Understanding the Role of the Pancreas in Type 2 Diabetes
The pancreas plays a critical role in blood sugar regulation through its production of insulin, a hormone that allows glucose to enter cells and be used for energy. In individuals with type 2 diabetes, this finely tuned system becomes disrupted, leading to either insulin resistance, where the body’s cells no longer respond properly to insulin, or impaired insulin secretion due to beta cell dysfunction. Over time, the pancreas struggles to keep up with the body’s increasing demands, eventually leading to chronically elevated blood glucose levels.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
The development of type 2 diabetes is multifactorial, involving genetics, lifestyle factors such as diet and exercise, and metabolic stressors that collectively strain pancreatic function. While historically considered a progressive and irreversible condition, new research has begun to challenge this assumption, raising the question: can your pancreas start working again with type 2 diabetes? Scientists and clinicians are exploring whether beta cells—the insulin-producing cells of the pancreas—can recover function or regenerate under the right conditions.
Reversibility of Beta Cell Dysfunction: What Science Is Discovering
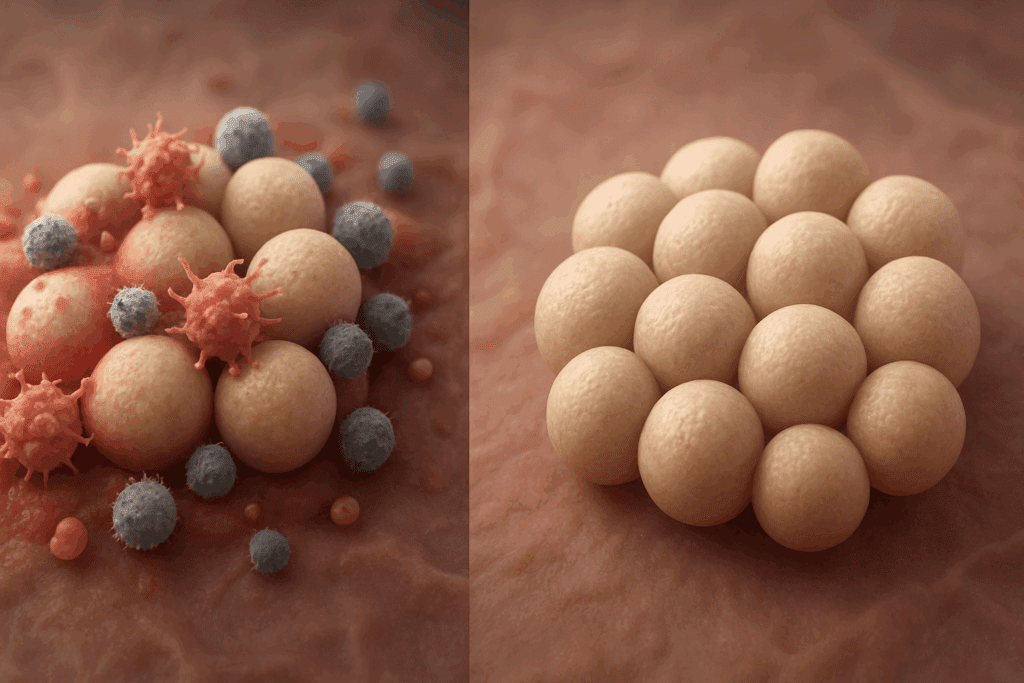
Recent studies have shown that beta cell dysfunction may not always be permanent. In fact, under certain circumstances, beta cells may regain some of their functional capacity. This groundbreaking insight has shifted the paradigm from managing diabetes symptoms to potentially reversing aspects of the disease. Animal studies and human clinical trials have provided promising evidence that beta cell rest, achieved through interventions like fasting, very low-calorie diets, or certain medications, can lead to partial restoration of insulin secretion.
One key concept in this area is “glucotoxicity,” which refers to the damaging effects of chronically high blood sugar levels on beta cell health. By improving glycemic control, whether through weight loss, dietary changes, or pharmacological interventions, the metabolic environment becomes more favorable for beta cell recovery. In this context, the idea that the pancreas can heal itself from diabetes is no longer purely speculative—it is grounded in a growing body of scientific evidence.
The Impact of Weight Loss and Caloric Restriction on Pancreatic Recovery
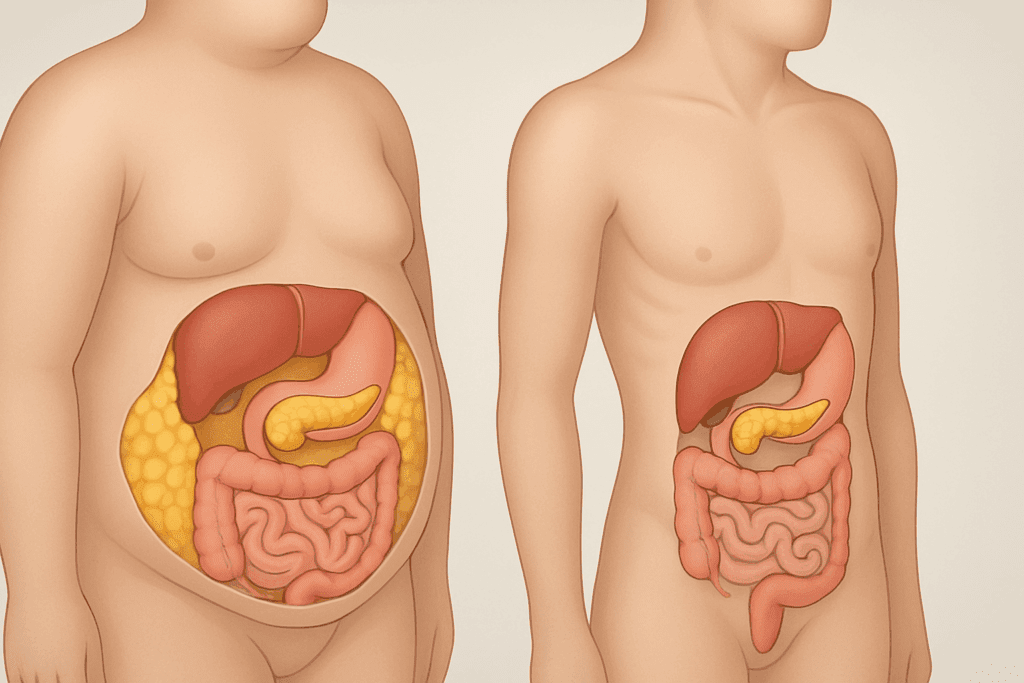
Perhaps one of the most compelling findings in recent years comes from studies examining the effects of weight loss on pancreatic function. Research from the United Kingdom’s DiRECT trial demonstrated that a significant proportion of individuals with type 2 diabetes who followed an intensive weight management program achieved remission. This remission was defined by the return of normal blood glucose levels without the need for diabetes medications.
The underlying mechanism appears to involve the reduction of fat in and around the pancreas, which may impair beta cell function when present in excess. By losing weight—especially visceral fat—participants were able to reduce the lipid burden on their pancreas, allowing beta cells to recover. This suggests that under the right metabolic conditions, the answer to the question “can your pancreas start working again with type 2 diabetes” is yes, particularly when weight loss is substantial and sustained.
Time-Restricted Eating and Intermittent Fasting: A Path to Pancreatic Regeneration?
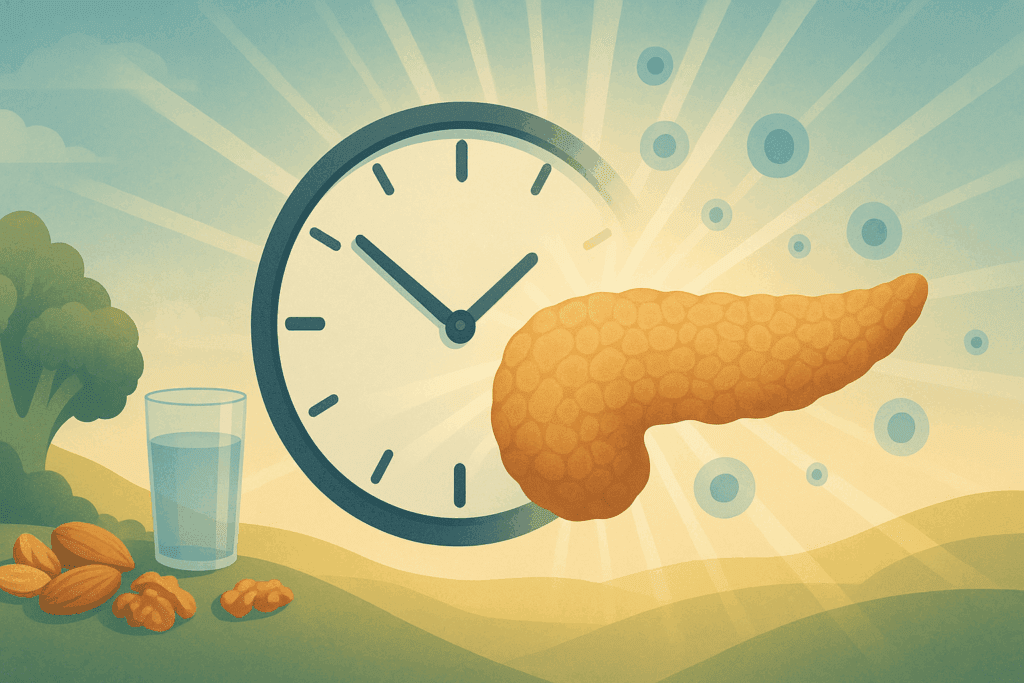
Intermittent fasting and time-restricted eating have gained popularity not only for weight management but also for their potential metabolic benefits. These dietary patterns, which alternate periods of eating and fasting, have been shown to improve insulin sensitivity, reduce blood glucose levels, and enhance cellular repair mechanisms. Emerging studies in both animals and humans suggest that intermittent fasting may also promote beta cell regeneration by providing periods of rest from insulin production.
During fasting states, the pancreas experiences reduced demand, which may help preserve or restore beta cell function. In rodent models, certain forms of fasting have led to the proliferation of insulin-producing cells. While more research is needed to confirm these effects in humans, early findings are encouraging and support the idea that the pancreas can heal itself from diabetes through metabolic interventions. These insights are particularly relevant for individuals seeking non-pharmacological strategies to manage or reverse their condition.
The Role of Incretin Hormones and Gut Health in Beta Cell Function
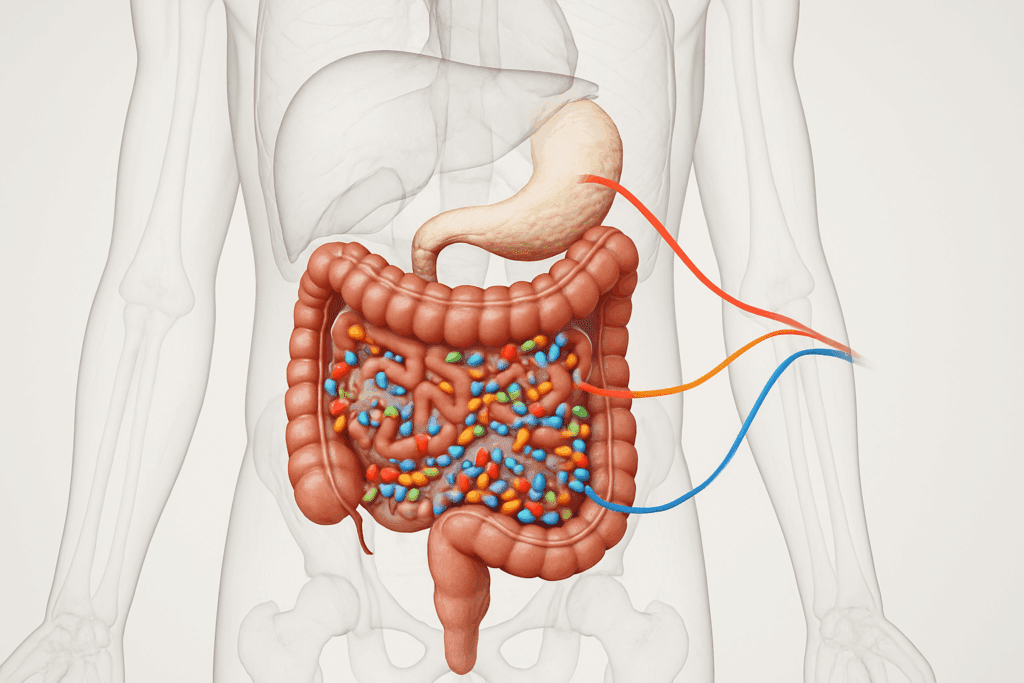
The interplay between the gut and pancreas is an area of active research, especially concerning incretin hormones such as GLP-1 (glucagon-like peptide-1). These hormones are released in response to food intake and stimulate insulin secretion. In people with type 2 diabetes, the incretin effect is often diminished. However, medications that mimic or enhance incretin hormones, such as GLP-1 receptor agonists, have been shown to improve beta cell responsiveness and lower blood glucose levels.
Beyond pharmacological approaches, gut health and the microbiome may also influence pancreatic function. Diets rich in fiber and fermented foods can promote a healthy gut microbiota, which in turn may support glucose metabolism and insulin sensitivity. Thus, optimizing gut health may indirectly contribute to beta cell preservation or recovery. This growing area of research strengthens the hypothesis that under favorable conditions, the pancreas can heal itself from diabetes to some extent.
The Potential of Stem Cell and Regenerative Therapies
In the realm of medical research discoveries, regenerative medicine offers some of the most exciting possibilities for treating type 2 diabetes. Scientists are exploring ways to reprogram cells or use stem cells to replace damaged or dysfunctional beta cells. In experimental settings, researchers have successfully converted non-insulin-producing cells into functioning beta-like cells capable of producing insulin. These breakthroughs hold promise for future therapies aimed at restoring endogenous insulin production.
Although these approaches are not yet widely available, clinical trials are ongoing, and progress is being made. If these therapies prove effective and safe, they could fundamentally change how we treat type 2 diabetes. In that context, asking whether your pancreas can start working again with type 2 diabetes becomes not only plausible but potentially answerable through medical innovation.
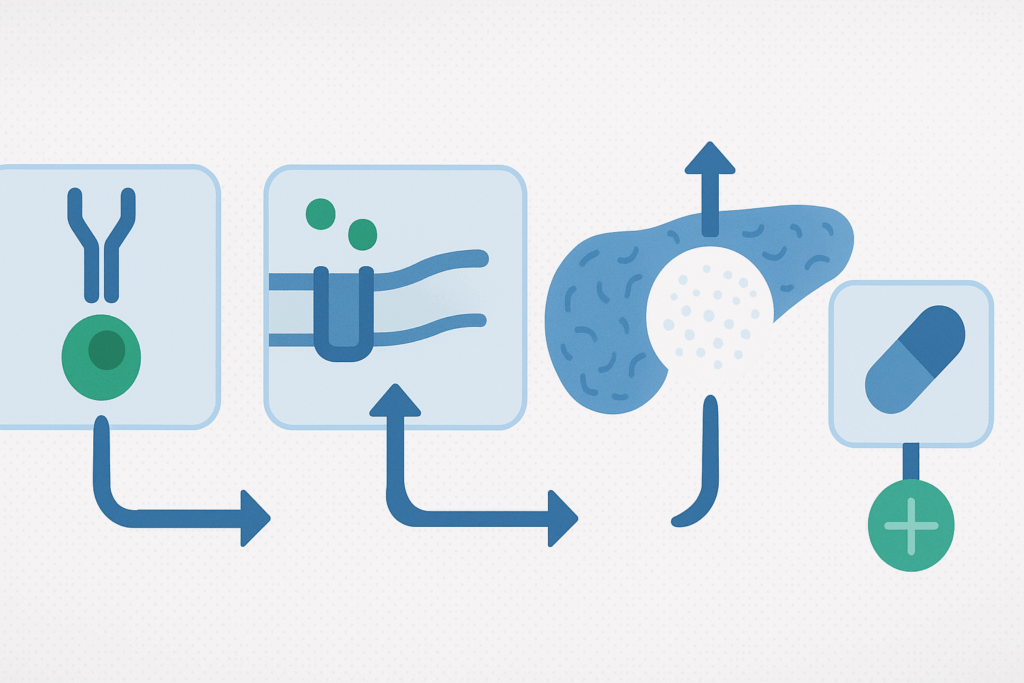
Medications That May Promote Beta Cell Function and Preservation
In addition to lifestyle interventions and regenerative medicine, certain medications have shown potential in preserving or enhancing beta cell function. GLP-1 receptor agonists and SGLT2 inhibitors are two classes of drugs that not only lower blood glucose but may also reduce beta cell stress. By improving the overall metabolic environment and decreasing insulin demand, these medications could help extend the functional lifespan of the pancreas.
Metformin, a cornerstone of type 2 diabetes treatment, primarily works by improving insulin sensitivity in the liver and peripheral tissues. While its direct effects on beta cells are less pronounced, it contributes to glycemic control, thereby reducing glucotoxic stress on the pancreas. Ongoing research into combination therapies and novel agents aims to further improve outcomes by targeting multiple pathways involved in diabetes progression.
Why Early Diagnosis and Intervention Matter
One of the most critical insights from recent research is the importance of early diagnosis and intervention. The longer type 2 diabetes goes untreated or poorly managed, the greater the likelihood of irreversible beta cell loss. Early and aggressive management not only helps prevent complications but may also preserve enough beta cell function to allow for meaningful recovery.
This has implications for public health messaging, clinical screening strategies, and patient education. Understanding that the pancreas may regain function if action is taken early could motivate individuals to seek care sooner and adhere more closely to lifestyle and medication recommendations. This reinforces the idea that the window of opportunity for pancreatic recovery exists and should not be missed.
Individual Variability and the Limits of Reversibility
While many individuals may benefit from interventions that support pancreatic recovery, it’s important to recognize that not everyone will respond in the same way. Factors such as age, duration of diabetes, genetic predisposition, and overall health all influence the extent to which the pancreas can heal itself from diabetes. Some people may achieve remission, while others may only experience partial improvement.
Medical professionals must tailor treatment strategies to individual needs and expectations. It’s equally important to maintain realistic goals and communicate that remission does not mean cure. Continuous monitoring, lifestyle commitment, and in many cases, ongoing medical therapy will remain necessary to sustain improvements in pancreatic function.
Looking Ahead: The Future of Diabetes Research and Pancreatic Regeneration
The field of diabetes research is advancing rapidly, with new insights emerging into how the disease develops, progresses, and—potentially—can be reversed. From cellular biology and genetics to nutrition science and behavioral medicine, an interdisciplinary approach is unlocking opportunities to improve the lives of millions affected by type 2 diabetes. Future research will likely focus on identifying biomarkers of beta cell stress and recovery, optimizing personalized treatment plans, and developing therapies that go beyond glucose control to address the root causes of pancreatic dysfunction.
In this evolving landscape, the question of whether your pancreas can start working again with type 2 diabetes continues to gain relevance. Scientific discoveries are offering hope where previously there was only management. Although there is no one-size-fits-all solution, the convergence of evidence suggests that meaningful recovery is possible for many.
Frequently Asked Questions: Can Your Pancreas Start Working Again with Type 2 Diabetes?
1. If my pancreas has been damaged by type 2 diabetes, is recovery still possible after many years?
Yes, but the likelihood and degree of recovery depend heavily on the duration and severity of type 2 diabetes. For individuals living with the condition for over a decade, beta cell loss can be significant, making full recovery less probable. However, research shows that even long-term diabetics may experience partial restoration of pancreatic function through intensive lifestyle changes and glycemic control. Whether your pancreas can start working again with type 2 diabetes later in its course often hinges on reducing chronic inflammation and improving insulin sensitivity. While full reversal may not be achievable for everyone, strategic interventions can slow progression and enhance remaining beta cell performance.
2. How does chronic stress impact pancreatic function in type 2 diabetes?
Chronic stress activates the hypothalamic-pituitary-adrenal (HPA) axis, increasing cortisol levels that worsen insulin resistance. Over time, this heightened stress response can further tax beta cells and impair glucose regulation. While often overlooked, stress management plays a crucial role in determining whether the pancreas can heal itself from diabetes. Techniques such as mindfulness meditation, deep breathing, and regular physical activity help reduce cortisol levels and create a metabolic environment more favorable to pancreatic health. Incorporating stress-reduction strategies alongside dietary and pharmacological interventions may enhance the potential for pancreatic recovery in people with type 2 diabetes.
3. Are there specific foods that help restore pancreatic function in type 2 diabetes?
Certain foods have been associated with improved pancreatic and metabolic health. Whole foods rich in polyphenols—such as berries, leafy greens, olive oil, and green tea—help reduce oxidative stress and support insulin signaling pathways. Omega-3 fatty acids, found in fatty fish and flaxseeds, also play a role in modulating inflammation, which is a key contributor to beta cell decline. While no food alone determines whether your pancreas can start working again with type 2 diabetes, dietary patterns emphasizing plant-based, anti-inflammatory ingredients can certainly support regenerative processes. Combining these foods with fasting-mimicking or low-calorie diets may further enhance pancreatic responsiveness.
4. Can personalized medicine improve the chances of pancreatic recovery in diabetes?
Yes, personalized medicine is rapidly advancing and holds promise for optimizing treatment outcomes. Genetic profiling and advanced metabolic testing can help identify individuals more likely to respond to specific interventions—such as GLP-1 therapy or intermittent fasting. Understanding your unique genetic and metabolic signature allows clinicians to tailor interventions that maximize the potential for beta cell regeneration. For some, the pancreas can heal itself from diabetes more readily when therapies are targeted, timely, and compatible with their biological makeup. This individualized approach represents the future of diabetes care, especially in the context of pancreatic recovery.
5. What role does sleep play in determining pancreatic recovery?
Quality sleep has a profound impact on hormonal balance, glucose metabolism, and beta cell function. Poor sleep disrupts circadian rhythms and increases insulin resistance, while adequate restorative sleep promotes hormonal harmony and reduces oxidative stress. If you’re asking whether your pancreas can start working again with type 2 diabetes, consider sleep as a foundational lifestyle factor. Recent studies suggest that individuals with consistent sleep patterns and good sleep hygiene exhibit better glycemic control and may even respond more effectively to diabetes interventions. Optimizing sleep may not regenerate beta cells directly but can significantly enhance the body’s overall ability to recover.
6. Is there a psychological component to healing the pancreas in type 2 diabetes?
Absolutely. The psychological burden of chronic illness can create a cycle of stress, poor adherence, and worsening metabolic health. Depression and anxiety are common among individuals with type 2 diabetes and can influence self-care behaviors critical to recovery. Studies have shown that mental health support, whether through therapy, support groups, or mindfulness training, can enhance treatment outcomes. If you’re wondering whether the pancreas can heal itself from diabetes, the mind-body connection should not be underestimated. Addressing emotional health is essential for sustaining the long-term lifestyle changes required for pancreatic improvement.
7. How do environmental toxins affect pancreatic health and diabetes progression?
Exposure to certain environmental toxins—such as persistent organic pollutants (POPs), heavy metals, and endocrine disruptors—has been linked to an increased risk of insulin resistance and beta cell dysfunction. These toxins can accumulate in fatty tissues and directly interfere with glucose metabolism and pancreatic signaling. While detoxification therapies are not proven to reverse diabetes, minimizing exposure to these toxins through organic foods, filtered water, and non-toxic household products may create a healthier internal environment. Creating such a setting could improve the odds that your pancreas can start working again with type 2 diabetes by reducing the external stressors that contribute to its decline.
8. Are there any cultural or socioeconomic factors that influence pancreatic recovery in type 2 diabetes?
Yes, access to quality healthcare, nutritional education, and financial resources significantly influences diabetes management and outcomes. Marginalized communities often face higher rates of food insecurity, limited healthcare access, and stress, all of which affect the possibility that the pancreas can heal itself from diabetes. Cultural dietary practices may either support or hinder metabolic health depending on how they align with diabetes-friendly principles. Public health interventions aimed at addressing these disparities are essential for enabling broader populations to benefit from pancreas-supportive strategies. Recognizing these systemic influences allows for more equitable and effective diabetes care.
9. How might future innovations in artificial intelligence support pancreatic recovery in diabetes care?
Artificial intelligence (AI) is poised to transform diabetes management by enabling real-time, personalized interventions. Machine learning models can analyze blood glucose trends, dietary intake, medication adherence, and lifestyle behaviors to predict optimal therapeutic strategies. As AI becomes more integrated into wearable technologies and mobile health apps, it can support early identification of beta cell stress and guide users toward interventions that maximize the chance for recovery. This technological support may improve the likelihood that your pancreas can start working again with type 2 diabetes by delivering precise, timely feedback based on individual data patterns. AI-guided health coaching is already being piloted in some care models with promising results.
10. Can the pancreas heal itself from diabetes completely, or is remission always temporary?
While remission is increasingly achievable, especially in early or moderate cases, it does not necessarily equate to a complete cure. The pancreas can heal itself from diabetes to a significant degree, particularly when interventions are introduced early and maintained long-term. However, beta cell resilience varies widely among individuals, and relapse is common if lifestyle habits revert or new metabolic stressors emerge. Continued monitoring and adaptive care plans are essential to sustaining remission. Ultimately, for many people, achieving pancreatic recovery means managing a chronic condition in a way that feels like freedom, even if vigilance must remain part of daily life.
Conclusion: Can the Pancreas Heal Itself from Diabetes? A Science-Based Perspective on Hope and Possibility
The notion that the pancreas can heal itself from diabetes was once considered overly optimistic, but today, it is increasingly supported by rigorous scientific inquiry. While a full cure for type 2 diabetes remains elusive, a combination of early intervention, sustained weight loss, intermittent fasting, gut health optimization, medication, and potentially even stem cell therapies all point toward the possibility of reversing beta cell dysfunction to some degree.
Understanding the biology behind pancreatic function, the mechanisms of damage and recovery, and the strategies that promote regeneration is crucial not only for clinicians and researchers but also for patients seeking empowered, evidence-based ways to manage their condition. As we look ahead, the expanding body of research offers a new lens through which to view type 2 diabetes—not merely as a chronic and unyielding disease but as a condition with modifiable outcomes and hope for partial recovery.
Ultimately, the answer to whether your pancreas can start working again with type 2 diabetes is: in many cases, yes—especially with early, targeted, and sustained intervention. While not everyone will experience complete remission, the potential for improved pancreatic function is a compelling reason to rethink how we approach this global health challenge.
Further Reading:
Beta cells in type 2 diabetes: Science explained
Remission of Type 2 diabetes restores pancreas function
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.


