECT trial in the UK have shown that a significant proportion of individuals who undergo intensive weight-loss programs can maintain normal blood sugar levels for at least two years. These findings challenge outdated notions of type 2 diabetes as a relentlessly progressive disease.
For remission to become a realistic goal for more individuals, healthcare systems must evolve to support intensive lifestyle interventions. Insurance coverage, provider training, and public health messaging all play a role in promoting the idea that a better outcome is possible. By redefining the type 2 prognosis landscape, we open the door to renewed hope and proactive engagement with treatment.
Navigating the Emotional and Social Dimensions of Living with Diabetes
Beyond the physiological impact, diabetes exerts a profound emotional and social toll on individuals. The constant vigilance required for blood sugar monitoring, dietary planning, and medication adherence can lead to burnout, stress, and anxiety. Diabetes distress—a term used to describe the emotional burdens specific to managing this chronic condition—is increasingly recognized as a factor that can negatively impact self-care and health outcomes.
Social support is essential for mitigating these effects. Individuals who have access to supportive family members, friends, and peer communities often report better psychological well-being and higher adherence to treatment plans. Healthcare providers are now encouraged to assess emotional well-being as part of routine diabetes care and to refer patients to mental health services when needed. Moreover, online communities and digital health platforms offer new ways for people living with diabetes to connect, share experiences, and find encouragement.
The emotional resilience required to live well with diabetes is often underestimated. It involves not just coping with the medical aspects but also navigating societal stigma, workplace challenges, and changes in personal identity. By integrating emotional and social health into the broader framework of diabetes management, we can foster more holistic and compassionate care models that truly support long-term well-being.
Advancements in Research and Their Implications for the Future
The field of diabetes research is rapidly evolving, with breakthroughs that hold the potential to further improve diabetes prognosis and quality of life. Innovations in beta-cell regeneration, stem cell therapy, and immunomodulation offer exciting possibilities for both type 1 and type 2 diabetes. Clinical trials are underway exploring the potential of implantable insulin-producing cells and gene editing technologies, which may one day provide lasting solutions beyond current treatments.
Artificial intelligence and machine learning are also transforming diabetes management by enabling predictive modeling, personalized treatment plans, and improved diagnostic tools. These technologies can analyze vast amounts of patient data to identify patterns and recommend interventions with a level of precision previously unattainable. As these innovations mature, they promise to make diabetes management more proactive, efficient, and patient-centered.
Public health initiatives and global awareness campaigns are contributing to earlier diagnosis, better education, and reduced stigma. The integration of diabetes care into primary health systems ensures that more people, especially in underserved communities, receive timely and effective support. As a result, the long-term outlook for individuals living with diabetes continues to improve, driven by a combination of scientific progress, policy reform, and empowered self-management.
Frequently Asked Questions: Can You Live with Diabetes? Long-Term Prognosis and Management Insights
1. How does sleep quality affect long-term diabetes prognosis?
Sleep quality has a surprisingly significant impact on diabetes prognosis. Poor sleep has been linked to impaired glucose metabolism, increased insulin resistance, and elevated cortisol levels—all of which can worsen blood sugar control. Over time, chronic sleep disturbances can contribute to cardiovascular risks and diabetic complications, thus deteriorating overall diabetes management. For those with type 2 diabetes, ensuring adequate sleep may serve as a low-effort but highly effective adjunct therapy that supports a more favorable type 2 prognosis. Investing in proper sleep hygiene can be just as critical as diet and exercise in shaping a positive diabetes 2 prognosis.
2. Can mindfulness and stress-reduction techniques improve diabetes management outcomes?
Yes, and the benefits are increasingly supported by research. Stress triggers hormonal fluctuations that raise blood glucose levels, making emotional regulation a key aspect of diabetes management. Mindfulness-based stress reduction (MBSR), yoga, and cognitive-behavioral therapy have shown promise in reducing A1C levels and improving patient-reported outcomes. These techniques foster psychological resilience and reduce diabetes-related burnout, especially important in sustaining long-term adherence to care plans. By promoting relaxation and emotional awareness, these interventions can contribute to an improved diabetes prognosis, especially when integrated with standard treatment.
3. What role does gut health play in type 2 prognosis and blood sugar regulation?
Emerging research suggests that the gut microbiome plays a crucial role in insulin sensitivity and inflammation, both of which influence type 2 prognosis. An imbalanced gut ecosystem may contribute to metabolic dysfunctions commonly seen in type 2 diabetes. Incorporating fermented foods, fiber-rich plants, and prebiotics into the diet can help restore a healthier gut flora. These dietary choices are proving beneficial not just for gastrointestinal health but for systemic glucose control as well. Optimizing gut health could become a foundational strategy in modern diabetes management, offering a novel pathway for improving diabetes 2 prognosis.
4. Can people with diabetes safely participate in high-intensity exercise programs?
Absolutely, with proper guidance and individualization. While traditional advice has focused on moderate-intensity exercise, newer findings suggest that high-intensity interval training (HIIT) can enhance insulin sensitivity and accelerate weight loss in people with type 2 diabetes. However, it’s important to undergo a clinical evaluation before beginning such programs, especially for those with cardiovascular risks. Personalized fitness planning, often guided by a diabetes care team, ensures safety while maximizing benefits. When implemented correctly, exercise regimens like HIIT can improve both physical fitness and long-term diabetes prognosis.
5. How do social determinants of health influence diabetes 2 prognosis in underserved populations?
Diabetes prognosis is not shaped by biology alone; social determinants such as income, education, and neighborhood access to healthy foods significantly affect outcomes. Underserved populations often face barriers to healthcare, medication, and preventive screenings, which can accelerate the progression of complications. In these settings, effective diabetes management requires addressing systemic inequities alongside clinical care. Community-based interventions and culturally tailored education programs have shown success in bridging this gap. Enhancing social support and access can markedly improve the type 2 prognosis among vulnerable groups.
6. Are there gender-specific differences in diabetes management and outcomes?
Yes, gender can subtly influence both the experience of diabetes and its long-term management. Women with diabetes often face a higher relative risk of cardiovascular disease than men, even with similar glycemic control. Hormonal fluctuations related to menstruation, pregnancy, and menopause can also complicate blood sugar regulation. Conversely, men are less likely to seek regular care, which can delay diagnosis and impact diabetes 2 prognosis. A gender-sensitive approach to diabetes care recognizes these differences and promotes more individualized and effective treatment plans.
7. What advancements are being made in non-invasive glucose monitoring for better diabetes management?
Non-invasive technologies represent the frontier of patient-centered diabetes management. Innovations like skin sensors, tear-based diagnostics, and near-infrared spectroscopy aim to monitor glucose without the need for fingersticks. These tools promise greater convenience and adherence, especially among patients wary of invasive testing. While most are still in the experimental or early commercial stages, their future integration could redefine how people approach diabetes self-care. More intuitive and painless monitoring may dramatically enhance daily management and, by extension, diabetes prognosis.
8. How does food insecurity affect the ability to maintain consistent diabetes management?
Food insecurity poses a profound challenge to effective diabetes care. Individuals with limited access to nutritious, affordable food often rely on processed items high in sugar and saturated fats, undermining glycemic control. This not only worsens metabolic markers but also increases psychological stress, compounding the burden of chronic illness. Food insecurity has been linked to higher rates of hospitalization and poor diabetes 2 prognosis across diverse populations. Policies and community programs that improve food access are therefore essential in advancing equitable diabetes management.
9. Can you live with diabetes without ever needing medication?
In certain cases—particularly with type 2 diabetes caught early—it is possible to manage blood glucose levels without long-term medication. Lifestyle changes such as weight loss, dietary adjustments, and consistent physical activity can sometimes lead to remission or delay the need for pharmaceuticals. However, this is highly individualized, and many patients will eventually require medication to maintain safe glucose levels. Rather than viewing this as a failure, incorporating medications should be seen as a strategic tool within a comprehensive care plan. Even with medication, an optimized lifestyle continues to play a central role in shaping a positive diabetes prognosis.
10. What psychological tools help individuals accept and adapt to a lifelong diagnosis like diabetes?
Coming to terms with a chronic condition involves more than clinical understanding; it requires emotional adaptation. Psychological frameworks like acceptance and commitment therapy (ACT) have been beneficial in helping individuals navigate the emotional landscape of living with diabetes. These models encourage people to focus on their values and develop flexible coping strategies rather than resist difficult emotions. Building emotional intelligence and self-compassion has been shown to improve adherence and overall diabetes management. Long-term adaptation not only enhances mental well-being but directly contributes to a stronger and more sustainable diabetes 2 prognosis.
A New Era of Hope: What the Future Holds for Diabetes Management and Prognosis
Living with diabetes is no longer a narrative of inevitable decline, but rather one of transformation, empowerment, and resilience. Advances in medicine, technology, and behavioral science have redefined what it means to manage this chronic condition successfully. The question “can you live with diabetes?” has evolved into an affirmation: you can live well—and even thrive—with diabetes, given the right tools, education, and support.
As we look to the future, the diabetes prognosis is increasingly shaped by proactive care, personalized medicine, and the integration of mental and social well-being into treatment paradigms. From rethinking the traditional assumptions about type 2 prognosis to exploring the frontiers of remission, the path forward is filled with possibility. The journey is not without its challenges, but with evidence-based strategies, emotional resilience, and continued innovation, individuals with diabetes can achieve not only longevity but also a rich and fulfilling quality of life.
In this new era, the focus shifts from merely controlling the disease to empowering individuals to take charge of their health. By fostering a deeper understanding of diabetes management and emphasizing the realistic potential for favorable outcomes, we can help millions of people rewrite the story of what it means to live with diabetes today—and in the years to come.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Type 2 diabetes and life expectancy
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.