Diabetes is a complex and pervasive health condition that affects millions of people worldwide. It is primarily divided into two major types—Type 1 and Type 2 diabetes—each with distinct causes, mechanisms, and treatment approaches. While the medical community has established clear distinctions between these two types, a lingering question often arises: Can Type 2 diabetes turn into Type 1 diabetes? This article delves into this inquiry, breaking down the scientific evidence and medical understanding surrounding this rare question.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
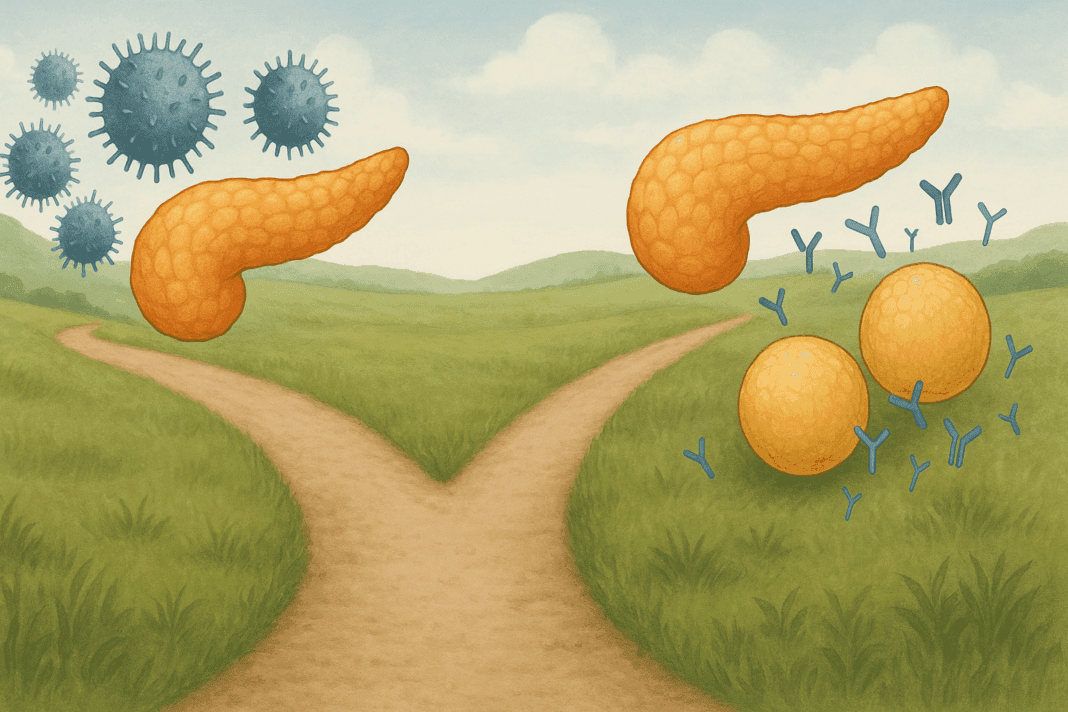
Understanding the Differences Between Type 1 and Type 2 Diabetes
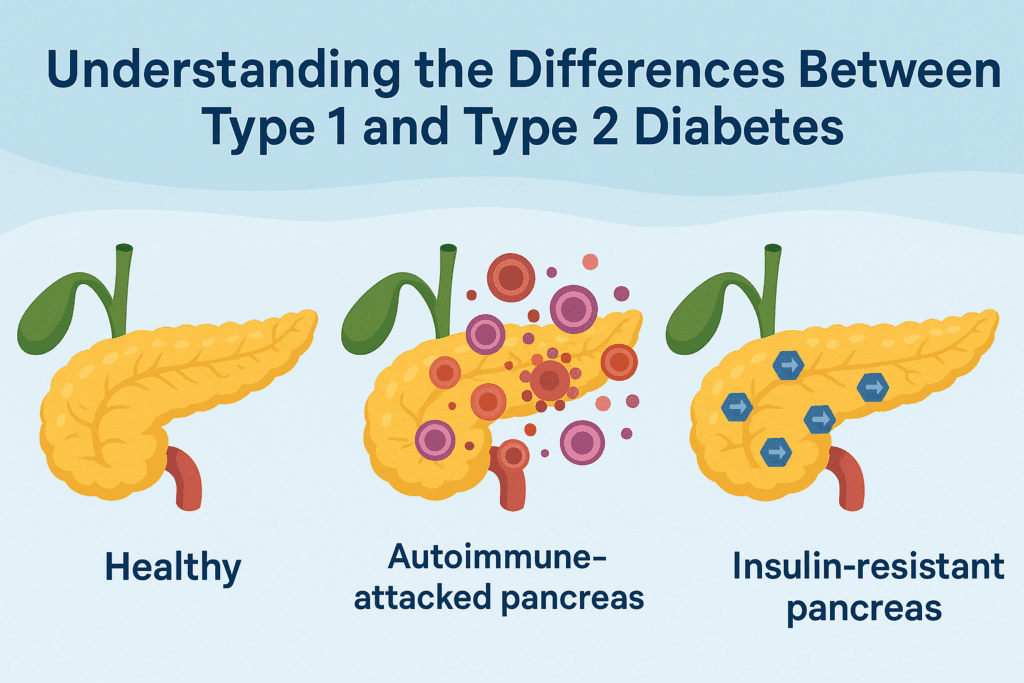
Before addressing whether Type 2 diabetes can evolve into Type 1, it is essential to comprehend the fundamental differences between the two. Type 1 diabetes is an autoimmune condition where the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This leads to an absolute deficiency of insulin, a hormone crucial for regulating blood glucose levels. Consequently, individuals with Type 1 diabetes must rely on insulin injections to manage their blood sugar.
In contrast, Type 2 diabetes is characterized by insulin resistance, where the body’s cells no longer respond properly to insulin. Over time, the pancreas compensates by producing more insulin, but eventually, it may not be able to meet the body’s demands. While Type 2 diabetes can often be managed with lifestyle changes, medications, and sometimes insulin, it does not inherently involve the autoimmune destruction of pancreatic beta cells.
These fundamental differences are crucial when exploring the potential for one type of diabetes to transform into the other.
Can Type 2 Diabetes Turn Into Type 1 Diabetes?
To directly address the question: Can Type 2 diabetes turn into Type 1? The short answer, according to current medical research, is no—Type 2 diabetes does not “turn into” Type 1 diabetes. However, understanding why this is the case requires a deeper dive into the mechanisms of both types of diabetes.
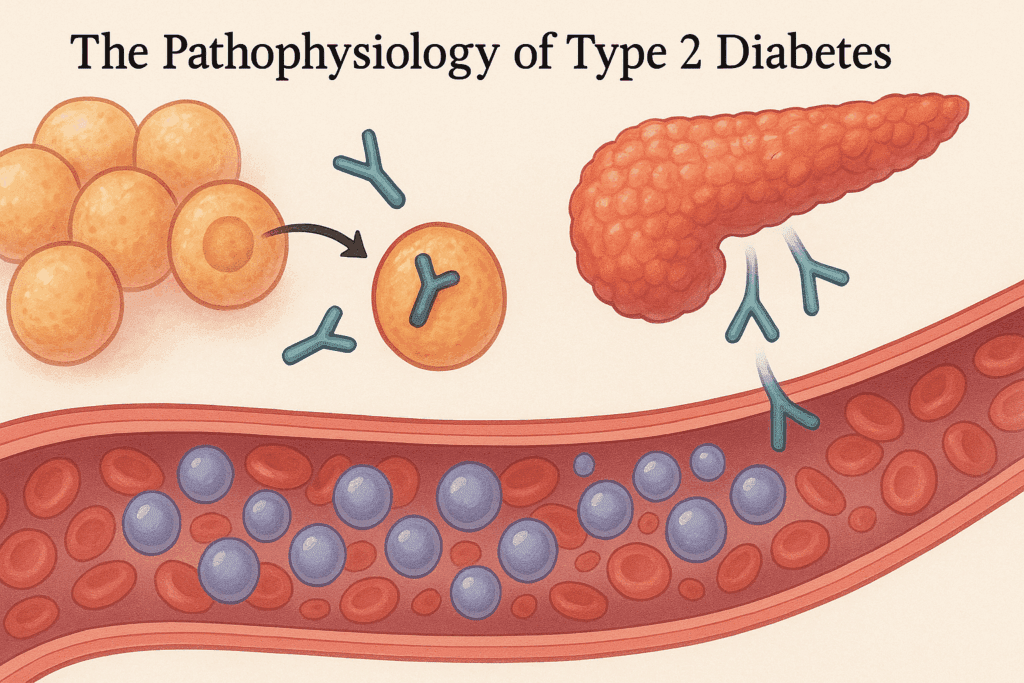
The Pathophysiology of Type 2 Diabetes
Type 2 diabetes is typically diagnosed when the body’s ability to respond to insulin decreases, a condition known as insulin resistance. Initially, the pancreas compensates by producing more insulin, which allows blood sugar levels to remain relatively stable. Over time, however, the pancreas may become unable to keep up with the increasing insulin demand, leading to higher blood glucose levels. This is when medication or insulin therapy might be introduced.
Although insulin resistance is the hallmark of Type 2 diabetes, it is crucial to note that the beta cells in the pancreas are not destroyed, unlike in Type 1 diabetes. Instead, they may become overworked and dysfunctional due to the body’s prolonged demand for insulin. In some cases, the beta cells can even recover with appropriate lifestyle interventions, such as weight loss, improved diet, and exercise.
The Nature of Type 1 Diabetes
In contrast, Type 1 diabetes is an autoimmune disorder in which the immune system attacks and destroys insulin-producing beta cells in the pancreas. This leads to an absolute insulin deficiency, which requires lifelong insulin therapy to manage blood glucose levels. Unlike Type 2 diabetes, Type 1 does not involve insulin resistance or a gradual decline in beta cell function; rather, it is characterized by the sudden and irreversible loss of beta cell function.
Because Type 1 diabetes is an autoimmune condition, it cannot be caused by lifestyle factors or insulin resistance. The destruction of beta cells in Type 1 is an irreversible process, which means it is not possible for Type 2 diabetes to evolve into Type 1. The mechanisms that lead to Type 1 diabetes are fundamentally different from those that lead to Type 2 diabetes, making such a transition biologically implausible.
Why the Confusion? Exploring Common Misunderstandings
Despite the clear distinctions between Type 1 and Type 2 diabetes, the idea that Type 2 diabetes could turn into Type 1 still circulates in some circles. This misconception may arise due to several factors, including the following:
Progression of Insulin Deficiency in Type 2 Diabetes: In advanced stages of Type 2 diabetes, when the pancreas can no longer produce sufficient insulin, individuals may require insulin therapy to control their blood sugar levels. This can sometimes create confusion, as it may appear that the person with Type 2 diabetes is shifting to a condition that is similar to Type 1 diabetes, which also requires insulin.
Increased Risk of Autoimmune Conditions in Type 2 Diabetes: Some studies suggest that individuals with Type 2 diabetes may have a higher risk of developing autoimmune conditions, including those that affect the pancreas. In rare cases, this might lead to the development of autoimmune pancreatitis, which could result in further beta cell destruction. While this may make it seem like Type 2 diabetes is “turning into” Type 1, it is more likely a complication rather than a transformation of the disease.
Misunderstanding of Diabetes Progression: Many people with Type 2 diabetes experience worsening blood sugar control over time. In some cases, the condition progresses despite lifestyle changes or medications, leading to insulin dependency. However, this progression is still within the context of Type 2 diabetes and does not involve the autoimmune destruction of beta cells seen in Type 1.
Is There Any Overlap Between Type 1 and Type 2 Diabetes?
While Type 2 diabetes cannot become Type 1, there are instances where the two types of diabetes may appear to overlap. One such example is Latent Autoimmune Diabetes in Adults (LADA), sometimes referred to as Type 1.5 diabetes. LADA is a form of diabetes that shares characteristics with both Type 1 and Type 2 diabetes. Like Type 1, LADA involves autoimmune destruction of beta cells, but it progresses much more slowly and is initially diagnosed as Type 2 diabetes.
Because individuals with LADA do not typically require insulin at the time of diagnosis and may initially respond to oral medications, the condition is often mistaken for Type 2 diabetes. Over time, however, as beta cells are destroyed, insulin therapy becomes necessary, which may lead to confusion regarding the progression of the disease.
Does Type 2 Diabetes Ever Become Type 1?
To reiterate, does Type 2 diabetes become Type 1? The answer is no. However, it is possible for individuals with Type 2 diabetes to develop autoimmune-related issues that lead to beta cell destruction, but these are rare cases and do not reflect a transition from Type 2 to Type 1 diabetes. It is also important to note that the progression of Type 2 diabetes to a point where insulin therapy is required does not equate to the development of Type 1 diabetes.
Recent Research and Emerging Insights on Type 1 and Type 2 Diabetes
The distinction between Type 1 and Type 2 diabetes remains critical for understanding their respective treatments and management strategies. Recent research into Type 2 diabetes has focused on improving the understanding of insulin resistance and the potential for reversing the condition through lifestyle modifications, medications, or bariatric surgery. Studies are also exploring the possibility of early interventions that could help preserve beta cell function for as long as possible.
In the case of Type 1 diabetes, groundbreaking research is being conducted to explore potential cures, including beta cell transplants, gene therapy, and immunotherapy. However, as of now, there is no established way to reverse Type 1 diabetes, and lifelong insulin therapy remains the standard approach.
Frequently Asked Questions (FAQ) on Type 2 and Type 1 Diabetes
Can Type 2 diabetes eventually require insulin treatment like Type 1 diabetes?
Yes, as Type 2 diabetes progresses, insulin therapy may be required if the pancreas is unable to produce sufficient insulin to manage blood sugar levels. However, this does not mean Type 2 turns into Type 1. The necessity for insulin in Type 2 is due to insulin resistance and beta cell dysfunction, while Type 1 requires insulin because the pancreas no longer produces any insulin at all due to the autoimmune destruction of beta cells.
Is there any chance that Type 2 diabetes will transform into an autoimmune condition similar to Type 1?
While Type 2 diabetes is not typically considered an autoimmune disease, there are rare cases, such as Latent Autoimmune Diabetes in Adults (LADA), where the condition can develop autoimmune features. LADA may initially appear as Type 2 diabetes due to insulin resistance, but it gradually develops into an autoimmune process that attacks the pancreas, similar to Type 1 diabetes. Thus, while Type 2 does not turn into Type 1, certain rare conditions may cause overlap between the two.
Can Type 2 diabetes eventually cause the body to lose its ability to produce insulin?
Over time, as Type 2 diabetes progresses, the pancreas can become less effective at producing insulin, especially when insulin resistance worsens. This can result in the need for insulin therapy to manage blood sugar levels. However, this is still a manifestation of Type 2 diabetes and does not signal a shift toward Type 1 diabetes, which is characterized by the total destruction of insulin-producing cells in the pancreas.
What are the key factors that lead to the need for insulin in Type 2 diabetes?
In Type 2 diabetes, the body’s cells become resistant to insulin, which makes it harder for glucose to enter the cells, raising blood sugar levels. Initially, the pancreas compensates by producing more insulin. Over time, however, the pancreas struggles to meet the body’s insulin demands, leading to a decline in insulin production. As a result, insulin injections may be necessary, but this is part of the natural progression of Type 2, not a transformation into Type 1 diabetes.
Can Type 2 diabetes mimic Type 1 diabetes as it worsens?
Although Type 2 and Type 1 diabetes share some symptoms, such as high blood sugar, they are fundamentally different conditions. Type 2 diabetes progresses due to insulin resistance and beta cell dysfunction, whereas Type 1 is an autoimmune condition that destroys insulin-producing cells. While the need for insulin in Type 2 may seem similar to Type 1, it is not indicative of Type 2 becoming Type 1. The two conditions have different underlying causes, and Type 2 does not develop into Type 1.
Are there any conditions that cause Type 2 diabetes to behave like Type 1?
In some cases, individuals with Type 2 diabetes may experience an autoimmune component, such as in LADA, where insulin resistance transitions into an autoimmune attack on the pancreas. This process can lead to a loss of insulin production, which might make it appear that Type 2 has turned into Type 1. However, LADA is a distinct form of diabetes that shares characteristics of both Type 1 and Type 2, and while it may resemble Type 1, it is not a progression of Type 2.
Can a Type 2 diabetic develop the same complications as someone with Type 1 diabetes?
While the causes of Type 1 and Type 2 diabetes are different, both can lead to similar complications if blood sugar is not well controlled. These complications can include nerve damage, kidney problems, and cardiovascular issues. However, these complications arise in Type 2 diabetes due to prolonged insulin resistance and inadequate insulin production, not because of the autoimmune destruction of pancreatic cells, as in Type 1 diabetes.
How do insulin resistance and beta cell dysfunction impact the development of Type 2 diabetes?
In Type 2 diabetes, the body’s cells become resistant to insulin, meaning they don’t absorb glucose effectively. Over time, the pancreas compensates by producing more insulin, but as the condition progresses, the pancreas becomes less able to produce enough insulin. Eventually, this leads to elevated blood sugar levels and the need for external insulin, though this process is distinct from the complete loss of insulin production in Type 1 diabetes.
What factors could cause a Type 2 diabetic to require insulin therapy?
Several factors can lead a person with Type 2 diabetes to require insulin, including the progression of insulin resistance, the pancreas’ declining ability to produce insulin, and the need for better blood sugar control. While the progression of Type 2 can lead to the use of insulin, this does not mean Type 2 turns into Type 1. The need for insulin is a step in managing the condition as it worsens but does not indicate the onset of Type 1 diabetes, which results from an autoimmune attack on insulin-producing cells.
Can a Type 2 diabetic experience the same loss of insulin production as someone with Type 1?
A Type 2 diabetic may experience reduced insulin production as the condition progresses, but this is not the same as the complete loss of insulin production seen in Type 1 diabetes. Type 2 diabetes involves insulin resistance and progressive pancreatic dysfunction, while Type 1 is characterized by the destruction of beta cells by the immune system. Even if insulin therapy becomes necessary in Type 2, it is still part of the natural progression of the disease and does not indicate a transformation into Type 1.
Conclusion: Clarifying the Distinction Between Type 1 and Type 2 Diabetes
In conclusion, while the question “Can Type 2 diabetes turn into Type 1?” is an understandable one given the complexities of the disease and its management, the current scientific consensus is that Type 2 diabetes cannot become Type 1. The two conditions arise from different underlying causes—insulin resistance and autoimmune beta cell destruction—and have distinct clinical features and treatment strategies. Although there are instances where individuals with Type 2 diabetes may require insulin therapy, this does not indicate a transformation into Type 1 diabetes.
Ultimately, it is important to be aware of the distinctions between the two types of diabetes, especially when considering the most appropriate treatment and management options. Advances in diabetes research continue to shed light on both conditions, offering hope for better treatment options and, eventually, potential cures. As always, individuals with diabetes should work closely with healthcare providers to monitor and manage their condition effectively.
By maintaining an informed approach to diabetes care and understanding the key differences between Type 1 and Type 2, patients and healthcare professionals can work together to optimize health outcomes.
Further Reading:
Is It Possible for Type 2 Diabetes to Turn into Type 1?
Can Type 2 Diabetes Turn Into Type 1?
Subtypes of Type 2 Diabetes Determined From Clinical Parameters
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.