Arterial pressure is more than just a number measured during a routine checkup; it is a vital indicator of cardiovascular health, reflecting the force that blood exerts on the walls of the arteries as it travels from the heart to the rest of the body. This pressure is fundamental to the proper functioning of the circulatory system, ensuring that oxygen and nutrients are efficiently delivered to tissues and organs. When this delicate balance is disrupted, it can lead to a cascade of complications, from hypertension and heart disease to organ damage. In this comprehensive exploration of arterial pressure, we examine its definition, underlying mechanisms, clinical significance, and the broader implications for public health. We will also address how arterial pressure is measured, what constitutes normal versus abnormal values, and how understanding this parameter is critical for early detection and prevention of serious cardiovascular disorders.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention

Understanding the Arterial Pressure Definition
The arterial pressure definition refers to the pressure exerted by circulating blood upon the walls of the arteries. This pressure is a result of the pumping action of the heart and the resistance offered by the arterial walls. It is typically measured in millimeters of mercury (mmHg) and expressed as two numbers: systolic and diastolic pressure. Systolic pressure represents the force when the heart contracts and pushes blood out into the arteries, while diastolic pressure indicates the pressure when the heart is at rest between beats. These two values together provide a comprehensive snapshot of how the heart and blood vessels are functioning.
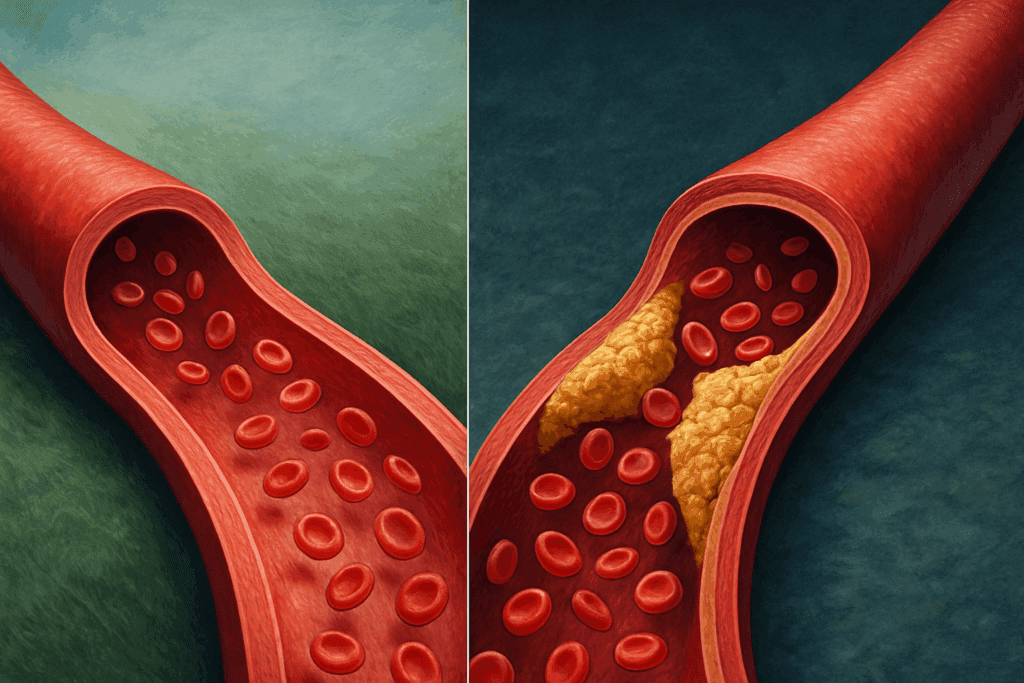
To comprehend what is arterial pressure in greater depth, it is helpful to understand that it reflects the interplay between cardiac output and systemic vascular resistance. Cardiac output is the amount of blood the heart pumps per minute, and vascular resistance is determined by the diameter and elasticity of the arteries. Thus, any condition that affects heart function or vascular tone can significantly alter arterial pressure. For instance, stiffened arteries due to aging or atherosclerosis increase resistance, raising arterial pressure even if cardiac output remains unchanged.
The phrase “blood pressure is the product of” a number of interacting variables underscores the complex physiology behind arterial pressure. In fact, blood pressure is the product of cardiac output and peripheral resistance, two factors regulated by neural, hormonal, and renal mechanisms. An understanding of these relationships is essential for clinicians seeking to manage disorders such as hypertension, where both elements may be dysregulated.
The Physiology Behind Arterial Pressure Regulation
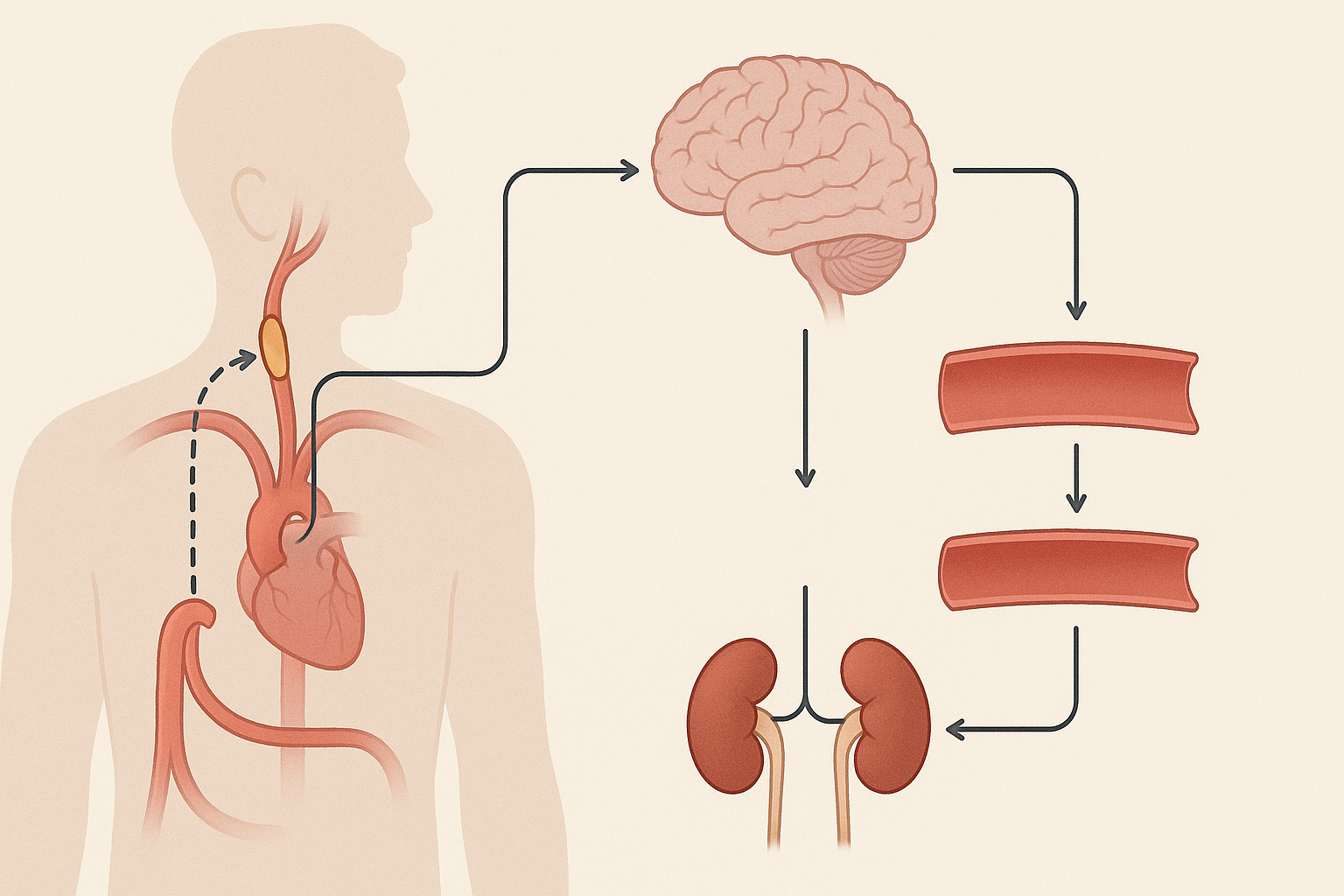
The regulation of arterial pressure involves a finely tuned network of sensors and effectors throughout the body. The baroreceptor reflex, located in the carotid sinus and aortic arch, plays a key role in short-term regulation. When blood pressure rises, baroreceptors are activated, sending signals to the brainstem to decrease heart rate and dilate blood vessels. Conversely, a drop in pressure prompts a sympathetic response to increase heart rate and constrict vessels, thereby elevating arterial pressure.
Long-term regulation, on the other hand, is largely governed by the kidneys and the renin-angiotensin-aldosterone system (RAAS). When blood volume or pressure falls, the kidneys release renin, triggering a hormonal cascade that ultimately increases sodium and water retention, thus raising blood volume and pressure. This system is crucial in maintaining constant pressure in the walls of the arteries over time, despite changes in posture, hydration, or activity level.
Hormones such as antidiuretic hormone (ADH) and atrial natriuretic peptide (ANP) also influence blood volume and vessel tone, contributing to overall arterial pressure control. These overlapping mechanisms ensure that arterial pressure remains within a range that supports tissue perfusion without damaging the delicate vascular endothelium.
Clinical Measurement and Interpretation of Blood Pressure
Blood pressure is one of the most commonly measured vital signs in clinical practice. It is typically assessed using a sphygmomanometer and stethoscope or automated digital devices. The process involves inflating a cuff around the upper arm to occlude blood flow, then slowly releasing the pressure while listening for characteristic sounds (Korotkoff sounds) that signify systolic and diastolic pressures. Accurate measurement is essential, as even small deviations can signal significant cardiovascular risk.
Understanding bp mein, or blood pressure readings in the clinical context, requires knowledge of what constitutes normal and abnormal values. A typical healthy reading is around 120/80 mmHg, where 120 represents the systolic and 80 the diastolic pressure. Prehypertension begins at 120-139/80-89 mmHg, while hypertension is diagnosed when values consistently exceed 140/90 mmHg. Hypotension, or abnormally low blood pressure, may be considered problematic when it leads to symptoms like dizziness or fainting.
Blood pressure readings can be influenced by various factors, including emotional state, recent physical activity, time of day, and medication use. White coat hypertension, for instance, refers to elevated readings in a clinical setting due to anxiety, which may not reflect true baseline pressure. Ambulatory or home monitoring may be necessary to obtain accurate assessments over time.
Arterial Pressure and Cardiovascular Risk
Elevated arterial pressure is a major risk factor for a range of cardiovascular diseases, including heart attack, stroke, heart failure, and chronic kidney disease. The constant pressure in the walls of the arteries is one of the driving forces behind vascular damage, particularly when levels are chronically high. This sustained mechanical stress can lead to endothelial dysfunction, arterial stiffness, and the formation of atherosclerotic plaques, all of which compromise blood flow and increase the risk of ischemic events.
Hypertension, often dubbed the “silent killer,” typically presents with no symptoms until significant damage has occurred. That is why regular screening and early intervention are so crucial. Lifestyle factors such as diet, exercise, alcohol intake, and stress levels significantly influence arterial pressure and are key targets for both prevention and management strategies.
Moreover, emerging research suggests that variability in blood pressure readings—rather than just absolute values—may be an independent risk factor for cardiovascular events. This reinforces the importance of maintaining steady, well-regulated arterial pressure rather than simply focusing on singular readings. For patients and clinicians alike, a comprehensive approach that considers patterns over time is essential.
Factors That Influence Arterial Pressure
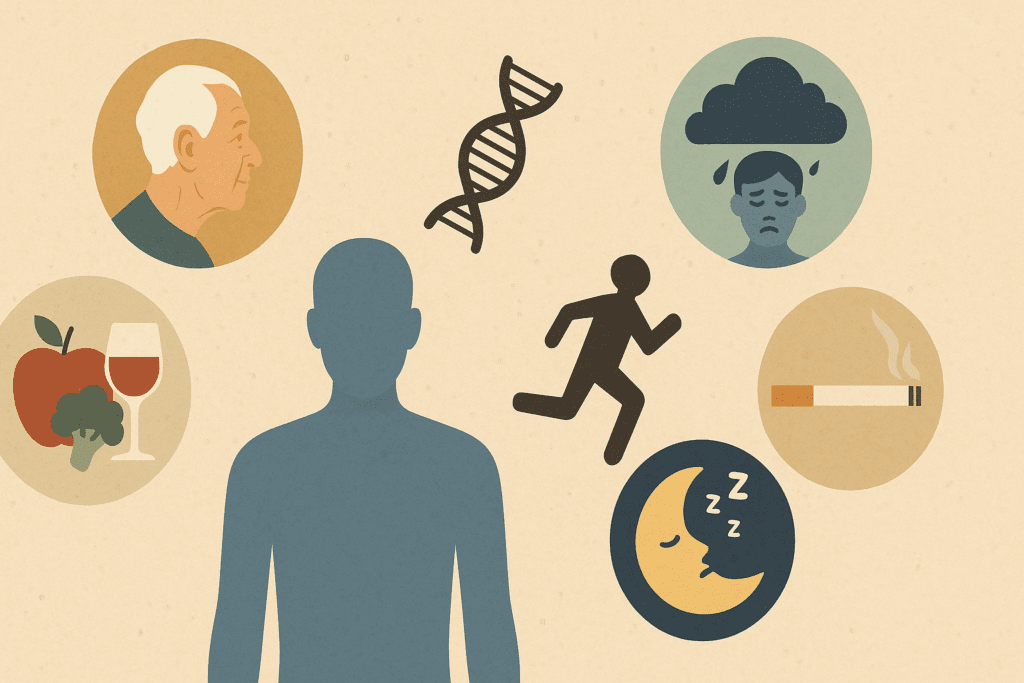
Numerous intrinsic and extrinsic factors influence arterial pressure. Age is a significant determinant; as individuals grow older, arterial walls lose elasticity, contributing to increased systolic pressure. Genetics also play a role, with a family history of hypertension raising the likelihood of developing similar issues. Ethnic background has been shown to correlate with differing risks, with some populations displaying higher baseline pressures and greater sensitivity to salt intake.
Lifestyle choices are among the most modifiable risk factors. Diets high in sodium and low in potassium can elevate arterial pressure, while excessive alcohol consumption and sedentary behavior exacerbate the problem. Smoking, by damaging the vascular endothelium and increasing sympathetic nervous activity, also contributes to chronic hypertension.
Sleep disorders, such as obstructive sleep apnea, are increasingly recognized as contributors to elevated arterial pressure. These conditions cause intermittent drops in oxygen levels, prompting repeated surges in sympathetic activity that strain the cardiovascular system over time. Stress, whether acute or chronic, can also elevate blood pressure by triggering hormonal pathways that tighten blood vessels and increase heart rate.
Pathophysiological Consequences of Abnormal Arterial Pressure
The consequences of uncontrolled arterial pressure extend far beyond the circulatory system. In the brain, elevated pressure can lead to strokes, both ischemic and hemorrhagic. Chronic hypertension accelerates cognitive decline and increases the risk of dementia, possibly by impairing cerebral blood flow and damaging microvasculature. In the eyes, hypertensive retinopathy can cause vision loss through damage to retinal vessels.
In the heart, the increased workload caused by high arterial pressure can lead to left ventricular hypertrophy, a thickening of the heart muscle that reduces efficiency and predisposes to heart failure. The kidneys are also vulnerable, as their delicate filtration system relies on stable perfusion pressure. Chronic hypertension is a leading cause of end-stage renal disease, necessitating dialysis or transplantation.
Low arterial pressure, though less frequently discussed, can also be problematic. Hypotension may lead to inadequate perfusion of vital organs, causing fatigue, confusion, and even shock in severe cases. Conditions such as Addison’s disease, severe dehydration, or autonomic dysfunction can impair the body’s ability to maintain adequate pressure, posing risks of organ failure and death.
Strategies for Maintaining Healthy Arterial Pressure
Maintaining healthy arterial pressure is one of the most effective ways to reduce the risk of cardiovascular disease. Lifestyle modifications form the cornerstone of prevention and management. A diet rich in fruits, vegetables, whole grains, and lean proteins—such as the DASH (Dietary Approaches to Stop Hypertension) diet—has been shown to significantly lower blood pressure. Reducing sodium intake, increasing physical activity, and achieving a healthy body weight are equally important.
Regular aerobic exercise helps improve vascular elasticity and lowers systemic resistance, directly contributing to healthier arterial pressure. Activities such as walking, swimming, or cycling performed for at least 150 minutes per week have been shown to yield measurable benefits. Resistance training can also be incorporated to enhance muscular and metabolic health.
Stress management techniques, including mindfulness meditation, deep breathing exercises, and cognitive behavioral therapy, can mitigate the neurohormonal responses that drive up arterial pressure. For individuals with sleep apnea, continuous positive airway pressure (CPAP) therapy can reduce nighttime spikes in blood pressure and improve overall cardiovascular outcomes.
Pharmacological Treatments for Hypertension and Hypotension
When lifestyle interventions are insufficient, pharmacological therapy becomes necessary. Antihypertensive medications are diverse in their mechanisms and include diuretics, ACE inhibitors, angiotensin receptor blockers (ARBs), beta-blockers, and calcium channel blockers. These agents act at different points in the regulatory pathways to reduce arterial pressure safely and effectively.
Selection of medication depends on patient-specific factors such as age, comorbid conditions, and risk profile. For example, ACE inhibitors are often preferred in patients with diabetes due to their renal protective effects, while beta-blockers may be used in individuals with coronary artery disease or arrhythmias. Combination therapy may be required in resistant hypertension to achieve target pressures.
For hypotension, treatment focuses on identifying and addressing the underlying cause. Volume expansion through fluid resuscitation, use of vasopressors, or hormone replacement in adrenal insufficiency are among the therapeutic options. In cases of orthostatic hypotension, compression stockings and gradual positional changes may help prevent symptomatic drops in pressure.
Emerging Research and Future Directions
Recent advances in biomedical research are shedding light on the molecular underpinnings of arterial pressure regulation. Genetic studies have identified polymorphisms that predispose individuals to hypertension, opening avenues for personalized medicine. Researchers are also exploring the gut microbiome’s influence on blood pressure, with certain bacterial profiles linked to lower or higher readings.
Novel technologies such as wearable blood pressure monitors and implantable sensors are enhancing our ability to track arterial pressure continuously and non-invasively. These tools allow for earlier detection of abnormal trends and more responsive management strategies. Artificial intelligence is being integrated into diagnostics and treatment planning, potentially improving outcomes through predictive analytics.
Meanwhile, public health initiatives focused on education, screening, and access to care are critical in addressing the global burden of hypertension. As awareness grows, so too does the opportunity for early intervention and improved long-term health outcomes. Future research will likely continue to refine our understanding of how best to maintain constant pressure in the walls of the arteries and prevent the complications associated with dysregulation.
Frequently Asked Questions: Arterial Pressure and Cardiovascular Health
1. How does long-term stress affect arterial pressure regulation?
Long-term stress plays a subtle yet powerful role in disrupting the body’s ability to maintain stable arterial pressure. Chronic stress activates the sympathetic nervous system and the hypothalamic-pituitary-adrenal (HPA) axis, resulting in increased secretion of cortisol and adrenaline. These hormones elevate heart rate and induce vasoconstriction, gradually leading to higher baseline blood pressure. Over time, this persistent state contributes to reduced vascular elasticity and endothelial damage, complicating the body’s efforts to sustain constant pressure in the walls of the arteries. Although stress doesn’t directly alter the arterial pressure definition, its physiological impact shows how emotional and psychological well-being intertwine with cardiovascular resilience.
2. Are there differences in arterial pressure patterns between men and women?
Yes, there are sex-specific variations in how arterial pressure behaves across the lifespan. Premenopausal women typically have lower blood pressure than men due to the protective effects of estrogen on vascular tone and elasticity. However, after menopause, women often experience a rapid increase in arterial pressure, sometimes surpassing their male counterparts. The shift emphasizes that blood pressure is the product of hormonal balance in addition to mechanical and renal factors. Understanding what is arterial pressure requires recognizing how biological sex influences the development and management of cardiovascular risk factors over time.
3. How does altitude influence arterial pressure and cardiovascular function?
Exposure to high altitude presents a unique challenge for maintaining adequate arterial pressure. In low-oxygen environments, the body compensates by increasing respiratory rate and heart output, which can elevate systemic blood pressure temporarily. Some individuals may develop high-altitude hypertension, especially during prolonged stays at elevation. The arterial pressure definition must then be understood within environmental context—adaptive responses such as increased red blood cell production can modify how blood pressure is regulated. Those with pre-existing cardiovascular conditions should be especially cautious when traveling to high altitudes, as the constant pressure in the walls of the arteries can be destabilized.
4. Can hydration levels significantly impact arterial pressure?
Hydration has a surprisingly influential role in maintaining healthy blood pressure levels. Dehydration leads to reduced blood volume, which in turn can cause a drop in arterial pressure, particularly during postural changes—a phenomenon known as orthostatic hypotension. Conversely, overhydration in individuals with impaired kidney function or heart failure may lead to elevated pressure due to fluid overload. These fluctuations exemplify that blood pressure is the product of complex homeostatic mechanisms, including fluid balance. For patients monitoring bp mein or managing hypotension, maintaining consistent hydration is a critical and often overlooked lifestyle factor.
5. How do medications for unrelated conditions affect arterial pressure?
Certain medications not primarily intended for cardiovascular use can still influence arterial pressure significantly. For example, corticosteroids may raise blood pressure by promoting sodium retention, while some antidepressants and non-steroidal anti-inflammatory drugs (NSAIDs) can induce vasoconstriction. On the other hand, alpha-blockers used for prostate enlargement may lower blood pressure too aggressively, especially when changing positions. When considering what is arterial pressure in a clinical setting, it’s crucial to evaluate medication profiles holistically. The risk of disrupting constant pressure in the walls of the arteries becomes more likely when polypharmacy is involved, especially among older adults.
6. What role does sleep play in regulating blood pressure rhythms?
Sleep is essential for maintaining circadian patterns in arterial pressure, with most individuals experiencing a natural dip in blood pressure during nighttime rest—a phenomenon known as nocturnal dipping. However, in conditions like sleep apnea or chronic insomnia, this pattern is disrupted, leading to non-dipping or even reverse-dipping profiles associated with increased cardiovascular risk. The disruption affects how blood pressure is the product of neural and hormonal rhythms that should synchronize during sleep. Patients with altered sleep architecture often exhibit poor morning bp mein readings, highlighting the importance of restorative sleep for cardiovascular health.
7. Is there a connection between gut health and arterial pressure regulation?
Emerging research points to a compelling link between gut microbiota and blood pressure regulation. The composition of the gut flora can influence systemic inflammation, insulin sensitivity, and even vascular tone through metabolites like short-chain fatty acids. These microbial byproducts interact with receptors in blood vessels, modulating how tightly or loosely they constrict. As such, arterial pressure is the product of not only cardiovascular mechanisms but also gastrointestinal health. While the arterial pressure definition may not explicitly include gut microbiota, integrative models of care increasingly recognize its influence.
8. How do elite athletes manage fluctuations in arterial pressure during training and competition?
Elite athletes experience dynamic shifts in arterial pressure due to the physiological demands of intense physical activity. During exercise, systolic pressure rises significantly to meet oxygen delivery demands, while diastolic pressure may remain stable or drop slightly. Training adaptation allows their cardiovascular systems to tolerate these spikes without sustained injury, partly due to superior vascular elasticity. Understanding what is arterial pressure in this population involves distinguishing between transient, functional elevations and pathological hypertension. Advanced monitoring techniques, including continuous bp mein tracking, are often used to tailor training loads and recovery protocols.
9. Are there cultural or dietary practices that uniquely support healthy arterial pressure?
Yes, various traditional dietary practices have been associated with better arterial pressure profiles. The Mediterranean diet, rich in omega-3 fatty acids, polyphenols, and plant-based foods, is known to enhance endothelial function and reduce inflammation. Similarly, the Japanese diet, which emphasizes fish, seaweed, and fermented foods, supports a healthy microbiome and blood pressure balance. These dietary patterns reflect an understanding that blood pressure is the product of lifestyle, genetics, and cultural context. By supporting constant pressure in the walls of the arteries through nutrient-rich foods, these diets offer preventative cardiovascular benefits.
10. What technological advancements are shaping the future of blood pressure management?
Recent innovations are transforming how arterial pressure is monitored and managed. Wearable devices now offer real-time bp mein tracking, allowing for more personalized treatment plans and earlier intervention in high-risk individuals. Some advanced systems use pulse wave analysis or optical sensors to estimate arterial pressure without a traditional cuff. Additionally, AI-driven algorithms can analyze longitudinal data to detect subtle trends, providing insights beyond the basic arterial pressure definition. These technologies are bridging the gap between static clinical snapshots and dynamic, everyday cardiovascular monitoring, offering new hope in preventing long-term complications.
Conclusion: Why Understanding Arterial Pressure Matters for Lifelong Cardiovascular Wellness
Understanding what is arterial pressure is not merely an academic exercise—it is a cornerstone of proactive cardiovascular care. From the arterial pressure definition rooted in fundamental physiology to the clinical implications of maintaining or losing control over this vital metric, the importance of arterial pressure cannot be overstated. When we consider that blood pressure is the product of complex interactions between the heart, vessels, and regulatory systems, it becomes clear that monitoring and managing it effectively is both an art and a science.
Whether evaluating bp mein in a primary care setting or exploring the mechanisms that ensure constant pressure in the walls of the arteries, healthcare professionals and patients alike benefit from a deeper grasp of these processes. With chronic diseases like hypertension on the rise globally, the call to action is clear: adopt healthy lifestyles, adhere to evidence-based therapies, and engage with preventive care.
By fostering awareness and education around arterial health, we empower individuals to take control of their well-being. In doing so, we reduce the burden of disease, enhance quality of life, and contribute to a healthcare system focused not only on treatment but also on prevention. In every heartbeat, arterial pressure tells a story—one of strength, resilience, and the continuous flow of life.
heart health monitoring, vascular resistance, circulatory system function, systolic and diastolic pressure, cardiovascular wellness, high blood pressure management, hypotension causes, hypertension treatment options, blood vessel elasticity, cardiac output regulation, autonomic nervous system, baroreceptor reflex, kidney and blood pressure, renin angiotensin system, endothelial function, lifestyle and blood pressure, aging and cardiovascular health, silent hypertension risks, blood flow dynamics, chronic disease prevention
Further Reading:
Physiology, Mean Arterial Pressure