Understanding the Critical Role of Blood Glucose Monitoring in Type 2 Diabetes
Managing type 2 diabetes requires more than just taking medication. It demands a comprehensive strategy involving diet, physical activity, stress management, and—crucially—consistent blood glucose monitoring. As researchers continue to investigate the most effective methods for controlling blood sugar levels, new evidence highlights the importance of timing and frequency in glucose checks, especially for individuals using medications like metformin. While metformin remains the first-line pharmacological treatment for type 2 diabetes, its effectiveness can be significantly enhanced when paired with proper blood sugar tracking. This ongoing research has emphasized that personalized monitoring strategies not only improve glycemic control but also empower patients to make real-time lifestyle adjustments that may improve long-term outcomes.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
For many living with type 2 diabetes, the process of checking blood sugar may seem routine. However, recent findings suggest that the best time to check blood sugar for type 2 diabetes with metformin isn’t the same for everyone. Factors such as meal timing, physical activity, sleep patterns, and even medication timing can all influence glucose readings and, by extension, treatment efficacy. In this new era of precision medicine, understanding when and how often to check blood glucose for type 2 diabetes is evolving into a highly individualized science. These updates in clinical guidance are grounded in patient-centered research, supporting a more responsive, real-time approach to managing diabetes that aligns with a person’s unique metabolic rhythms.
The Science Behind Metformin and Its Interaction with Glucose Levels
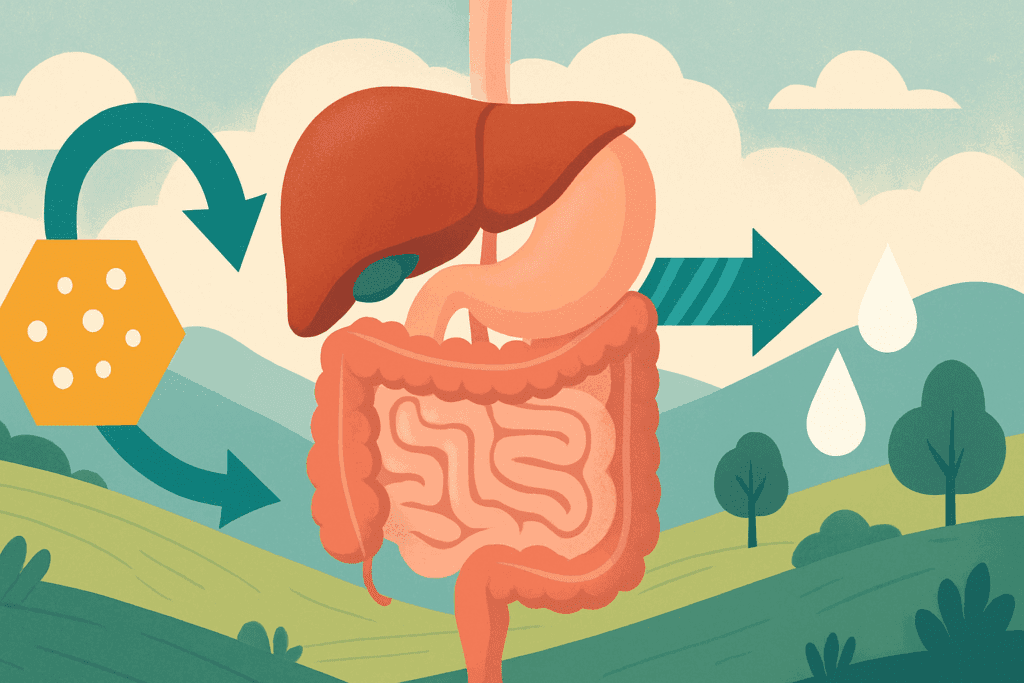
Metformin, widely recognized as the cornerstone of pharmacological treatment for type 2 diabetes, works by improving insulin sensitivity and reducing hepatic glucose production. Its benefits are well-documented, with decades of clinical trials affirming its ability to lower A1C levels and mitigate the risk of long-term complications like cardiovascular disease and neuropathy. However, what’s often underappreciated is how metformin’s effectiveness can vary depending on how and when patients monitor their blood sugar.
Emerging studies have demonstrated that individuals who optimize their glucose monitoring strategies see better alignment with metformin’s peak action times. The best time to check blood sugar for type 2 diabetes with metformin, for example, may be during early morning fasting hours or post-prandial windows—depending on the specific patient’s insulin response and lifestyle. Monitoring in these windows can offer a clearer picture of how well metformin is working to control post-meal glucose spikes or fasting hyperglycemia. Without this strategic approach, patients may miss important glucose fluctuations, potentially leading to under- or overtreatment.
Moreover, metformin’s delayed peak action (typically occurring 4 to 6 hours after ingestion) makes it critical for patients and clinicians to time glucose checks accordingly. By syncing blood glucose monitoring with metformin’s pharmacokinetics, patients can gain a more accurate understanding of whether their current regimen is achieving therapeutic goals. This personalized feedback loop enables timely medication adjustments and dietary modifications, improving overall diabetes management and quality of life.
When Is the Best Time to Check Blood Sugar for Type 2 Diabetes with Metformin?
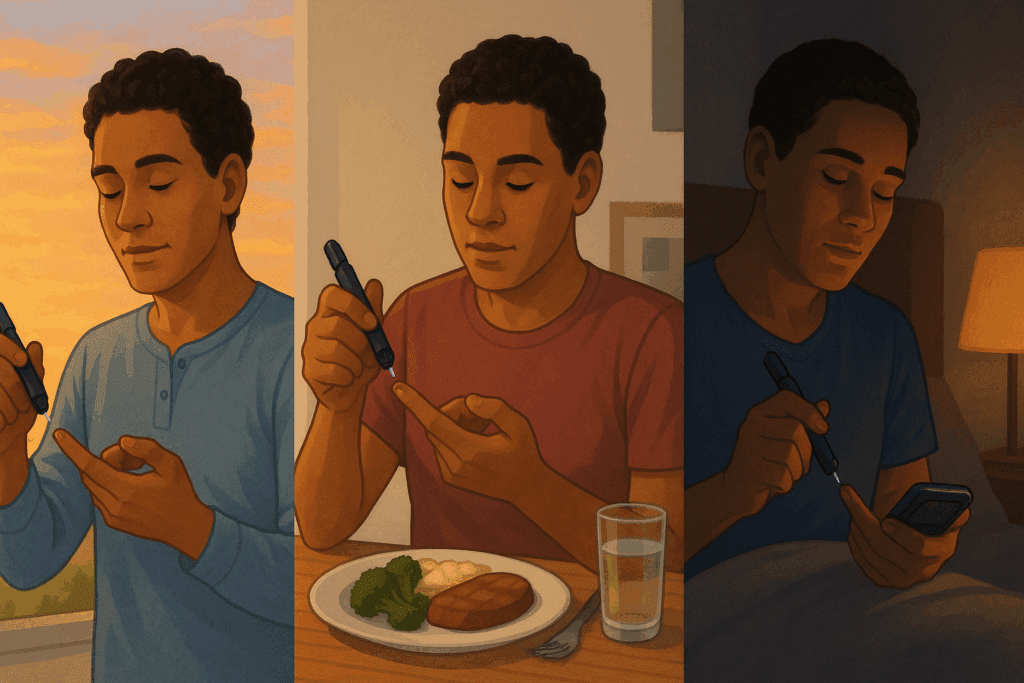
Although traditional guidelines recommend checking fasting blood glucose in the morning, the emerging consensus is that a more dynamic approach yields better outcomes—especially for those on metformin. Research indicates that the best time to check blood sugar for type 2 diabetes with metformin can depend heavily on the individual’s eating schedule, sleep patterns, and response to medication.
For some, checking glucose levels two hours after a meal may reveal whether their body is effectively handling postprandial glucose surges. For others, a pre-dinner or bedtime reading may be more telling, especially if nocturnal hypoglycemia or dawn phenomenon is a concern. By understanding their personal glucose trends, patients can better assess the impact of metformin across different metabolic states. This nuanced approach helps avoid misleading snapshots that could mask underlying dysregulation.
Clinicians increasingly recommend a combination of fasting and post-meal glucose checks to provide a fuller metabolic profile. This integrated strategy aligns with the pharmacodynamics of metformin, particularly its tendency to blunt hepatic glucose production overnight. When patients understand when to test and how those results relate to their medication, they are better equipped to make informed decisions about dietary adjustments, exercise timing, and medication scheduling. Ultimately, identifying the best time to check blood sugar for type 2 diabetes with metformin can personalize care, reduce glucose variability, and enhance treatment outcomes.
How Often to Check Blood Glucose for Type 2 Diabetes: Individualizing Frequency
Determining how often to check blood glucose for type 2 diabetes is just as important as knowing when to check. Frequency guidelines have traditionally varied based on treatment modality—daily for those on insulin, and less frequently for those on oral agents like metformin. However, recent studies challenge this one-size-fits-all model, suggesting that even non-insulin users can benefit from regular monitoring, especially during periods of lifestyle change, illness, or stress.
New recommendations support a more flexible, situation-based approach. For example, patients adjusting to a new diet or exercise program may find it helpful to check glucose before and after meals to understand how different foods or physical activity levels impact their blood sugar. Similarly, individuals with fluctuating glucose levels may benefit from checking multiple times per day until stability is achieved. The frequency should be dictated by the patient’s goals, whether it’s reducing A1C, minimizing hypoglycemic episodes, or tracking progress during weight loss.
Importantly, technology has transformed the landscape of type 2 diabetes monitoring. Continuous glucose monitors (CGMs) and flash glucose systems now provide real-time data, allowing for less invasive but more comprehensive tracking. These tools can reduce the burden of frequent fingersticks while offering detailed trend analysis. For those using metformin, CGMs can illuminate how glucose responds to medication over 24-hour cycles, providing insights that were previously unavailable. Understanding how often to check blood glucose for type 2 diabetes is now about balancing patient comfort with clinical utility—a balance made easier with modern monitoring technologies.
The Role of Personalized Monitoring in Enhancing Metformin’s Efficacy
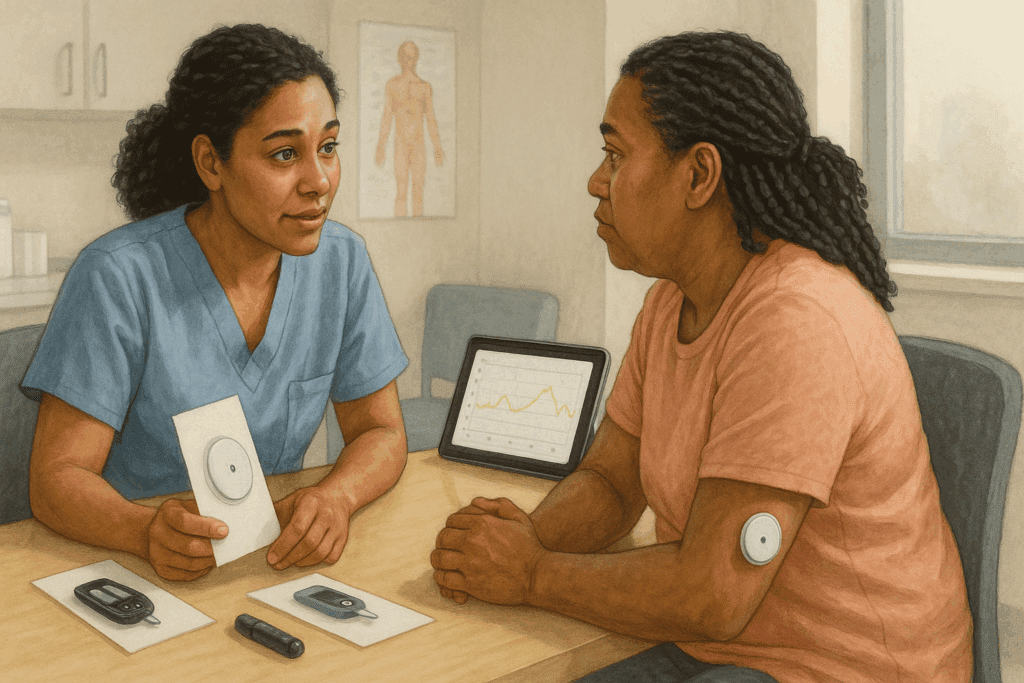
Personalized medicine is reshaping how we manage chronic conditions, and diabetes care is no exception. By tailoring monitoring routines to individual metabolic patterns, patients can derive greater benefit from medications like metformin. This approach recognizes that two individuals with the same A1C may experience vastly different daily fluctuations in glucose—and thus may require different monitoring strategies.
For example, a patient who experiences significant post-meal spikes despite a relatively controlled fasting glucose may need to focus more on postprandial monitoring. In contrast, someone with high morning readings might benefit from overnight tracking to assess dawn phenomenon or nocturnal insulin resistance. By using these individualized insights, metformin therapy can be fine-tuned to address specific glycemic challenges, such as inadequate suppression of hepatic glucose output or suboptimal peripheral insulin sensitivity.
Moreover, research shows that patients who engage in regular, personalized glucose monitoring are more likely to adhere to their medication regimens. This may be due in part to the immediate feedback loop created by testing: seeing the impact of lifestyle choices and medication in real-time reinforces positive behaviors and promotes a sense of agency. When patients know the best time to check blood sugar for type 2 diabetes with metformin and understand how often to do so, they are more likely to stay engaged with their care plan, leading to better long-term outcomes.
Insights from Recent Clinical Trials and Observational Studies
Over the past five years, a number of clinical trials and observational studies have provided new insights into optimal blood glucose monitoring practices. One such study, published in Diabetes Care, evaluated over 3,000 patients using metformin alone. It found that those who checked their blood sugar at both fasting and post-meal intervals had significantly lower A1C levels than those who tested only once daily or inconsistently. This suggests that comprehensive monitoring can enhance metformin’s glucose-lowering effects by providing a fuller picture of glycemic control.
Another study conducted by researchers at the Joslin Diabetes Center investigated how continuous glucose monitoring influenced treatment outcomes in non-insulin users. Participants using CGMs experienced fewer hyperglycemic episodes and demonstrated improved time-in-range metrics, even without insulin therapy. These findings underscore the value of frequent, real-time data—even for patients who are not traditionally advised to test often. The research concluded that the synergy between technology, education, and tailored monitoring significantly boosts metformin efficacy.
Additionally, observational data from population health studies show that demographic and lifestyle factors—including age, diet, and sleep—can influence the optimal timing and frequency of glucose monitoring. For instance, older adults may benefit from more structured testing routines, while younger, tech-savvy individuals may prefer flexible, tech-enabled approaches. These insights highlight the importance of adaptability in crafting type 2 diabetes monitoring plans that reflect real-world needs and constraints.
How Technology Is Revolutionizing Type 2 Diabetes Monitoring
The integration of digital health tools into diabetes care is accelerating rapidly. From wearable CGMs to smartphone apps that sync glucose data with meal logs and physical activity, technology now offers unprecedented visibility into daily blood sugar patterns. For individuals taking metformin, this visibility is invaluable, helping to pinpoint the best time to check blood sugar for type 2 diabetes based on personalized data rather than generalized guidelines.
Modern CGMs such as the Dexcom G7 and Abbott’s FreeStyle Libre systems can provide minute-by-minute readings, highlighting subtle glucose changes that might be missed with standard fingerstick methods. These devices not only improve accuracy but also reduce the psychological burden of diabetes management by eliminating the need for constant manual testing. For patients on metformin, this means being able to observe how their glucose responds throughout the day—before meals, after meals, during exercise, and overnight—creating a more holistic understanding of their condition.
In addition to CGMs, artificial intelligence (AI) and machine learning algorithms are beginning to play a role in personalized diabetes care. Some platforms now use patient data to generate tailored recommendations for when and how often to check blood glucose for type 2 diabetes, based on past patterns, medication timing, and lifestyle inputs. As these tools continue to evolve, they will likely become central to helping patients and providers co-create evidence-based, patient-specific monitoring plans.
Navigating Practical Challenges and Overcoming Barriers to Monitoring
Despite the clear benefits of tailored blood glucose monitoring, practical barriers remain. For some patients, cost is a major concern—especially when insurance coverage for CGMs or test strips is limited. Others may struggle with the discomfort or inconvenience of frequent testing, particularly if they have comorbid conditions like neuropathy or arthritis that make fingersticks painful.
Education and support are key to overcoming these challenges. Diabetes educators, primary care physicians, and endocrinologists all play a role in helping patients find monitoring routines that are both clinically effective and personally sustainable. For example, alternating between CGM use and periodic fingerstick testing may offer a compromise for those concerned about affordability. Similarly, setting clear goals—such as identifying the best time to check blood sugar for type 2 diabetes with metformin—can help patients stay motivated by tying monitoring to meaningful outcomes.
Additionally, addressing cultural and psychological factors is essential. Some individuals may feel overwhelmed by constant data or may avoid testing out of fear of judgment. Creating a supportive, non-punitive care environment that emphasizes learning over blame can encourage consistent monitoring. The goal is not perfection but progress—using glucose data as a tool for empowerment rather than criticism.
Frequently Asked Questions: Type 2 Diabetes Monitoring and Metformin
1. Can stress or sleep patterns influence the best time to check blood sugar for type 2 diabetes with metformin?
Absolutely. Stress and sleep cycles significantly affect blood glucose levels and, consequently, influence the best time to check blood sugar for type 2 diabetes with metformin. Elevated cortisol during periods of stress can spike blood sugar levels even in the absence of food intake, especially in the early morning hours. This means some individuals may need to monitor glucose shortly after waking or during high-stress periods, regardless of their meal schedule. Inadequate sleep, especially fragmented or shortened sleep, can also cause insulin resistance, which may make blood sugar monitoring more important during morning hours or after particularly poor nights of rest. Factoring in sleep quality and emotional stress provides a more nuanced view of glucose control, helping to fine-tune metformin use more effectively.
2. What role does dietary timing play in determining how often to check blood glucose for type 2 diabetes?
Meal timing can be a crucial factor in optimizing how often to check blood glucose for type 2 diabetes. For example, people who follow intermittent fasting or eat large meals late in the day may benefit from more frequent post-meal checks to evaluate how their body processes prolonged fasting periods followed by high-glycemic intake. Others who consume smaller, evenly spaced meals may require fewer glucose checks, as their blood sugar is less likely to swing dramatically. The type and timing of carbohydrate consumption also influence this equation—meals rich in fast-absorbing sugars may call for closer monitoring. Integrating meal timing into type 2 diabetes monitoring helps patients respond more dynamically to dietary effects and medication timing.
3. How can seasonal changes affect the effectiveness of type 2 diabetes monitoring?
Surprisingly, seasonal shifts can alter metabolic patterns, influencing both how often to check blood glucose for type 2 diabetes and when those checks are most useful. Colder months may be associated with decreased physical activity, leading to elevated fasting glucose levels. Conversely, increased sun exposure and higher activity in summer can enhance insulin sensitivity, potentially reducing glucose variability. These seasonal shifts may require temporary changes to type 2 diabetes monitoring routines, especially for patients using metformin. Adjusting monitoring frequency during high-stress or sedentary seasons ensures that data remains clinically relevant and treatment remains effective throughout the year.
4. Is there an ideal window during exercise to measure the impact of metformin on blood sugar?
Yes, strategic timing around exercise can provide valuable insights for patients trying to optimize the best time to check blood sugar for type 2 diabetes with metformin. Exercise typically reduces blood sugar, but the degree varies depending on when glucose is measured. Measuring glucose 30 minutes before and about an hour after moderate to intense activity can reveal how metformin and physical exertion interact. These readings may help determine whether glucose dips too low after exertion or if there’s a post-exercise spike, which sometimes occurs with anaerobic activity. Understanding these fluctuations can inform whether exercise should be timed around metformin dosing or meal intake for better glycemic balance.
5. How can digital tools improve how often to check blood glucose for type 2 diabetes?
Digital tools, especially continuous glucose monitors (CGMs) and smartphone-integrated apps, are transforming how often to check blood glucose for type 2 diabetes in a practical, patient-friendly way. These technologies eliminate the need for manual tracking and allow users to visualize trends over time, such as recurring post-breakfast spikes or late-night elevations. CGMs can alert patients to fluctuations even when they’re unaware, which is especially valuable for those who may otherwise avoid frequent testing. Moreover, some platforms are equipped with AI-driven insights that suggest personalized testing frequencies based on behavioral patterns, diet, and metformin use. This automated intelligence helps tailor type 2 diabetes monitoring without overwhelming patients with data.
6. Should patients using both metformin and insulin adjust their monitoring differently?
Definitely. Patients on combination therapy—including metformin and insulin—often require a more nuanced approach to monitoring. While insulin typically necessitates more frequent glucose checks, metformin modifies insulin sensitivity and hepatic glucose output, which can affect the timing and interpretation of those readings. In these cases, the best time to check blood sugar for type 2 diabetes with metformin may shift depending on insulin action peaks. For example, a post-lunch reading might capture insulin’s mid-course effectiveness while also showing whether metformin is successfully suppressing hepatic glucose production. This dual-tracking strategy ensures neither medication’s effects are misinterpreted in isolation.
7. What are some overlooked signs that your current type 2 diabetes monitoring strategy may need revision?
Several subtle indicators can signal that your type 2 diabetes monitoring routine isn’t fully aligned with your needs. Persistent fatigue after meals, nighttime awakenings, or unexpected hunger episodes may suggest unmonitored glucose spikes or dips. If A1C levels are stable but daily symptoms persist, it could mean your testing schedule is missing critical moments, such as early morning or post-meal fluctuations. Reassessing the best time to check blood sugar for type 2 diabetes with metformin—especially if lifestyle factors like work hours or diet have changed—can restore alignment between data and reality. Infrequent or poorly timed readings may offer a false sense of control, leading to therapeutic stagnation.
8. Are there social or psychological factors that impact how often people monitor blood glucose with type 2 diabetes?
Yes, psychosocial factors play a profound but often underestimated role in how often people engage with type 2 diabetes monitoring. Emotional burnout, fear of poor results, or stigma around public testing can all decrease adherence. Some patients may avoid checking their blood sugar after eating indulgent meals due to guilt, which skews overall data accuracy. Social support, whether through peer groups or digital communities, can increase consistency and foster healthier monitoring habits. Addressing these psychological barriers is key to helping patients identify the best time to check blood sugar for type 2 diabetes with metformin and maintain a realistic, sustainable testing frequency.
9. Can fluctuations in kidney or liver function change the best time to check blood sugar for type 2 diabetes with metformin?
Yes, kidney and liver function are critical determinants in how metformin is metabolized and cleared from the body, which in turn affects optimal monitoring timing. Impaired renal function can prolong metformin’s action, potentially blunting postprandial spikes or causing unexpected lows. Similarly, liver dysfunction may affect glucose production, altering fasting glucose levels and the expected pharmacodynamics of metformin. In such cases, working with a healthcare provider to determine a revised schedule for type 2 diabetes monitoring is essential. These physiological shifts often require not just altered medication dosing, but new strategies for how often to check blood glucose for type 2 diabetes to ensure safety and efficacy.
10. What advancements in research could change future recommendations for type 2 diabetes monitoring?
Emerging studies in precision endocrinology and wearable biosensors suggest that future recommendations for type 2 diabetes monitoring may become entirely algorithm-driven. Research is moving toward personalized “monitoring passports” that adjust in real-time based on circadian rhythm, diet composition, microbiome profiles, and even stress biomarkers. These tools could redefine the best time to check blood sugar for type 2 diabetes with metformin on a day-to-day basis. Moreover, future apps may proactively suggest how often to check blood glucose for type 2, based not only on past behavior but also predictive modeling of upcoming lifestyle events. This represents a paradigm shift from reactive to predictive diabetes management, promising unprecedented personalization in type 2 diabetes care.
Conclusion: Empowering Patients Through Smart, Personalized Monitoring
The landscape of type 2 diabetes management is shifting toward a more individualized and empowered approach, where strategic monitoring plays a central role. With mounting evidence showing that personalized tracking enhances metformin’s effectiveness, patients and clinicians alike are rethinking traditional norms around when and how often to check blood glucose for type 2 diabetes. No longer is it sufficient to rely solely on fasting readings or occasional checks. Instead, the focus has turned to creating dynamic, data-informed strategies that reflect each patient’s unique physiology, daily routine, and health goals.
By identifying the best time to check blood sugar for type 2 diabetes with metformin, patients can align their monitoring with the drug’s pharmacological action, uncovering insights that enhance therapeutic outcomes. Likewise, understanding how often to check blood glucose for type 2 diabetes provides the flexibility to adapt monitoring to life’s changing rhythms—whether that means more frequent checks during illness or reduced testing during stable periods.
Ultimately, type 2 diabetes monitoring is no longer just a clinical task—it is a powerful self-management tool. As technology continues to evolve and patient education improves, the potential for more accurate, effective, and personalized care is greater than ever. With the right knowledge, tools, and support, patients can become active participants in their health journey, using smart monitoring to unlock the full benefits of metformin and live healthier, more informed lives.
Further Reading:
When is the best time to check blood sugar with type 2 diabetes?
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.