Understanding the Urgency: Why Modern Care Plans Matter More Than Ever
Type 2 diabetes is no longer just a chronic condition requiring medication and routine monitoring; it is now recognized as a complex, multifactorial disease that demands a comprehensive and evolving approach. With more than 400 million people affected globally, the need for an evidence-based care plan for type 2 diabetes has never been more pressing. Unlike in the past when treatment relied predominantly on glycemic control through pharmaceuticals, today’s care plans are increasingly multidimensional. They integrate lifestyle changes, psychological support, education, technological innovation, and emerging therapeutic interventions. This shift reflects a growing body of scientific evidence showing that holistic, personalized strategies lead to better outcomes—not just in glucose regulation but also in quality of life, cardiovascular health, and long-term disease management.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
What makes this transformation particularly significant is its alignment with the realities of patient diversity and individualized needs. Every case of diabetes mellitus type 2 is shaped by unique genetic, environmental, and behavioral factors, which means that a one-size-fits-all treatment model is both outdated and inadequate. New research emphasizes tailoring care plans to reflect the person’s stage of disease progression, comorbidities, socioeconomic context, and psychosocial challenges. In doing so, clinicians are now empowered to intervene more precisely and more effectively. The resulting diabetes mellitus type 2 care plan is more than a set of instructions; it is a dynamic, patient-centered strategy aimed at proactive disease reversal, risk mitigation, and overall wellness.
Evolution of the Traditional Diabetes Mellitus Type 2 Care Plan
Historically, the care plan for diabetes mellitus 2 centered around diet, exercise, and pharmacologic agents, with blood glucose levels as the primary metric of success. While these pillars remain vital, emerging research reveals that limiting the focus solely to these factors overlooks essential contributors to disease progression. For example, stress, sleep quality, and even gut microbiota composition have been linked to insulin resistance and metabolic dysfunction. These insights have led to a redefinition of what constitutes a comprehensive diabetes care plan in clinical practice.
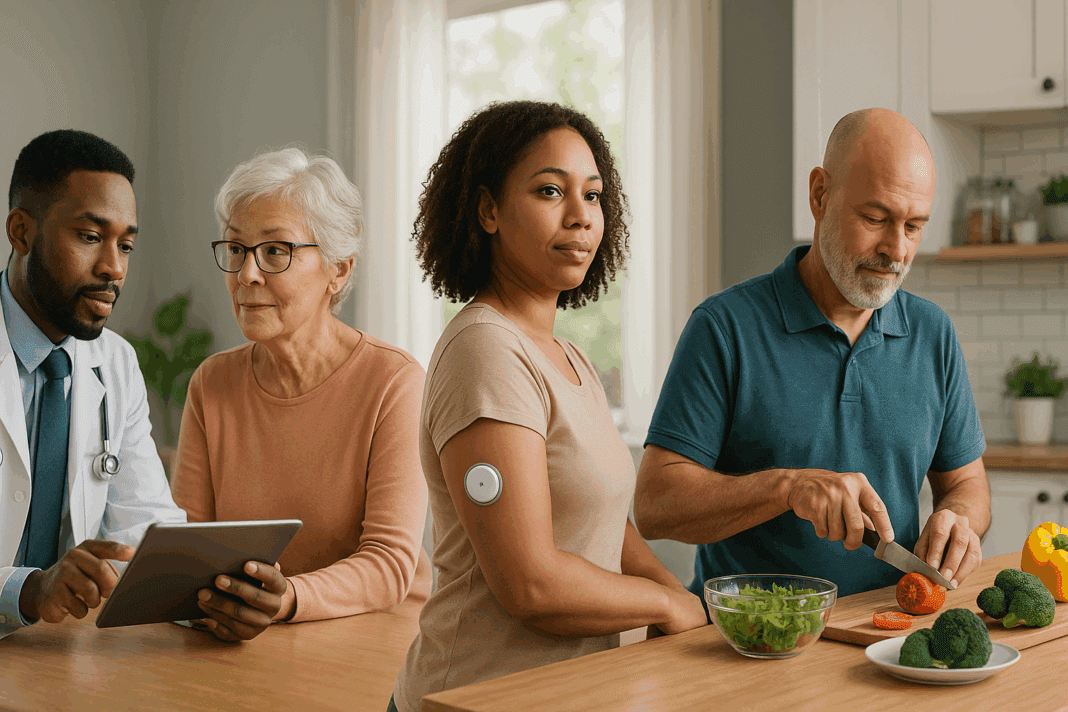
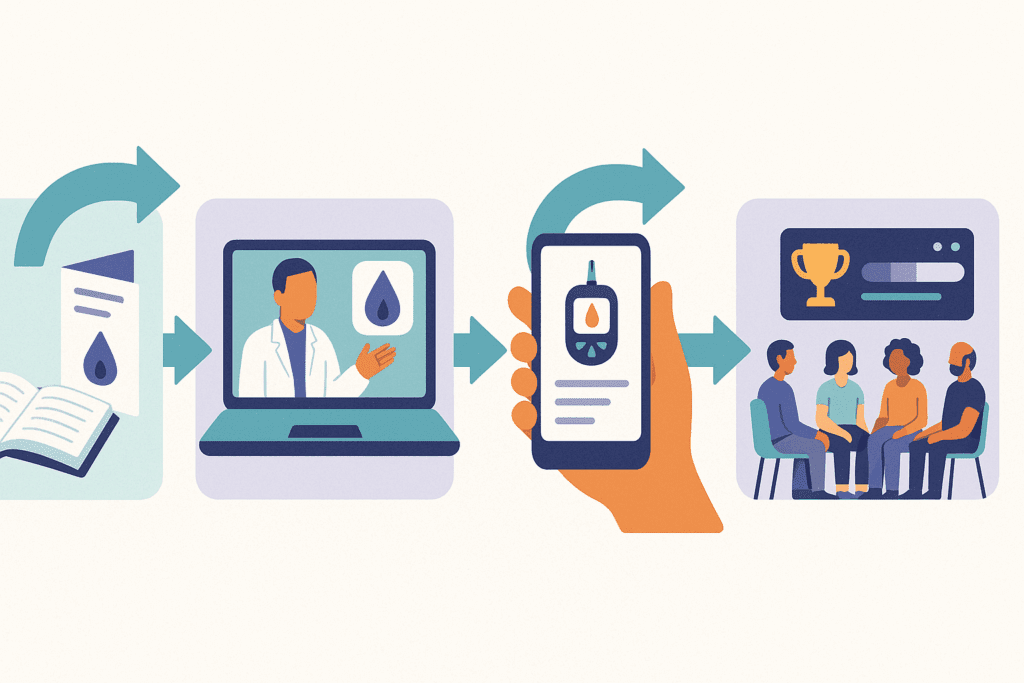
Today, evidence-based care incorporates frequent assessments of both physiological and behavioral parameters. Clinicians are encouraged to screen for depression, sleep apnea, food insecurity, and medication adherence issues, all of which can subtly undermine treatment efficacy. The diabetes mellitus type 2 care plan now routinely includes patient education on carbohydrate quality, meal timing, and mindful eating habits. Digital tools such as continuous glucose monitors and mobile apps for lifestyle tracking are also becoming standard components of care. These tools not only support real-time data collection but also foster patient engagement and accountability, both of which are critical for long-term success.
Crucially, the evolution of care plans has been informed by longitudinal studies and randomized controlled trials that demonstrate how these interventions tangibly affect health outcomes. For instance, the Look AHEAD (Action for Health in Diabetes) study showed that intensive lifestyle interventions could lead to sustained weight loss and improved cardiovascular markers. This data-driven perspective ensures that the modern care plan for type 2 diabetes is not simply aspirational but grounded in proven clinical value.
The Role of Personalized Nutrition in Optimizing Outcomes
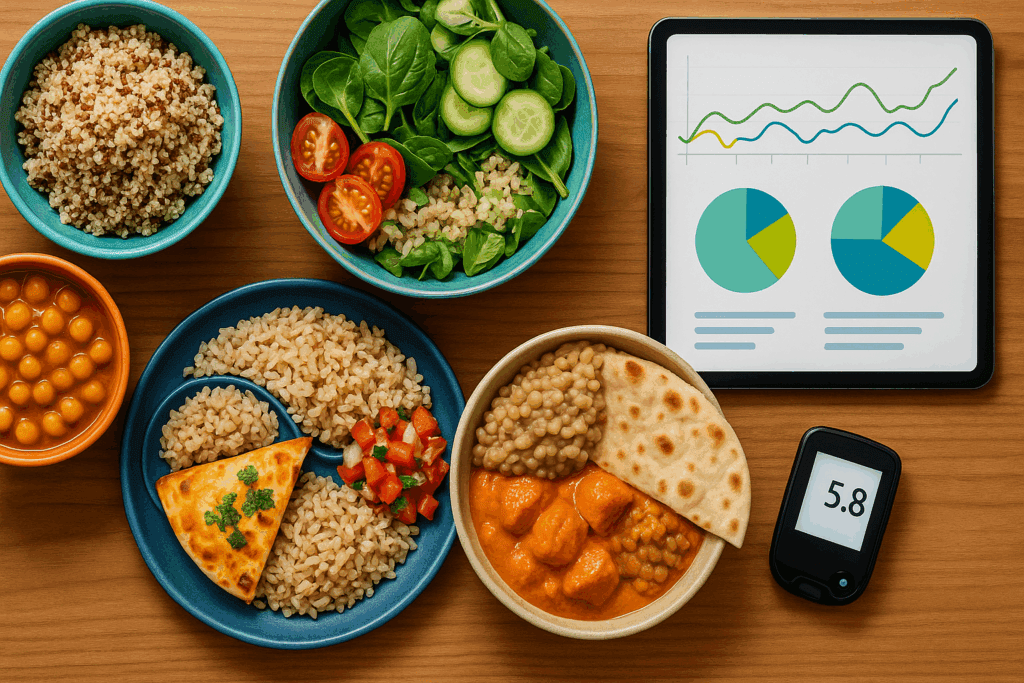
One of the most exciting frontiers in diabetes care is the use of personalized nutrition to enhance glycemic control. While generalized dietary guidelines have historically advised carbohydrate moderation and increased fiber intake, newer research suggests that individual glycemic responses to foods vary widely, even among people with similar demographics and health status. This finding has propelled the integration of personalized dietary planning into the care plan for type 2 diabetes.
Microbiome analysis, genetic testing, and continuous glucose monitoring now offer clinicians tools to tailor dietary interventions with unprecedented precision. A person whose glucose levels spike with oats but remain stable with quinoa, for example, can adjust their diet based on direct evidence rather than generic advice. Additionally, time-restricted eating and intermittent fasting protocols are being investigated as viable adjuncts to standard nutritional guidance, particularly for patients struggling with insulin resistance.
Moreover, culturally appropriate meal planning has gained prominence as a determinant of dietary adherence. Research has shown that when dietary advice aligns with a patient’s cultural preferences and traditions, compliance improves markedly. Thus, a well-designed diabetes mellitus type 2 care plan is not only evidence-based but also inclusive, practical, and empathetic to individual preferences. This tailored approach helps break down barriers to dietary change and empowers patients to take ownership of their health journey.

Integrating Behavioral and Mental Health Support into Diabetes Care
Psychological well-being plays a critical yet often underappreciated role in diabetes management. Depression, anxiety, and diabetes distress can significantly interfere with treatment adherence, dietary choices, and self-monitoring behaviors. As such, mental health assessment is now considered a best practice within any robust care plan for diabetes mellitus 2. This holistic approach recognizes that optimal glycemic control cannot be achieved in isolation from emotional and psychological factors.
Cognitive behavioral therapy (CBT), mindfulness training, and diabetes-specific support groups are increasingly recommended as adjunctive treatments. These interventions have demonstrated efficacy in reducing hemoglobin A1c levels, improving mood, and enhancing treatment compliance. For example, studies show that patients who participate in structured mental health programs report fewer diabetes-related complications and hospitalizations.
Additionally, providers are being trained to identify signs of burnout and psychological resistance in their patients. This preventive strategy aims to intervene early before disengagement or non-compliance sets in. By weaving mental health considerations into the broader care plan for type 2 diabetes, providers are better equipped to support the full spectrum of patient needs. This integrative care model reflects a growing recognition that health is not merely the absence of disease but the presence of physical, emotional, and social well-being.
Pharmacologic Innovations and Precision Medicine in Treatment Plans
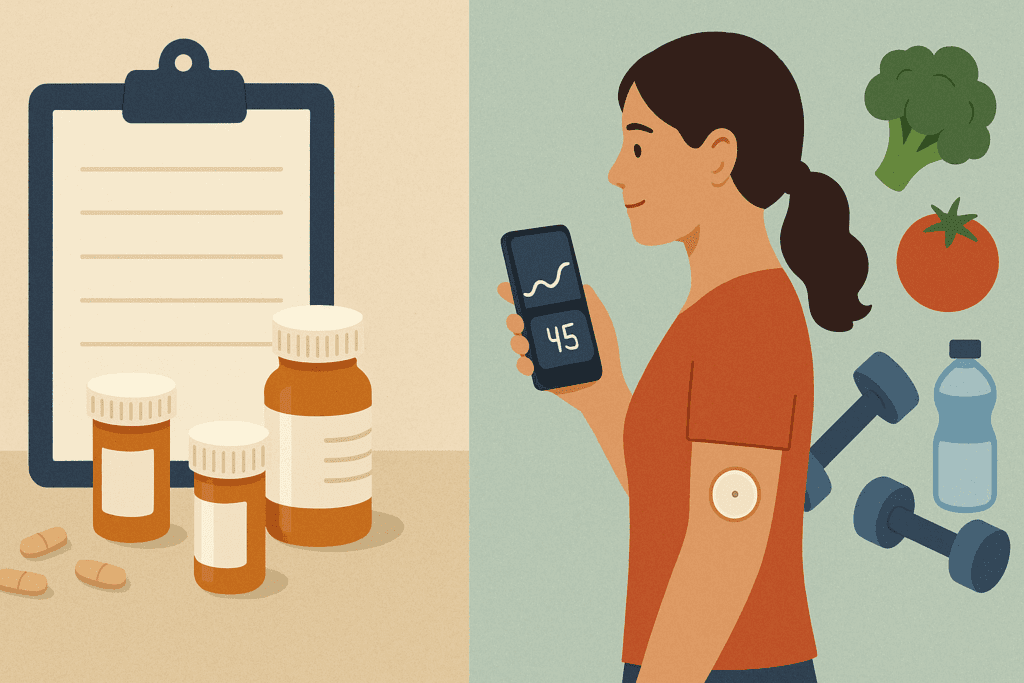
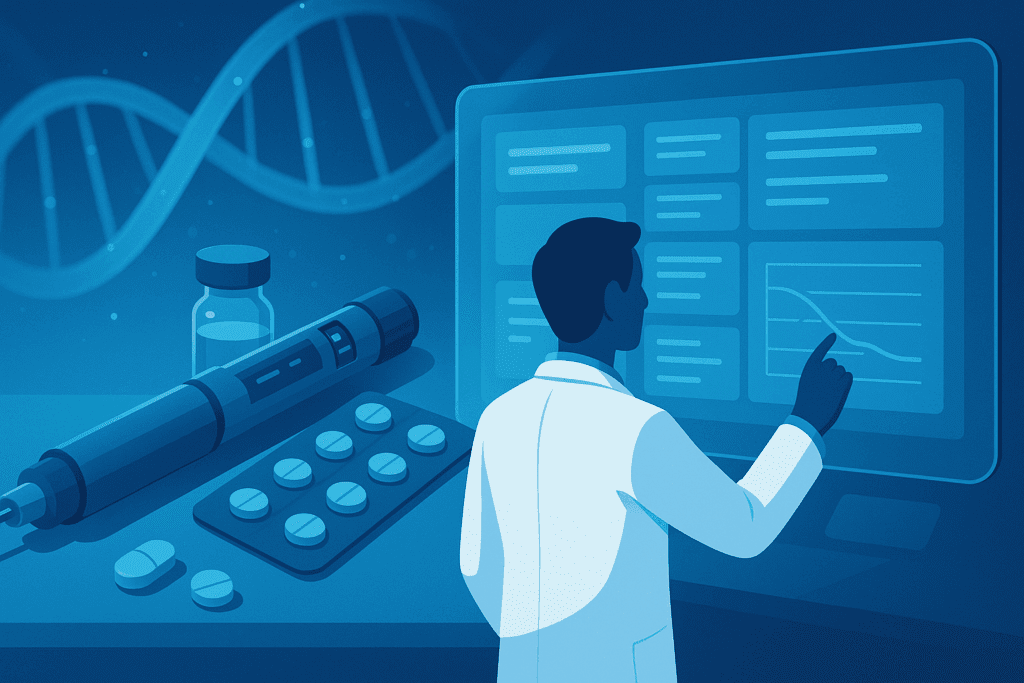
The pharmacologic landscape for type 2 diabetes has expanded considerably in recent years. In addition to traditional agents like metformin and sulfonylureas, a new generation of medications has emerged, including GLP-1 receptor agonists, SGLT2 inhibitors, and dual-action therapies that target multiple metabolic pathways. These innovations provide clinicians with greater flexibility to design pharmacologic regimens that are both effective and well-tolerated.
New research suggests that certain drug classes may confer benefits beyond glycemic control, such as cardiovascular protection, weight reduction, and renal function preservation. This makes them especially valuable additions to the modern diabetes mellitus type 2 care plan. For instance, SGLT2 inhibitors have been shown to reduce hospitalization rates for heart failure in patients with coexisting cardiovascular disease. Meanwhile, GLP-1 receptor agonists not only help regulate blood sugar but also assist in appetite control and weight loss, which are key goals in managing obesity-related diabetes.
The advent of pharmacogenomics—the study of how genetic factors influence drug response—is poised to further revolutionize treatment. By analyzing genetic markers, clinicians can predict how a patient will respond to specific medications, thereby minimizing trial-and-error prescribing. This precision medicine approach ensures that the care plan for diabetes mellitus 2 is not only reactive but also proactive, aligning treatment strategies with individual biological profiles for optimal outcomes.

The Emerging Role of Technology in Diabetes Self-Management
Technology has become an indispensable component of diabetes care, reshaping how patients interact with their condition and how clinicians deliver support. From wearable devices to cloud-based data platforms, digital innovations are enhancing both self-monitoring and provider oversight. Continuous glucose monitors (CGMs), for example, offer real-time glucose tracking that helps patients understand the impact of food, stress, and activity on their blood sugar levels.
Incorporating these tools into the care plan for type 2 diabetes allows for dynamic feedback loops, where patients can make immediate adjustments based on real-time information. This capability supports more nuanced decision-making and fosters a sense of control and empowerment. Furthermore, mobile applications that track dietary intake, exercise routines, medication adherence, and mood are proving valuable in sustaining long-term behavioral change.
Telemedicine has also emerged as a vital conduit for care continuity, especially in the wake of the COVID-19 pandemic. Virtual consultations allow for timely intervention, particularly in underserved or remote areas where in-person care may be limited. These platforms facilitate medication adjustments, nutritional counseling, and mental health check-ins without the logistical barriers of traditional healthcare delivery. When embedded into a comprehensive diabetes mellitus type 2 care plan, technology not only enhances access and efficiency but also strengthens the therapeutic alliance between patients and providers.
Reframing Diabetes Education for Lasting Impact
Education remains a cornerstone of effective diabetes care, but modern approaches are moving beyond didactic instruction to emphasize interactive, patient-centered learning. Traditional models often relied on one-size-fits-all information delivery, which failed to account for diverse learning styles, health literacy levels, and cultural contexts. In contrast, contemporary diabetes education is increasingly tailored, experiential, and participatory.
Empowerment-based models encourage patients to co-create their care strategies, ask questions, and set realistic goals. Group-based education sessions, peer mentoring, and culturally adapted curricula are gaining popularity for their ability to foster community and shared accountability. By incorporating behavior change theories, educators can also better understand the psychological barriers to adoption and retention of healthy habits.
Inclusion of digital modules, gamification techniques, and interactive video content further enriches the educational experience. These tools make complex concepts more accessible and reinforce learning through engagement. When integrated into a larger care plan for diabetes mellitus 2, such educational innovations play a pivotal role in translating knowledge into action. The goal is not merely to inform but to transform—to enable individuals to live confidently and competently with their condition.

Addressing Health Disparities Through Inclusive Care Models
Despite advancements in diabetes management, significant disparities persist in outcomes across racial, ethnic, and socioeconomic lines. Research shows that marginalized populations often experience delayed diagnosis, limited access to high-quality care, and poorer treatment adherence. These inequities underscore the importance of designing care plans that are inclusive, equitable, and responsive to the unique challenges faced by diverse communities.
Community-based interventions have shown promise in bridging these gaps. Initiatives that train community health workers, provide culturally sensitive educational materials, and offer mobile clinics are helping to improve access and trust. Additionally, language translation services, transportation assistance, and flexible scheduling can make care more accessible for those with structural barriers.
Health systems are also being urged to collect and analyze demographic data to identify at-risk groups and tailor interventions accordingly. This data-driven approach ensures that the care plan for diabetes mellitus 2 is not only personalized at the individual level but also equitable at the population level. By aligning medical strategies with social determinants of health, the healthcare community can work toward truly inclusive diabetes management.
Frequently Asked Questions: Enhancing the Modern Care Plan for Type 2 Diabetes
1. How can social support systems strengthen the care plan for type 2 diabetes?
Social support is an often-overlooked element that can significantly strengthen a care plan for type 2 diabetes. Family members, close friends, and peer networks can improve patient adherence to treatment goals by offering emotional encouragement, accountability, and even practical help with food preparation or physical activity. Recent research shows that when patients with type 2 diabetes engage in structured peer-support groups, they report better glycemic control and lower diabetes-related stress. These communal spaces foster shared experiences and problem-solving, especially when managing complex self-care routines. To truly elevate a diabetes mellitus type 2 care plan, healthcare providers are increasingly recommending structured inclusion of social supports through counseling sessions, family-based interventions, and digital community platforms.
2. What role does sleep quality play in the care plan for diabetes mellitus 2?
Emerging evidence highlights the role of sleep in modulating insulin sensitivity and inflammation, both critical to managing type 2 diabetes. Poor sleep, whether due to insomnia, sleep apnea, or inconsistent sleep patterns, can directly impact glycemic control and increase the risk of metabolic dysfunction. Incorporating sleep hygiene assessments and interventions into the care plan for diabetes mellitus 2 is becoming more common in advanced clinical settings. For example, patients might undergo sleep studies or receive cognitive behavioral therapy for insomnia (CBT-I) as a supplemental part of their diabetes management. Addressing sleep quality helps to round out a more holistic diabetes mellitus type 2 care plan and may reduce the need for pharmacological escalation.
3. Are there gender-specific considerations when tailoring a diabetes mellitus type 2 care plan?
Yes, gender can influence the presentation, complications, and treatment response in type 2 diabetes, making it an important factor when creating a personalized care plan. For instance, women with diabetes are more prone to depression and cardiovascular complications, while men may be more likely to develop kidney disease. Hormonal variations also affect insulin sensitivity, particularly during menopause or with polycystic ovarian syndrome (PCOS). A gender-informed care plan for type 2 diabetes might involve additional cardiovascular screening for women or testosterone assessments for men with unexplained fatigue and metabolic issues. Understanding these nuances enables a more refined and effective care plan for diabetes mellitus 2.
4. How can financial constraints impact adherence to a care plan for type 2 diabetes?
Economic barriers are a major determinant of treatment adherence and overall health outcomes in people managing type 2 diabetes. High out-of-pocket costs for medications, glucose monitors, healthy foods, and clinic visits often result in delayed care or rationed supplies. This is why many modern diabetes mellitus type 2 care plans now include assessments of financial stability and referrals to patient assistance programs. Some healthcare systems are integrating social workers and financial counselors into diabetes clinics to help patients access community resources and subsidies. Proactively addressing these barriers ensures that the care plan for diabetes mellitus 2 remains both realistic and sustainable for patients across diverse socioeconomic backgrounds.
5. Can wearable fitness technology improve the success of a diabetes mellitus type 2 care plan?
Absolutely. Devices such as fitness trackers, smartwatches, and continuous glucose monitors (CGMs) provide real-time data that patients and providers can use to make more informed decisions. These tools enhance engagement and motivation by allowing users to track their physical activity, caloric intake, and glucose trends in relation to lifestyle choices. When integrated into a comprehensive care plan for type 2 diabetes, wearable tech offers opportunities for early intervention and ongoing adjustment based on data-driven insights. Moreover, remote monitoring through these devices enables clinicians to provide timely feedback and interventions. This tech-savvy component can help modernize a traditional care plan for diabetes mellitus 2 and support sustainable self-management.
6. What are some lesser-known dietary strategies included in personalized diabetes care plans?
Beyond conventional advice to reduce sugar and refined carbs, emerging dietary strategies focus on meal timing, macronutrient sequencing, and the gut microbiome. For instance, eating protein and fats before carbohydrates in a meal can blunt postprandial glucose spikes. Similarly, some research supports the benefits of early time-restricted feeding, where meals are consumed within an 8- to 10-hour window to align with circadian rhythms. Including fermented foods and prebiotic fibers may also improve gut flora composition and insulin sensitivity. These strategies are being incorporated into forward-thinking diabetes mellitus type 2 care plans to fine-tune nutrition without increasing dietary burden. A well-tailored care plan for type 2 diabetes can integrate these nuanced interventions based on patient readiness and clinical context.
7. How do cultural beliefs influence the success of a care plan for diabetes mellitus 2?
Cultural beliefs shape perceptions of illness, food preferences, physical activity norms, and attitudes toward medical treatment. If unaddressed, these beliefs can create friction between a healthcare provider’s recommendations and a patient’s willingness to comply. Culturally competent care involves recognizing and respecting these beliefs while collaboratively designing a diabetes mellitus type 2 care plan that incorporates culturally appropriate solutions. For example, substituting traditional high-glycemic foods with culturally familiar but lower-GI alternatives can improve both adherence and outcomes. Training providers in cultural humility and using community health workers from similar backgrounds also strengthens the care plan for diabetes mellitus 2 by building trust and promoting effective communication.
8. What long-term complications can arise from an incomplete care plan for type 2 diabetes?
An incomplete or poorly coordinated care plan for type 2 diabetes can leave patients vulnerable to a range of preventable complications, including cardiovascular disease, neuropathy, nephropathy, retinopathy, and lower limb amputations. These outcomes not only diminish quality of life but also lead to increased hospitalizations and healthcare costs. Inadequate monitoring, lack of mental health integration, and insufficient education can all contribute to suboptimal disease control. A comprehensive diabetes mellitus type 2 care plan includes regular screenings, early detection protocols, and coordinated referrals to specialists when needed. Preventive care is not just an optional add-on; it is a critical pillar of every robust care plan for diabetes mellitus 2, especially in high-risk populations.
9. How does the patient-provider relationship affect the care plan for diabetes mellitus 2?
The quality of the patient-provider relationship can make or break the success of a care plan for diabetes mellitus 2. Trust, empathy, and open communication encourage patients to share challenges, ask questions, and stay engaged in their treatment. Providers who use motivational interviewing techniques and shared decision-making create an atmosphere where patients feel heard and respected. This collaborative dynamic leads to more realistic goal setting and better adherence to treatment recommendations. Building rapport is particularly important in long-term chronic disease management, as it allows the care plan for type 2 diabetes to evolve organically with the patient’s changing needs.
10. What future innovations might reshape the care plan for type 2 diabetes?
The future of diabetes care is likely to be shaped by artificial intelligence (AI), digital twins, and regenerative medicine. AI can analyze massive datasets to predict individual responses to therapy, enabling even more refined personalization within a diabetes mellitus type 2 care plan. Digital twins—virtual models of a patient’s physiology—could allow clinicians to simulate treatment outcomes before implementing them in real life. Stem cell therapies and islet cell transplants are also being explored as potential cures, rather than just management strategies. These innovations have the potential to revolutionize what it means to have a care plan for diabetes mellitus 2, shifting the paradigm from lifelong management to targeted, potentially curative interventions.
Conclusion: The Future of Diabetes Care Hinges on Innovation, Personalization, and Equity
As the scientific understanding of type 2 diabetes deepens, so too must the strategies used to manage it. The evolution of the care plan for type 2 diabetes reflects a broader paradigm shift toward patient-centered, evidence-based, and technologically enabled care. No longer confined to a rigid checklist of medications and meal plans, today’s diabetes mellitus type 2 care plan is a living document—one that adapts to the patient’s biology, psychology, environment, and aspirations.
The integration of personalized nutrition, mental health support, advanced pharmacotherapy, and digital tools represents a profound step forward. These components do not operate in silos but synergistically, each reinforcing the others to create a holistic framework for disease management. Importantly, addressing disparities through inclusive care models ensures that these benefits are not limited to a privileged few but are accessible to all.
Looking ahead, the challenge is not just to implement these strategies but to do so with empathy, cultural competence, and scientific rigor. The care plan for diabetes mellitus 2 must continue to evolve alongside emerging evidence and shifting patient needs. In doing so, it holds the promise of not only managing disease but transforming lives—an aspiration that lies at the very heart of modern medicine.
Further Reading:
The Final Frontier in Diabetes Care: Implementing Research in Real-World Practice
Advances in the management of type 2 diabetes in adults
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.