Introduction: Why Evolving Diabetes Criteria Matter More Than Ever
Diabetes, in all its forms, continues to be one of the most pressing public health concerns worldwide. As both incidence and awareness increase, so too does the need for more refined, precise, and universally accepted diagnostic frameworks. The evolution of diabetes diagnosis criteria is not simply a technical shift within endocrinology but a fundamental transformation that affects clinical outcomes, treatment strategies, public health policies, and individual lives. With ongoing research reshaping our understanding of the disease’s pathophysiology, biomarkers, and genetic underpinnings, it has become imperative to reassess how we define, test for, and manage both type 1 and type 2 diabetes. This article explores the most up-to-date research on diagnostic guidelines, addressing the criteria for diagnosing diabetes mellitus in its multiple forms, while also evaluating emerging innovations in testing and their implications for treatment.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
Understanding the Foundation: Traditional Diagnostic Criteria for Diabetes Mellitus
To appreciate how modern approaches are reshaping the landscape, one must first understand the long-standing standards for diabetes mellitus diagnosis. Historically, the diagnostic criteria for diabetes mellitus have been anchored in blood glucose metrics. A fasting plasma glucose (FPG) level of 126 mg/dL (7.0 mmol/L) or higher, or a 2-hour plasma glucose level of 200 mg/dL (11.1 mmol/L) during an oral glucose tolerance test (OGTT), has been used to confirm the presence of diabetes. Additionally, a random plasma glucose of 200 mg/dL or greater in a person with symptoms of hyperglycemia or hyperglycemic crisis has been considered diagnostic. Hemoglobin A1c (HbA1c), reflecting average blood glucose over approximately three months, has also become a staple criterion, with a threshold of 6.5% or more commonly indicating diabetes.
While these diagnostic tools have been invaluable, they are not without limitations. Variability in lab methodologies, physiological differences across populations, and the challenge of identifying early-stage or atypical diabetes cases have necessitated refinement. The criteria for DM diagnosis must now integrate newer tools, biomarkers, and understanding of disease heterogeneity. This shift is especially urgent for improving early identification and intervention strategies.
Refining the Type 1 Diabetes Diagnosis Criteria in the Modern Era
Type 1 diabetes, characterized by autoimmune destruction of pancreatic beta cells, has traditionally been diagnosed in children or adolescents, although adult-onset type 1 diabetes is increasingly recognized. The diagnosis relies heavily on identifying high blood sugar levels consistent with hyperglycemia and the absence of insulin resistance. Yet, with overlapping symptoms and glucose profiles, distinguishing type 1 from type 2 diabetes—especially in adults—can be challenging.
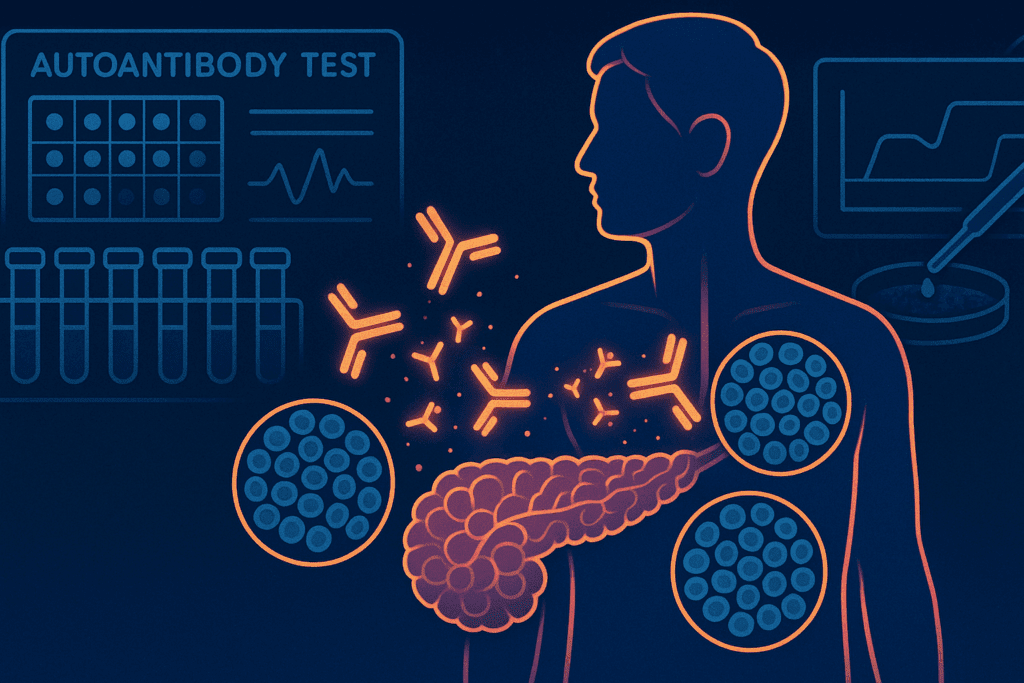
Modern type 1 diabetes diagnosis criteria increasingly emphasize immunological and genetic markers. Type 1 diabetes lab tests now include autoantibody panels that detect islet cell antibodies (ICA), glutamic acid decarboxylase antibodies (GAD65), insulin autoantibodies (IAA), and others. These markers help distinguish autoimmune diabetes from type 2, especially in ambiguous cases. A type 1 diabetes blood test that reveals multiple autoantibodies can confirm the diagnosis even before clinical symptoms manifest, especially in individuals with a family history.
Additionally, the concept of “staging” type 1 diabetes is gaining traction. Stage 1 involves the presence of two or more islet autoantibodies with normal blood sugar levels, while stage 2 includes dysglycemia without symptoms. Stage 3 represents the traditional clinical presentation. This nuanced framework allows for earlier detection and potential prevention strategies, shifting the paradigm from reactive to proactive care. The increasing role of type 1 DM testing in asymptomatic individuals underscores the expanding scope of diagnostic strategies.
Type 1 Diabetes Blood Sugar Levels: A Closer Look at Laboratory Thresholds and Monitoring
Understanding type 1 diabetes blood sugar levels is critical not only for diagnosis but also for ongoing management. Individuals with type 1 diabetes typically present with significantly elevated glucose levels due to absolute insulin deficiency. Classic symptoms—polyuria, polydipsia, weight loss, and fatigue—are accompanied by blood glucose values that exceed the diagnostic thresholds mentioned earlier.
However, emerging research suggests that variability in blood sugar levels, especially in the preclinical stages, can offer important diagnostic cues. Continuous glucose monitoring (CGM) systems are now used in both research and clinical settings to detect early fluctuations in glucose that traditional blood tests might miss. For individuals with positive autoantibody profiles, even subtle deviations from normoglycemia may indicate progression toward clinical diabetes.
In clinical contexts, type 1 diabetes high blood sugar levels often exceed 250 mg/dL and are accompanied by ketosis or diabetic ketoacidosis (DKA) at presentation. Yet, a more nuanced understanding of these thresholds is necessary, especially as more cases are identified at earlier stages through screening and family history evaluations. The role of the diabetes 1 test now extends beyond emergency diagnosis to early, pre-symptomatic detection.
Emerging Innovations in Type 1 Diabetes Lab Tests and Genetic Screening
Type 1 diabetes lab tests have evolved significantly, encompassing more than just glucose and HbA1c measurements. In addition to autoantibody detection, researchers are now exploring HLA genotyping and polygenic risk scores to predict susceptibility. Genetic testing for markers such as HLA-DR3/DR4 is increasingly used in research and sometimes in clinical trials to identify individuals at high risk for developing type 1 diabetes.
Moreover, experimental biomarkers such as zinc transporter 8 autoantibodies (ZnT8A) and C-peptide levels are becoming central to the diagnostic and prognostic process. C-peptide, a byproduct of insulin production, can indicate residual beta cell function and help distinguish between type 1 and type 2 diabetes. In some individuals, particularly those diagnosed later in life, these lab tests clarify ambiguous presentations and guide decisions on insulin initiation and long-term management.
These emerging diagnostic tools support a more personalized approach to treatment. Medicine for diabetes type 1 is becoming increasingly tailored to the individual’s genetic and immunological profile. The expansion of type 1 diabetes labs and their integration into mainstream care marks a turning point in precision medicine.
Rethinking Type 2 Diabetes Diagnosis Criteria in a Complex Epidemiological Landscape
While type 2 diabetes remains the most common form of diabetes worldwide, its diagnostic challenges are just as nuanced. Traditionally, type 2 diabetes diagnosis criteria have overlapped with general diagnostic criteria for diabetes, including fasting glucose, OGTT, and HbA1c levels. However, emerging data suggests these thresholds may not capture early metabolic dysfunction or account for ethnic and genetic variability.
One of the main concerns with existing criteria for diabetes type 2 is their inability to identify prediabetes or early insulin resistance in asymptomatic individuals. Consequently, more refined diagnostic algorithms incorporating insulin sensitivity markers, adipokines, and inflammatory biomarkers are under investigation. Moreover, t2dm diagnostic criteria are increasingly contextualized within broader cardiometabolic risk profiles.
Recent studies emphasize the value of combining glycemic data with imaging technologies and metabolic panels to assess beta cell function and visceral adiposity. Such integrative approaches aim to personalize diagnosis, moving beyond a one-size-fits-all model. In light of these insights, the criteria for diagnosing diabetes mellitus type 2 are being reevaluated to accommodate the complex interplay of genetic, lifestyle, and environmental factors.
The Role of A1c and the Challenge of Ethnic Variability in Diagnosis
The HbA1c test remains one of the most widely used tools in both type 1 and type 2 diabetes diagnosis criteria due to its convenience and long-term representation of blood glucose levels. However, it is not without controversy. Several studies have highlighted disparities in HbA1c readings among different ethnic groups, potentially leading to under- or over-diagnosis.
This discrepancy raises critical questions about the reliability of A1c as a standalone diagnostic measure. For instance, individuals of African, Mediterranean, or Southeast Asian descent may have hemoglobin variants that affect the accuracy of the test. As such, relying solely on A1c could misrepresent true glycemic status, prompting a reconsideration of how diabetes guidelines for diagnosis are applied across populations.
To address this, new guidelines suggest using a combination of tests—fasting glucose, OGTT, and A1c—especially in populations with known biological variability. These combined measures provide a more holistic view of glycemic control and reduce the likelihood of misclassification. The move toward comprehensive screening models reflects a more inclusive and accurate interpretation of diabetes 2 diagnosis criteria.

Early Screening and Prevention: Redefining Diagnostic Timing
Another critical area where research is reshaping practice is in the timing of diagnosis. Traditional models focused on diagnosing diabetes only after symptoms appeared or glucose levels exceeded established thresholds. However, mounting evidence suggests that by the time overt hyperglycemia occurs, significant beta cell loss or insulin resistance has already developed.
As a result, there is growing support for earlier screening in high-risk populations, including those with a family history, obesity, or gestational diabetes history. These efforts aim to identify individuals during the so-called “silent phase” of the disease, where intervention may delay or prevent progression. The evolving diabetes diagnosis criteria increasingly support the use of risk calculators, genetic profiling, and longitudinal monitoring in clinical settings.
In pediatric populations, early diagnosis is particularly critical given the rapid onset and potential complications associated with both type 1 and type 2 diabetes. Here, the criteria for diagnosing diabetes must also account for age-specific glucose metabolism patterns, growth-related variability, and the psychosocial impacts of chronic disease in youth.
Therapeutic Implications: How Refined Diagnosis Enhances Type 1 Diabetes Treatment
As our ability to diagnose type 1 diabetes improves, so too does our ability to tailor its treatment. Traditional insulin therapy remains the cornerstone of diabetes mellitus type 1 treatment. However, advancements in diagnostics now enable more precise insulin regimens based on residual beta cell function, genetic markers, and even immune profiles.
Personalized approaches to how to treat diabetes 1 are emerging, including immunotherapy trials aiming to preserve beta cell function in newly diagnosed individuals. The ability to detect the disease in its earliest stages allows for enrollment in such trials before irreversible damage occurs. These developments hold promise for altering the disease trajectory entirely.
Moreover, improved diagnostic accuracy reduces the risk of misclassification, which can lead to inappropriate therapy. For instance, prescribing oral hypoglycemics for a misdiagnosed type 1 patient can delay proper insulin initiation and increase complication risks. Thus, the stakes in refining the type 1 diabetes diagnosis criteria are both clinically and personally significant.
Toward a Global Consensus: Harmonizing Guidelines Across Health Systems
The diversity of healthcare systems worldwide means that diagnostic criteria for diabetes mellitus vary, sometimes significantly, by region. Organizations like the American Diabetes Association (ADA), World Health Organization (WHO), and International Diabetes Federation (IDF) each publish diagnostic frameworks that, while largely aligned, still differ in thresholds or emphasis.
Global harmonization of diabetes criteria is essential for ensuring consistent care and comparative research across borders. This is particularly relevant as diabetes prevalence grows in low- and middle-income countries, where diagnostic resources may be limited. Standardizing tests like the type 1 diabetes blood test and the OGTT can help streamline care pathways and facilitate international data sharing.
Additionally, initiatives to expand access to laboratory diagnostics, especially in under-resourced areas, are key to implementing refined criteria effectively. Integrating updated diabetes guidelines for diagnosis into electronic health records and mobile health tools can also improve real-time clinical decision-making.
Frequently Asked Questions (FAQ): Redefining Diabetes Diagnosis Criteria
1. How are recent advances changing the way type 1 diabetes is diagnosed in adults?
Historically, type 1 diabetes was primarily associated with children, but newer studies reveal a significant number of adult-onset cases that were previously misdiagnosed as type 2. With refined diagnostic criteria for diabetes mellitus, clinicians now incorporate immunological and genetic testing in adults, especially when traditional indicators are ambiguous. A type 1 diabetes blood test that includes autoantibody detection is increasingly used to identify latent autoimmune diabetes in adults (LADA). These cases often present with milder symptoms and lower type 1 diabetes blood sugar levels at onset, complicating the diagnostic process. As such, type 1 DM testing in adults now plays a vital role in ensuring the right classification and in selecting the correct medicine for diabetes type 1, such as early insulin initiation rather than oral agents.
2. Why is it important to look beyond blood sugar levels when diagnosing type 2 diabetes?
Although blood sugar remains a cornerstone of diabetes diagnosis criteria, relying solely on glucose metrics may miss early metabolic disturbances. Many individuals exhibit insulin resistance or pancreatic beta-cell dysfunction long before exceeding blood sugar thresholds. That’s why new criteria for diabetes type 2 increasingly include metabolic markers such as fasting insulin, C-peptide levels, and triglyceride-to-HDL ratios. These provide a deeper insight into underlying dysfunctions that may precede traditional type 2 diabetes diagnosis criteria. Advanced screening offers a preventive window to implement lifestyle changes or pharmacological interventions before the condition progresses.
3. How can genetics influence the diagnostic criteria for type 1 and type 2 diabetes mellitus?
Genetic profiling is playing a growing role in refining the diagnostic criteria for diabetes. For type 1, certain HLA haplotypes significantly increase the likelihood of developing the condition, prompting early surveillance in high-risk individuals. For type 2, polygenic risk scores are being developed to help predict susceptibility, especially in ethnically diverse populations where diabetes 2 diagnosis criteria may not apply uniformly. This shift supports a more personalized approach to diabetes criteria, incorporating genetic context to better match diagnostic tools to individual risk profiles. With the advancement of precision medicine, understanding genetic predispositions could eventually redefine how and when to implement a diabetes 1 test or a type 1 diabetes blood test.
4. Are current diagnostic guidelines adequate for identifying diabetes in children and adolescents?
The existing diabetes guidelines for diagnosis may not fully capture the unique metabolic dynamics of children and adolescents. Youth can experience rapid fluctuations in type 1 diabetes blood sugar levels, and their presentation often includes diabetic ketoacidosis (DKA), which may skew initial assessments. Moreover, the increasing incidence of type 2 diabetes among adolescents adds complexity to applying criteria for DM diagnosis in pediatric populations. Type 1 diabetes lab tests must be performed alongside clinical evaluations of weight, acanthosis nigricans, and family history to ensure appropriate classification. Updating diagnostic criteria for diabetes mellitus in youth is essential to reflect both physiological differences and the rising trend of early-onset diabetes.
5. How do social determinants of health impact timely diabetes diagnosis?
Social factors such as access to healthcare, education, and socioeconomic status significantly influence how and when individuals are diagnosed. Communities with limited access to regular screenings may not meet the diagnostic criteria for type 2 diabetes mellitus until the disease has advanced. Similarly, the availability of comprehensive type 1 DM testing may be restricted in resource-limited settings, delaying proper treatment. Addressing these disparities means expanding access to diagnostics like the diabetes 1 test and integrating community health programs. Policymakers must also ensure that diabetes mellitus diagnosis criteria are communicated clearly to underserved populations through culturally competent education.
6. What are the potential pitfalls of over-reliance on A1c in diabetes diagnosis?
While A1c is a convenient and widely accepted component of diabetes criteria, it does not always provide an accurate picture across all populations. Conditions such as anemia, kidney disease, or hemoglobinopathies can alter A1c values, leading to under- or overdiagnosis. In these situations, relying on fasting glucose or an oral glucose tolerance test (OGTT) may offer better diagnostic clarity. Given these nuances, the criteria for diagnosing diabetes mellitus type 2 now often recommend confirming abnormal A1c values with an additional test. This multifaceted approach is part of a broader shift toward more robust and inclusive diagnostic criteria for diabetes.
7. How are researchers working to detect diabetes earlier, even before symptoms develop?
The medical community is increasingly focused on identifying diabetes in its silent or preclinical phase. Studies now target individuals with a family history of type 1 diabetes using autoantibody screenings and genetic risk scoring to flag risk before clinical symptoms arise. Type 1 diabetes labs are being used for longitudinal tracking in children with high-risk profiles, even when their blood sugar levels remain normal. Similarly, researchers are exploring how early insulin resistance can be identified through fasting insulin and HOMA-IR assessments, refining t2dm diagnostic criteria for early-stage detection. This preemptive strategy allows for earlier interventions, including trials in immunomodulation for delaying the onset of autoimmunity or lifestyle changes for those at risk of type 2 diabetes.
8. What role do continuous glucose monitoring (CGM) systems play in refining diagnosis?
CGMs provide a dynamic profile of blood glucose trends, offering insights that static tests often miss. They are particularly useful in borderline cases where blood sugar levels type 1 or 2 fluctuate but remain near diagnostic cutoffs. CGMs help identify postprandial spikes, nighttime hypoglycemia, or dawn phenomenon, which could inform more nuanced interpretations of diabetes mellitus diagnosis criteria. For patients suspected of type 1 diabetes, CGM can reveal patterns consistent with high glycemic variability, even in the absence of classic symptoms. Integrating CGM data into the diagnostic workflow is a forward-looking strategy to fine-tune both type 1 and type ii diabetes diagnosis criteria.
9. How does early diagnosis affect long-term treatment outcomes for type 1 diabetes?
Early detection of type 1 diabetes can significantly improve clinical outcomes by preserving residual beta-cell function. When diagnosis occurs before significant insulin deficiency, patients may require lower doses of insulin and have better glycemic control over time. This is crucial because certain forms of medicine for diabetes type 1 are more effective when endogenous insulin production is still present. Moreover, early detection through type 1 diabetes lab tests allows patients to engage in structured education and technology use—such as insulin pumps or CGMs—sooner. With more refined type 1 diabetes diagnosis criteria, long-term complications like nephropathy or retinopathy may be delayed or prevented entirely.
10. Could emerging biomarkers replace traditional glucose-based testing in the future?
Biomarker research is at the forefront of efforts to move beyond glucose-centric diagnostics. Molecules such as adiponectin, proinsulin-to-insulin ratios, and inflammatory cytokines are being studied for their potential role in early disease identification. These markers could revolutionize the criteria for diagnosing diabetes by offering earlier, more sensitive detection methods. If validated, they might complement or even replace existing tests like the type 1 diabetes blood test or HbA1c for specific populations. As research continues, the diagnostic criteria for type 2 diabetes and type 1 alike may evolve to reflect a broader biochemical understanding of the disease process, leading to earlier, more personalized treatment pathways.
Conclusion: A New Era in Diabetes Diagnosis and Treatment Begins with Better Definitions
The evolution of diagnostic criteria for diabetes marks a critical shift in how we understand, identify, and manage both type 1 and type 2 diabetes. With improved clarity in the criteria for DM diagnosis and expanded access to sophisticated testing technologies, healthcare providers are better equipped to offer timely, precise, and effective care. As research continues to unveil novel biomarkers, genetic indicators, and preclinical stages of the disease, the diagnostic process is transitioning from a reactive model to a proactive one.
Whether through enhanced type 1 diabetes lab tests or redefined thresholds for type 2 diabetes diagnosis criteria, the trajectory of diabetes care is now one of personalization and prevention. By integrating the latest evidence into global guidelines and clinical practice, we can reduce misdiagnosis, ensure early intervention, and ultimately improve outcomes for millions worldwide. As we continue redefining diabetes diagnosis criteria, we lay the foundation for a future in which the burden of this chronic disease is met not only with empathy and insight but also with the full power of scientific innovation.
Further Reading:
Redefining the Diagnosis of Diabetes Using Glycated Hemoglobin
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.