Understanding the Scope of Diabetes and Its Systemic Reach
Diabetes, once largely viewed as a metabolic disorder defined by abnormal blood sugar regulation, is now recognized as a condition that touches nearly every organ and physiological system. As global research advances, scientists and clinicians are uncovering the profound and often underestimated effects of this chronic disease on the human body. This shift in understanding has propelled medical experts to explore not only how diabetes alters blood glucose levels but also how it causes complex, far-reaching damage over time.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
One of the most pressing concerns among researchers is identifying the specific diabetes effects on body systems that develop gradually and quietly. While initial symptoms may seem localized or even manageable, the long-term implications—ranging from cardiovascular deterioration to impaired neurological function—underscore the necessity for early intervention and comprehensive care. The question is no longer limited to whether diabetes is simply a metabolic issue but rather how it becomes a multisystem disease that alters the structural and functional integrity of the body.
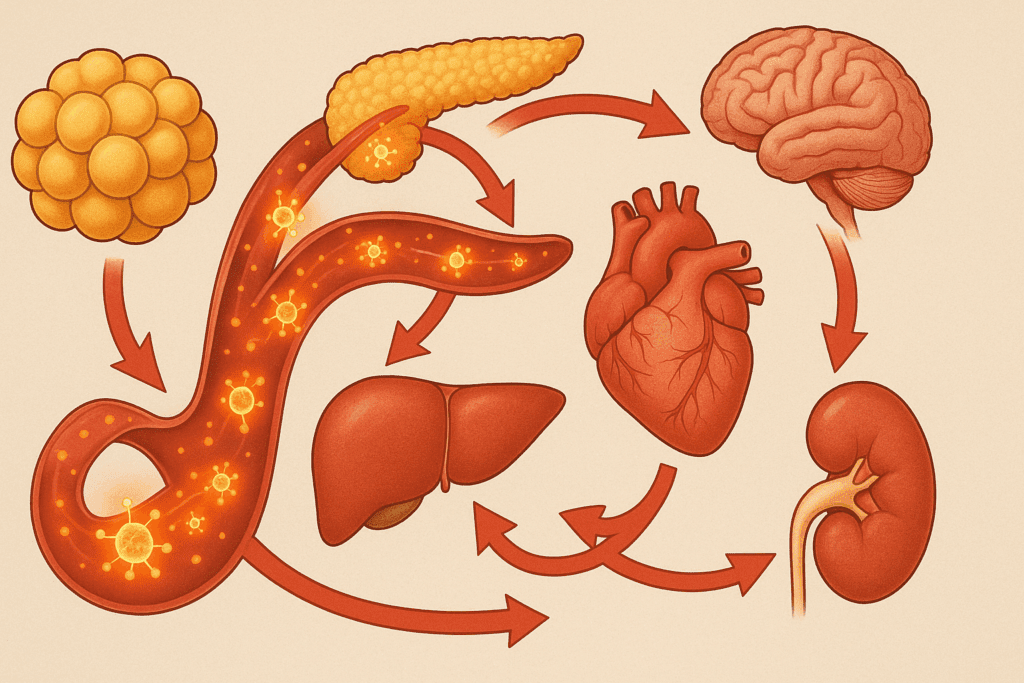
As we delve into the newest findings, it becomes increasingly evident that understanding what organs diabetes affects is essential for prevention and personalized treatment strategies. These insights also raise questions about whether diabetes is a disease of the pancreas or liver, as emerging data suggest a more interconnected and system-wide pathology than previously imagined. Through the lens of new research, we can better grasp the true burden of diabetes as not merely a condition of glucose control but as a whole-body disorder.
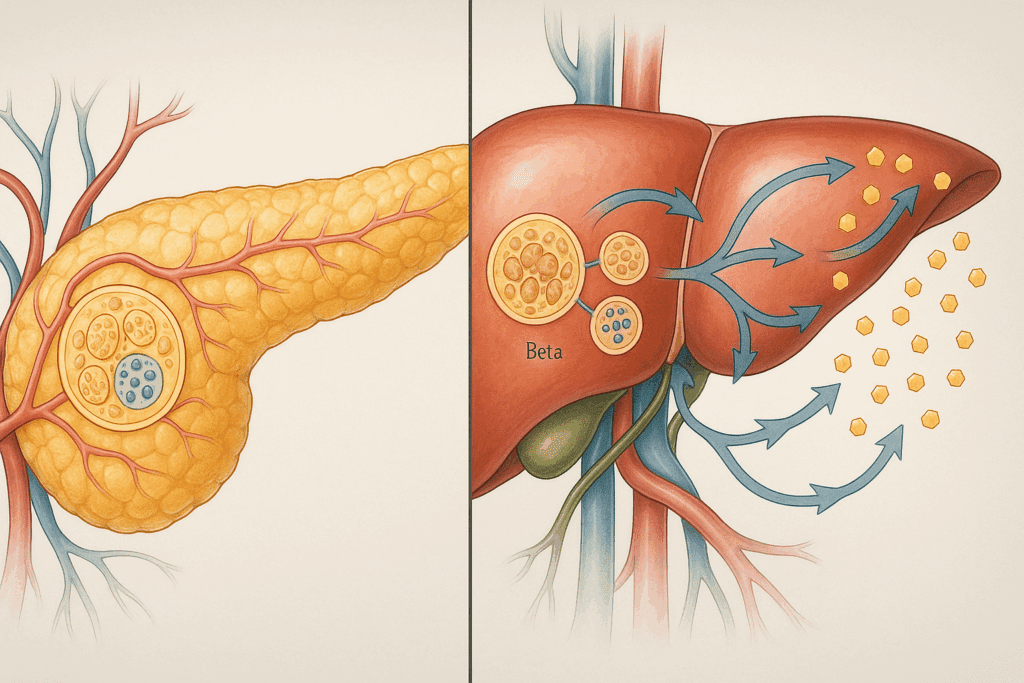
The Pancreas, Liver, and the Core of Diabetes Development
At the heart of diabetes lies a dysfunction in insulin production and utilization, implicating the pancreas as a primary organ in the disease’s onset. The pancreas houses the islets of Langerhans, which contain beta cells responsible for insulin secretion. In type 1 diabetes, an autoimmune attack on these cells halts insulin production altogether. In type 2 diabetes, insulin resistance occurs, where the body’s cells become unresponsive to insulin, often leading to eventual pancreatic beta-cell exhaustion. In both cases, the pancreas plays a critical role, but new studies are now exploring how the liver is equally involved in this process.
This dual-organ perspective prompts deeper inquiry into whether diabetes is a disease of the pancreas or liver. The liver, responsible for glucose storage and release, becomes dysregulated in diabetes. Insulin normally inhibits hepatic glucose output, but in diabetic individuals, this process is impaired, leading to excess glucose being dumped into the bloodstream. This hepatic insulin resistance is now believed to contribute significantly to hyperglycemia, thus positioning the liver not as a secondary player but as a co-conspirator in the pathophysiology of diabetes.
Recent research has illuminated the feedback loops between the pancreas and liver, particularly involving signaling pathways like the insulin-AKT-FoxO1 cascade. These insights challenge the traditional view of diabetes as a pancreas-centric disease and instead support the notion that it is a systemic metabolic disorder involving multiple organs from the outset. Understanding these relationships not only deepens our grasp of diabetes organ pathology but also opens doors for targeted therapies that address both pancreatic and hepatic dysfunction.
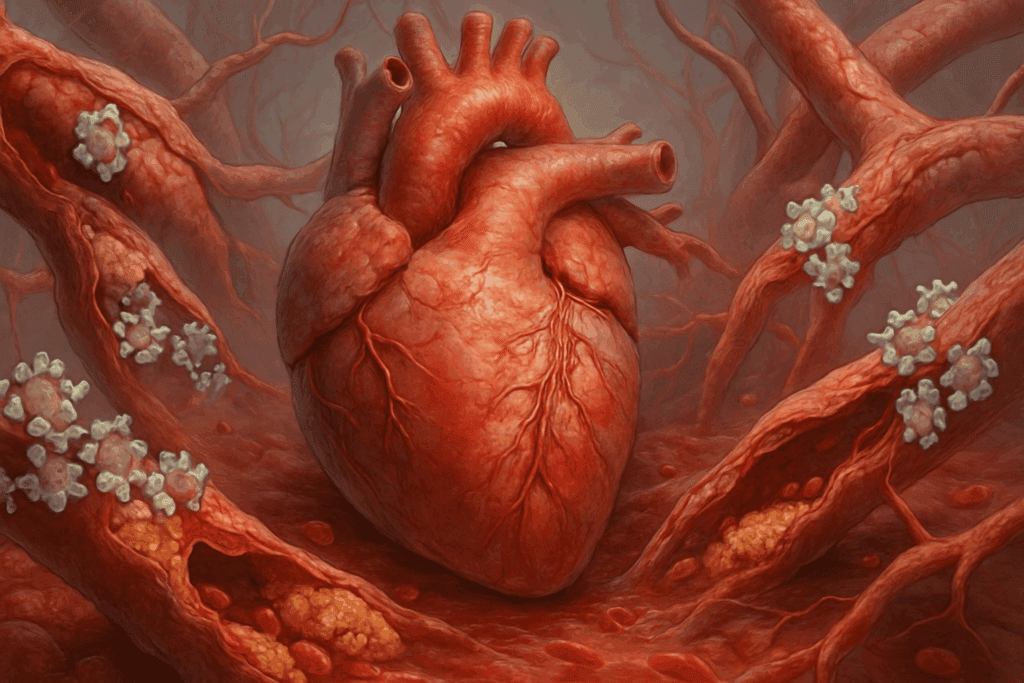
Cardiovascular Consequences: The Heart’s Vulnerability to Diabetes
The cardiovascular system is one of the most profoundly affected body systems in diabetes, with heart disease being the leading cause of death among diabetic patients. Chronic hyperglycemia promotes inflammation, endothelial dysfunction, and accelerated atherosclerosis, all of which elevate the risk for coronary artery disease, stroke, and heart failure. These outcomes are not simply comorbidities but direct consequences of prolonged metabolic imbalance.
One of the critical mechanisms linking diabetes to cardiovascular damage is glycation—the non-enzymatic attachment of glucose to proteins—which leads to the formation of advanced glycation end-products (AGEs). AGEs alter the structure and function of blood vessels, making them less elastic and more prone to rupture or blockage. Furthermore, insulin resistance, a hallmark of type 2 diabetes, contributes to dyslipidemia, characterized by elevated triglycerides and low levels of protective HDL cholesterol, compounding cardiovascular risk.
New clinical trials are now evaluating medications such as SGLT2 inhibitors and GLP-1 receptor agonists for their cardioprotective effects, reflecting a paradigm shift in diabetes management. No longer is glucose control the sole endpoint; protecting the organs affected by diabetes—particularly the heart—is now an integral part of treatment algorithms. These insights underscore how diabetes effects on body systems extend far beyond glycemic thresholds, highlighting the need for comprehensive, organ-targeted care.
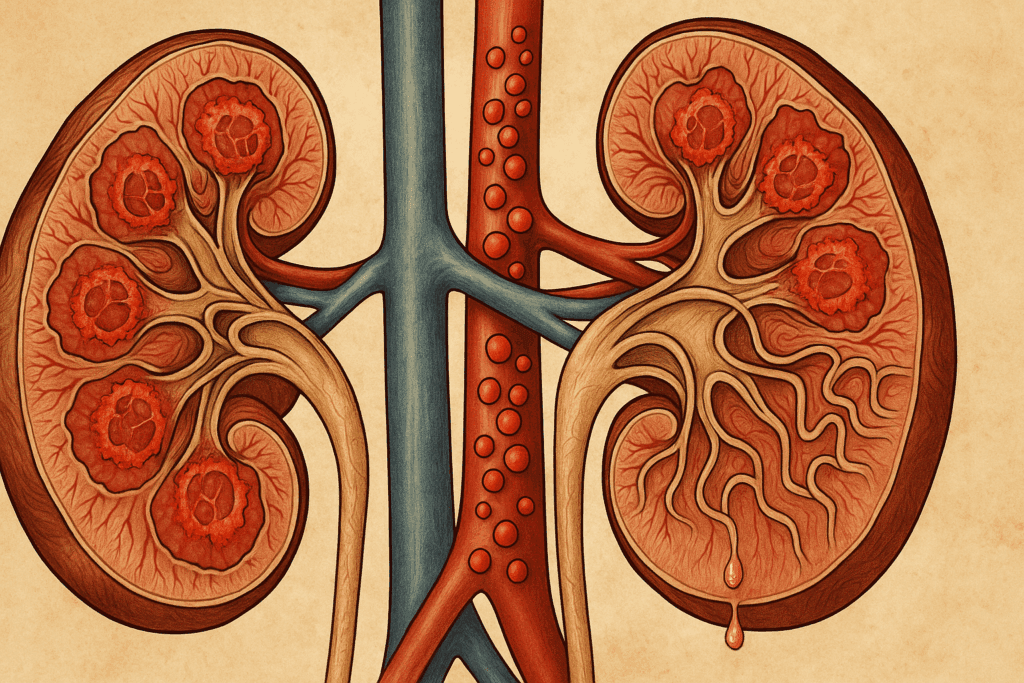
The Kidneys and Diabetic Nephropathy: A Silent Struggle
The kidneys are another major target of diabetic damage, with diabetic nephropathy being the leading cause of chronic kidney disease and end-stage renal failure globally. The kidneys filter waste from the blood through an intricate network of glomeruli, which are highly sensitive to glucose levels. In diabetes, prolonged hyperglycemia damages these delicate structures, leading to protein leakage (albuminuria), reduced filtration capacity, and eventual renal failure.
One of the emerging themes in recent studies is the inflammatory component of diabetic nephropathy. While high glucose levels have long been recognized as a driving force, new evidence points to immune system activation and oxidative stress as key contributors to kidney deterioration. This expanded understanding helps explain why traditional glucose-lowering treatments may not fully halt kidney damage.
Clinicians now focus on early screening for microalbuminuria and the use of medications like ACE inhibitors and ARBs to delay disease progression. In addition, novel therapies targeting inflammation and fibrosis are under development, aiming to protect one of the most critically impacted diabetes organs before irreversible damage sets in. The growing emphasis on renal preservation reflects a broader trend of understanding diabetes as a multi-organ disease.
Neurological Complications: The Brain and Nerves Under Siege
Neuropathy, both peripheral and autonomic, represents one of the most debilitating complications of diabetes, affecting the nervous system’s ability to transmit signals efficiently. Patients may experience tingling, numbness, or sharp pain in the limbs, as well as gastrointestinal irregularities, bladder dysfunction, and even impaired cardiovascular regulation due to autonomic nerve involvement. These symptoms illustrate how diabetes effects on body systems can lead to substantial declines in quality of life.
Emerging studies also suggest that diabetes increases the risk for cognitive decline and neurodegenerative diseases, including Alzheimer’s disease—a condition some researchers now refer to as “type 3 diabetes.” Chronic hyperglycemia, insulin resistance, and inflammation are believed to disrupt the blood-brain barrier and impair neuronal energy metabolism, laying the groundwork for memory impairment and executive dysfunction.
Understanding the neurological implications of diabetes expands our view of the organs affected by diabetes beyond traditionally recognized structures. It highlights the importance of early and aggressive glycemic control, not only to prevent peripheral nerve damage but also to safeguard cognitive function in the long term. With ongoing research into neuroprotective strategies, the brain is increasingly becoming a central focus in comprehensive diabetes care.
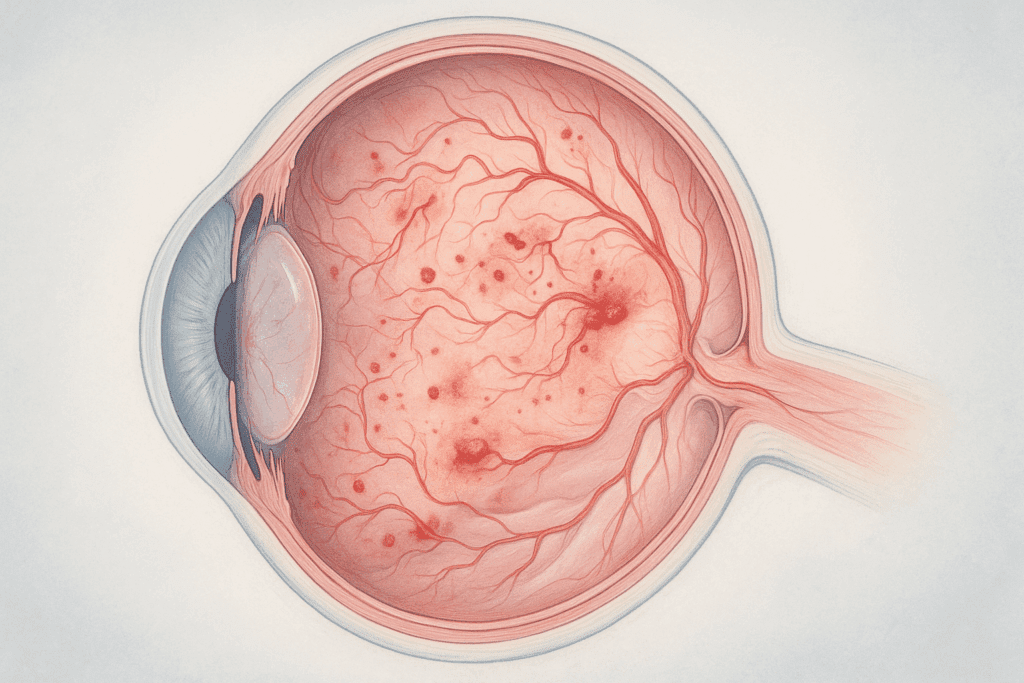
The Eyes and Vision Loss: Retinal Complications of Diabetes
Diabetic retinopathy is a leading cause of vision impairment and blindness among adults, resulting from damage to the blood vessels of the retina. In the early stages, small vessels may leak fluid or hemorrhage, while advanced stages involve the growth of abnormal new vessels, retinal detachment, and macular edema. Because these changes often occur without early symptoms, regular eye examinations are vital for diabetic patients.
New imaging technologies, including optical coherence tomography and retinal angiography, allow for earlier detection and better monitoring of diabetic eye disease. Moreover, treatments such as anti-VEGF injections and laser photocoagulation have transformed the management of diabetic retinopathy, making vision preservation more achievable than ever before.
However, the increasing prevalence of diabetes worldwide means a corresponding rise in vision-threatening complications, emphasizing the need for prevention through systemic glucose control. Understanding what organs diabetes affects must include the eyes—not just as a peripheral concern but as a central aspect of patient quality of life. Research is also investigating how early retinal changes can serve as biomarkers for broader vascular damage, linking eye health to overall systemic well-being.
The Immune System and Inflammatory Pathways in Diabetes
Chronic inflammation is now recognized as a key mediator in the progression of diabetes and its complications. In both type 1 and type 2 diabetes, the immune system plays a pivotal role—whether through autoimmunity in the former or low-grade systemic inflammation in the latter. These immune responses contribute not only to the onset of diabetes but also to the damage sustained by various organ systems over time.
Studies have shown that adipose tissue in obese individuals secretes pro-inflammatory cytokines such as TNF-alpha and interleukin-6, which interfere with insulin signaling and promote insulin resistance. This inflammatory milieu exacerbates damage to the pancreas, liver, kidneys, and cardiovascular system, suggesting that the diabetes organ effects are at least partially mediated by immune dysregulation.
Emerging therapies aimed at modulating inflammation—such as IL-1 inhibitors and other biologic agents—are being explored for their potential to slow disease progression. Understanding the immune system’s role offers a new lens through which to view diabetes, not merely as a metabolic imbalance but as a chronic inflammatory disease with widespread consequences. These findings have redefined how clinicians approach the long-term care of patients, incorporating anti-inflammatory strategies alongside traditional treatments.
Gastrointestinal and Endocrine Disruption: More Than Blood Sugar
Diabetes also alters gastrointestinal function, often leading to complications such as gastroparesis, a condition where the stomach empties too slowly. This delay can result in nausea, vomiting, bloating, and erratic blood sugar levels, making diabetes management more challenging. The condition is linked to autonomic neuropathy affecting the vagus nerve, illustrating how interconnected diabetes effects on body systems truly are.
Moreover, hormonal imbalances beyond insulin dysregulation play a role in diabetes pathology. Incretins—hormones released by the gut in response to food—are often impaired in people with diabetes. These hormones help regulate insulin secretion and appetite, and their dysfunction can lead to overeating and poor glycemic control. New medications such as GLP-1 receptor agonists target these pathways and offer promising results in both blood sugar regulation and weight loss.
The gastrointestinal and endocrine interplay in diabetes exemplifies how this disease impacts more than just glucose. It disrupts hormone networks, digestive motility, and nutrient absorption, adding layers of complexity to treatment and quality of life. A deeper understanding of these connections reinforces the idea that diabetes is far more than a single-organ condition—it is a web of dysfunction that spans the body.
Frequently Asked Questions: How Diabetes Affects Organs and Body Systems
1. How do psychological stress and emotional health influence the organs affected by diabetes?
While diabetes is traditionally viewed through a physiological lens, growing research highlights how chronic psychological stress exacerbates complications in organs affected by diabetes. Stress hormones like cortisol can worsen insulin resistance and elevate blood glucose levels, contributing to damage in the kidneys, heart, and nervous system. Mental health conditions such as depression and anxiety are also linked to poorer glycemic control, indirectly increasing risk to multiple body systems affected by diabetes. This underscores the need for integrated care that includes mental health support as part of diabetes management. Addressing emotional well-being can help protect both metabolic balance and diabetes organ health more effectively.
2. Is diabetes a disease of the pancreas or liver, and how does this classification affect treatment strategies?
The debate around whether diabetes is a disease of the pancreas or liver remains ongoing, but modern research suggests it is a disease of both—and beyond. The pancreas is the source of insulin, while the liver regulates glucose storage and release, and both play interdependent roles in glucose homeostasis. Understanding this dual involvement has reshaped treatment strategies by encouraging the development of medications that target both hepatic insulin resistance and pancreatic beta-cell function. Therapies like GLP-1 receptor agonists and SGLT2 inhibitors exemplify this dual-action approach. Recognizing that diabetes organ involvement extends to multiple systems reinforces the need for multifaceted treatment plans.
3. Can lifestyle changes reverse damage to body systems affected by diabetes?
While some diabetes-related damage may be irreversible, particularly in advanced cases, early intervention through lifestyle changes can significantly slow or even reverse some complications. Regular physical activity has been shown to enhance insulin sensitivity and improve liver and cardiovascular function. A nutrient-dense diet low in refined carbohydrates may alleviate metabolic stress on diabetes organs like the pancreas and kidneys. Moreover, emerging data suggest that intermittent fasting and time-restricted eating may positively influence organ repair and reduce systemic inflammation. These findings give hope that body systems affected by diabetes can regain function when supported by sustainable lifestyle habits.
4. What role does the gut microbiome play in diabetes-related organ damage?
New evidence suggests the gut microbiome has far-reaching effects on diabetes progression and the extent of diabetes effects on body systems. Alterations in gut flora have been linked to increased intestinal permeability and chronic low-grade inflammation, which can intensify insulin resistance and liver dysfunction. Short-chain fatty acids produced by healthy microbes support pancreatic health and reduce oxidative stress on various organs affected by diabetes. Probiotic and prebiotic therapies are now being investigated as adjunctive treatments to reduce organ-specific complications. These insights position the gut microbiome as a promising frontier in mitigating multi-organ damage associated with diabetes.
5. What organs does diabetes affect first, and how does progression vary between individuals?
Although the pancreas is often the first organ to exhibit dysfunction in diabetes, early signs of damage may also occur in the liver and blood vessels. Subclinical liver fat accumulation (nonalcoholic fatty liver disease) frequently coexists with early insulin resistance, even before overt diabetes is diagnosed. However, the timeline and severity of organ involvement vary greatly among individuals depending on genetics, lifestyle, and access to care. For some, the heart or kidneys may manifest early complications, while for others, peripheral neuropathy is the first symptom. Understanding this variability is crucial for personalized medicine approaches that address how diabetes affects each body system uniquely.
6. How are children’s organs affected by diabetes differently than adults’?
In pediatric cases, particularly with type 1 diabetes, organs affected by diabetes are subjected to prolonged exposure to abnormal glucose levels over a lifetime. This can accelerate complications like kidney disease and retinopathy if blood sugar is not tightly managed from a young age. Growth and hormonal changes during adolescence further complicate management, making organ protection more challenging. Additionally, psychological stress and social stigma in children and teens can indirectly worsen glycemic control, impacting long-term organ function. Pediatric care must therefore emphasize education, psychological support, and early screening for body systems affected by diabetes.
7. Are there differences in how men and women experience diabetes effects on body systems?
Yes, research indicates that biological sex may influence the way diabetes affects different organs and systems. For instance, women with diabetes often have a higher relative risk for cardiovascular disease compared to men, possibly due to differences in hormonal protection and lipid metabolism. Men, on the other hand, may experience more severe liver involvement earlier in disease progression. Hormonal fluctuations in women—such as during pregnancy or menopause—can also shift how diabetes organ damage presents, affecting insulin sensitivity and vascular integrity. These sex-specific trends highlight the importance of tailoring diabetes management to individual physiological profiles.
8. How does aging influence the vulnerability of organs affected by diabetes?
Aging compounds the impact of diabetes on organ systems, making older adults particularly vulnerable to complications. As the body ages, natural regenerative capacity diminishes, which means organs like the heart, kidneys, and brain have reduced resilience to metabolic stress. The cumulative burden of oxidative damage and chronic inflammation further weakens these body systems affected by diabetes. Moreover, older adults are more likely to have comorbidities, which can mask or worsen diabetes symptoms. Care plans for aging individuals should focus on organ preservation, functional independence, and monitoring for subtle signs of multi-organ involvement.
9. Are there any promising technologies for monitoring the progression of diabetes organ damage?
Yes, several innovative technologies are emerging to track how diabetes affects various organs with greater precision. Continuous glucose monitors (CGMs) have revolutionized real-time glucose tracking, helping to minimize fluctuations that harm organs affected by diabetes. Advanced imaging techniques like MRI elastography and retinal optical coherence tomography can detect early tissue changes in the liver and eyes, respectively. Biomarker-based blood tests are also being developed to assess inflammation, fibrosis, and organ-specific stress in real time. These tools are pivotal in assessing diabetes effects on body systems before irreversible damage occurs, allowing for earlier and more personalized interventions.
10. What future treatments are being developed to protect body systems affected by diabetes?
Ongoing research is targeting the root mechanisms of diabetes organ damage rather than just glucose levels. Therapies aimed at mitochondrial health, fibrosis prevention, and immune modulation are showing promise in animal and early human trials. Gene-editing technologies like CRISPR are being explored to repair insulin-producing pancreatic cells or regulate liver metabolism more effectively. Additionally, artificial pancreas systems and smart insulin delivery technologies may optimize glucose control in ways that directly reduce long-term damage to organs affected by diabetes. The future of diabetes treatment lies in understanding how deeply interconnected all body systems are—and intervening at the systemic level rather than isolating symptoms.
Conclusion: Embracing a Holistic View of Diabetes and Organ Health
The evolving landscape of diabetes research reveals a condition that extends far beyond its textbook definitions. What organs does diabetes affect? The answer, supported by a growing body of evidence, is nearly all of them. From the pancreas and liver to the brain, eyes, kidneys, and heart, diabetes casts a wide net of impact, often quietly and insidiously. Recognizing this interconnectedness is critical not only for effective treatment but also for prevention and patient education.
Understanding whether diabetes is a disease of the pancreas or liver opens the door to broader insights about systemic pathology and organ crosstalk. Likewise, investigating diabetes effects on body systems helps clinicians and researchers prioritize holistic care strategies. Emerging therapies that go beyond glucose control—targeting inflammation, hormonal regulation, and organ-specific complications—are ushering in a new era of comprehensive diabetes management.
As we move forward, continued exploration of the organs affected by diabetes will be essential in reducing the burden of this global epidemic. With precision medicine, early detection technologies, and interdisciplinary care, there is growing hope that we can not only manage but also mitigate the far-reaching consequences of this chronic disease. Embracing a full-body perspective allows us to respond more thoughtfully, care more effectively, and ultimately improve the lives of those living with diabetes.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Everything You Need to Know About Diabetes
Effects of diabetes on the body and organs
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.