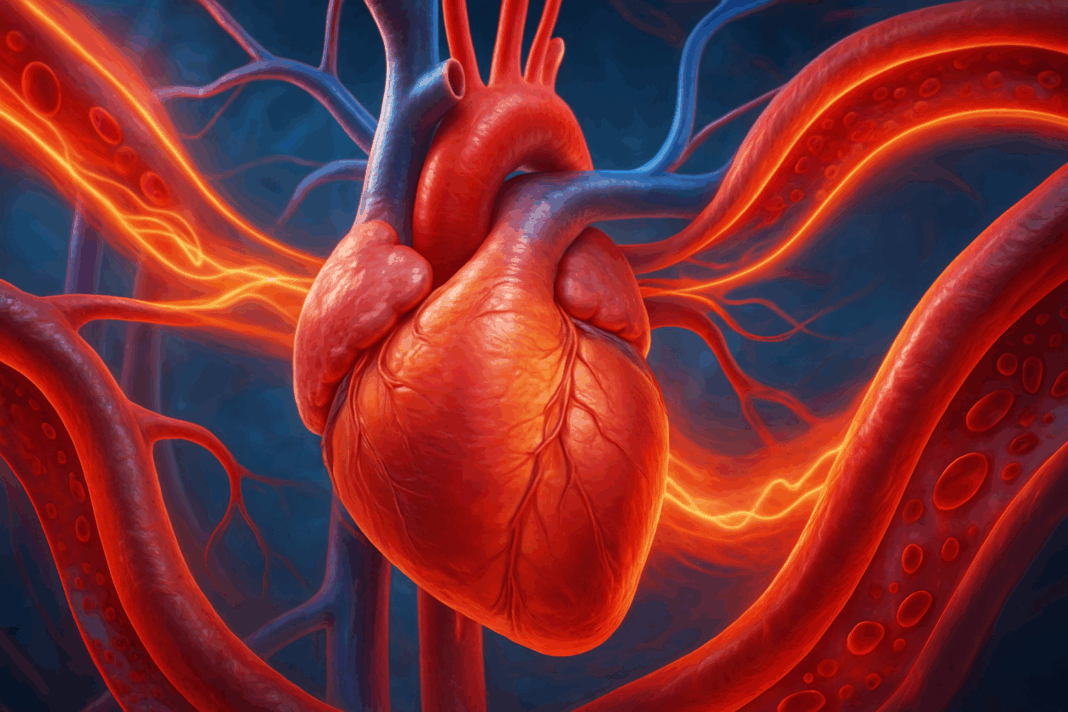
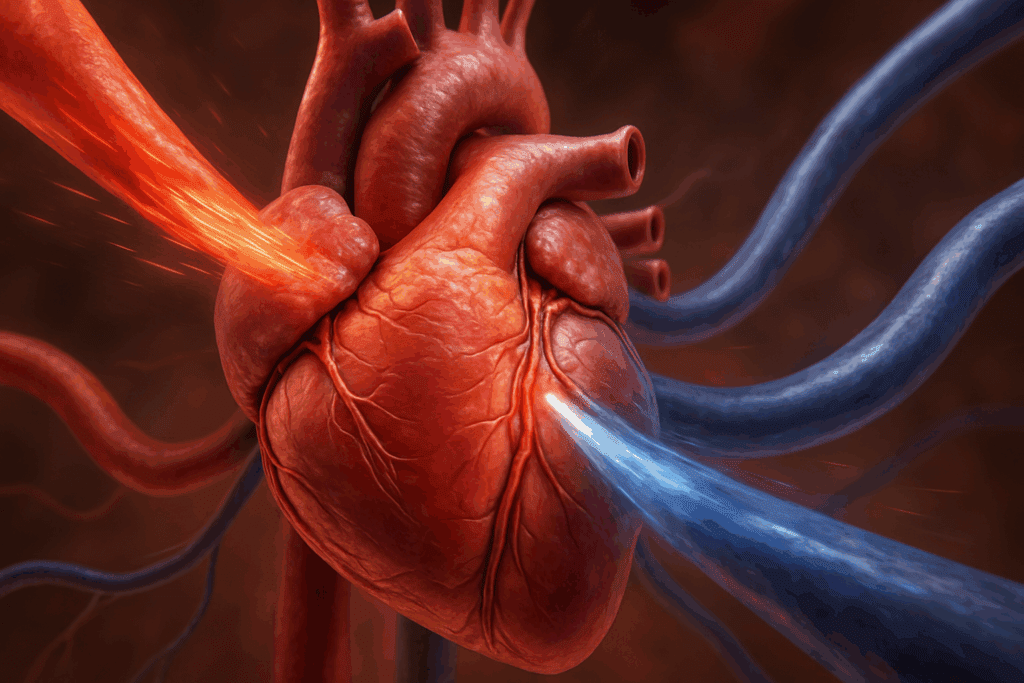
The human cardiovascular system is a complex and dynamic network that relies on finely tuned physiological processes to maintain homeostasis and ensure adequate blood flow to tissues throughout the body. Among the most critical parameters governing cardiovascular function is blood pressure, which represents the force exerted by circulating blood on the walls of the body’s arteries and veins. Within this realm, systolic vascular pressure emerges as a particularly important component, offering insight into the health and functionality of the heart during contraction phases. To grasp the full implications of systolic vascular pressure, it is essential to explore the forces exerted on arterial and venous walls during different cardiac events, including atrial and ventricular contractions and relaxations.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Understanding Arterial Blood Pressure: A Foundational Overview
Arterial blood pressure is determined by the interplay between cardiac output and systemic vascular resistance. It represents the force that blood exerts on arterial walls as it is pumped from the heart through the circulatory system. Typically measured as two values—systolic and diastolic pressure—this parameter is critical in diagnosing and managing various cardiovascular disorders. Systolic pressure, in particular, reflects the peak force within arteries when the heart’s ventricles contract. Factors such as arterial stiffness, blood volume, and heart rate directly affect these readings, and abnormalities in arterial blood pressure often signal underlying pathologies such as hypertension, heart failure, or atherosclerosis.
When discussing arterial blood pressure in the context of atrial activity, it becomes essential to distinguish between the mechanical contributions of the atria and those of the ventricles. While the ventricles contribute the majority of the pressure that propels blood through the systemic and pulmonary circuits, the atria also exert subtle but meaningful forces that influence overall hemodynamics. The force exerted on arterial walls during atrial contraction, for example, though smaller in magnitude, plays a supporting role in ensuring effective ventricular filling and preloading, thereby indirectly influencing systolic pressure.
The Force Exerted on Arterial Walls During Atrial Contraction
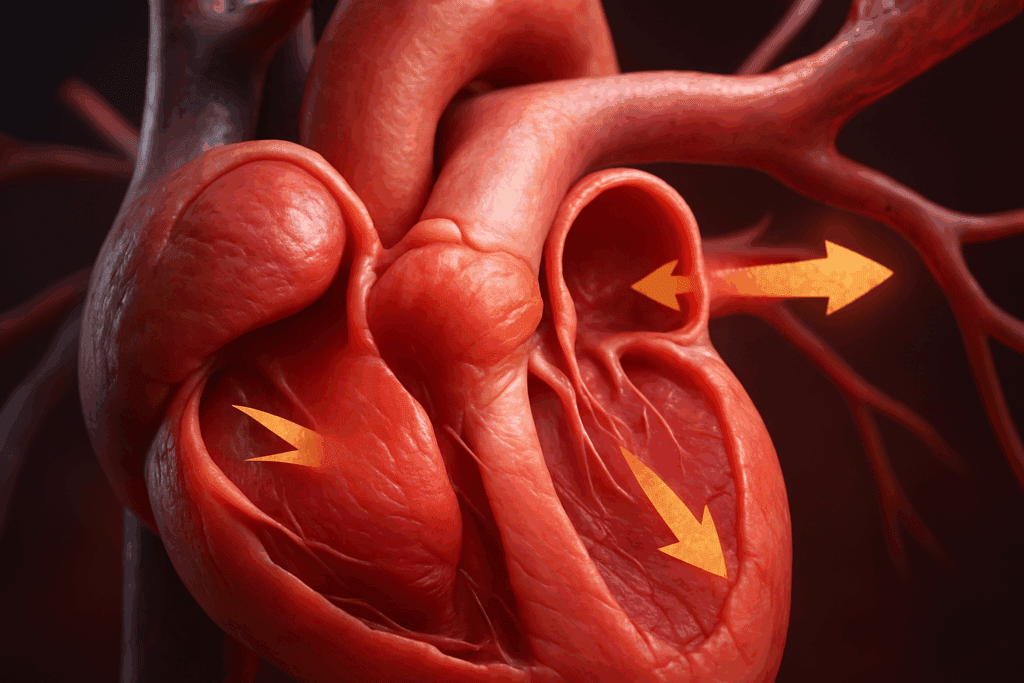
During atrial contraction, or atrial systole, the atria contract to push the remaining blood into the ventricles. This action, although relatively gentle compared to ventricular contraction, contributes to the final phase of ventricular filling and affects preload. The force exerted on arterial walls during atrial contraction is not as pronounced as that produced by the ventricles, but it plays an important priming role. By increasing ventricular end-diastolic volume, atrial contraction sets the stage for a more forceful ventricular systole. This increased preload enhances stroke volume through the Frank-Starling mechanism, ultimately influencing systolic vascular pressure.
Although the direct force exerted on arterial walls during atrial contraction is minimal, its indirect impact on arterial blood pressure should not be underestimated. In patients with impaired atrial contraction, such as those with atrial fibrillation, the loss of this “atrial kick” can lead to reduced cardiac output and suboptimal blood pressure regulation. Clinical studies have demonstrated that in such scenarios, particularly in patients with stiff ventricles or diastolic dysfunction, the absence of effective atrial contraction results in diminished preload, compromised systolic pressure, and symptomatic hypotension.
The Force Exerted on Venous Walls During Atrial Contracting
Venous return to the heart is a passive process influenced by pressure gradients and assisted by mechanisms such as skeletal muscle contraction and thoracic pressure changes. During atrial contraction, there is a transient increase in atrial pressure, which can lead to a brief rise in pressure within the venae cavae and other nearby veins. The force exerted on the venous walls during atrial contracting is modest, but it carries physiological significance in terms of modulating venous flow and maintaining the continuity of circulation.
This small yet measurable force can contribute to minor backpressure within the venous system, particularly when venous valves are functioning correctly. In cases where valve insufficiency exists, atrial contraction may exacerbate venous reflux, especially in peripheral veins. Additionally, in conditions such as right-sided heart failure or tricuspid regurgitation, atrial contraction may cause visibly pulsatile neck veins due to this force transmission. These phenomena underscore the interconnectedness between atrial mechanics and venous hemodynamics and highlight the role of atrial contracting forces in systemic circulatory integrity.
What Influences Systolic Vascular Pressure?
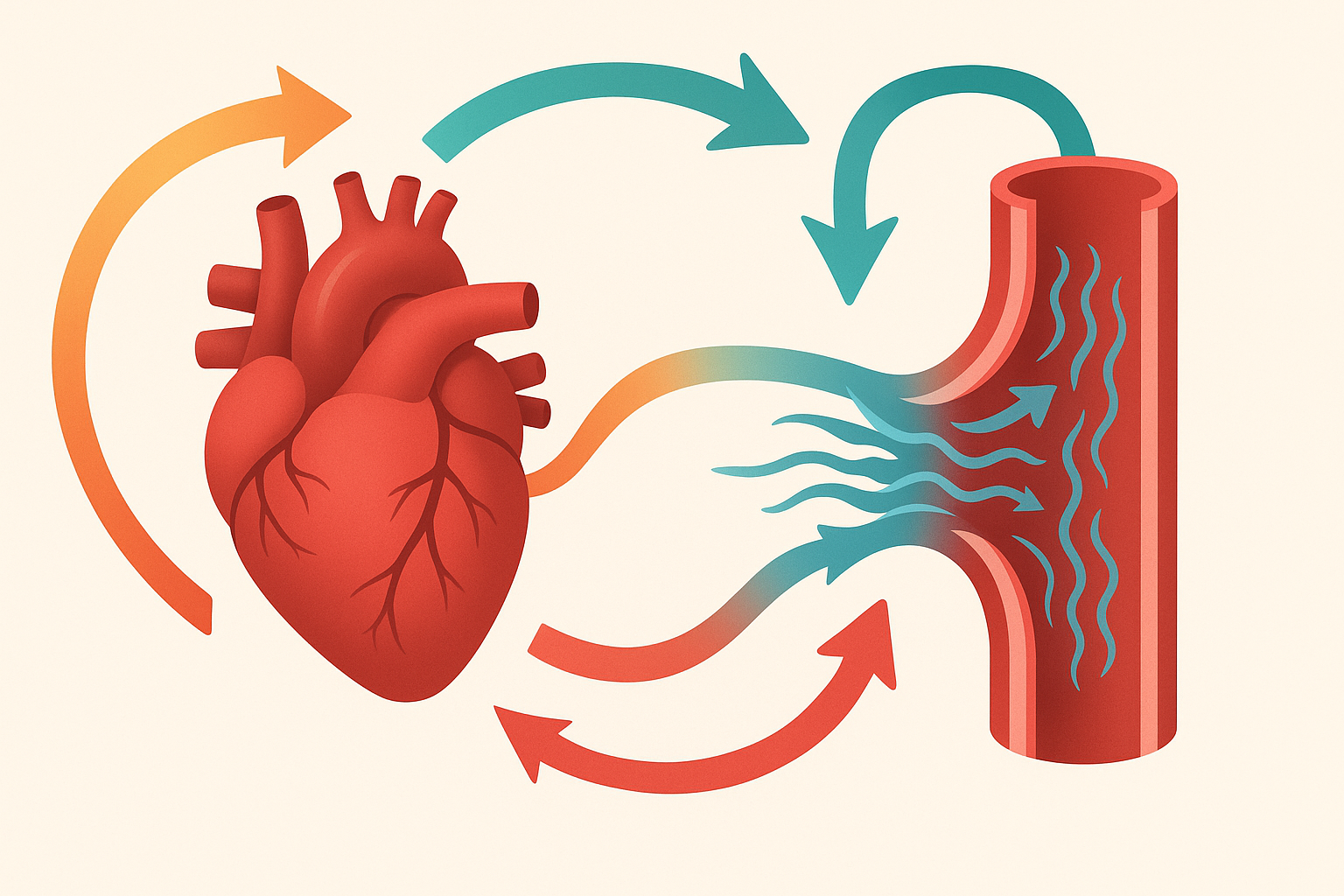
Systolic vascular pressure is primarily influenced by three critical components: cardiac output, arterial compliance, and peripheral vascular resistance. Cardiac output, determined by heart rate and stroke volume, plays the most direct role. When the heart contracts with greater force, it ejects more blood into the arterial system, raising systolic pressure. Conversely, a weakened heart will yield lower output and reduced systolic values. Stroke volume itself is influenced by preload, afterload, and myocardial contractility, all of which are modifiable through both physiological and pharmacological means.
Arterial compliance refers to the elasticity of the arterial walls. Younger, healthier arteries can expand to accommodate surges in blood flow during systole, effectively dampening the rise in pressure. In contrast, aged or atherosclerotic arteries are stiffer, resulting in higher systolic pressures for the same volume of ejected blood. This reduced compliance is a key reason why systolic hypertension becomes more prevalent with age. Peripheral vascular resistance, governed by the tone of arterioles, also significantly influences systolic pressure. Vasoconstriction elevates resistance and thus raises systolic values, while vasodilation lowers them.
Other factors that influence systolic vascular pressure include blood viscosity, body position, hydration status, and neurohormonal activity. For instance, activation of the sympathetic nervous system increases both heart rate and vascular tone, thereby elevating systolic pressure. Hormones such as epinephrine and angiotensin II can exert similar effects. Understanding these influences is crucial for managing conditions like hypertension and for optimizing hemodynamic performance in patients with heart disease.
The Force Exerted on Venous Walls During Ventricular Contraction
During ventricular systole, the ventricles contract forcefully to eject blood into the aorta and pulmonary artery. This event is associated with a significant rise in intraventricular pressure, which is then transmitted into the arterial circulation. However, this phase also has implications for the venous system. The force exerted on venous walls during ventricular contraction is primarily felt in the central veins and the atria due to the transmission of pressure through the cardiac chambers and valves.
In the context of the right side of the heart, the contraction of the right ventricle can momentarily impede venous return, causing a brief elevation in central venous pressure. This phenomenon, known as the “v” wave in venous pulse tracings, reflects the mechanical interplay between ventricular contraction and venous dynamics. While this force is not typically strong enough to cause retrograde flow, it can become clinically relevant in pathological conditions. In heart failure or when there is tricuspid valve dysfunction, the force of ventricular contraction may result in exaggerated venous distension and congestion.
The interplay between ventricular contraction and venous wall pressure also has implications for medical procedures such as central venous catheterization and fluid management. Clinicians must account for these transient pressure changes to ensure accurate hemodynamic monitoring. Moreover, the systemic venous response to ventricular contraction becomes increasingly important in critical care settings where rapid shifts in intrathoracic pressures and preload volumes can alter patient outcomes.
The Force Exerted on Arterial Walls During Atrial Relaxation
Atrial relaxation, or atrial diastole, occurs after atrial contraction and during the early stages of ventricular systole. During this phase, the atria become receptive chambers, filling with blood from the venous system. The force exerted on arterial walls during atrial relaxation is minimal, as the atria are not actively contracting. However, this phase is essential for setting up the subsequent cycle of cardiac function and ensuring optimal preload for the ventricles.
While the direct mechanical impact on arterial walls is negligible, the timing of atrial relaxation relative to ventricular contraction plays a role in maintaining synchronized cardiac output and stable arterial blood pressure. If atrial relaxation is impaired, as in the case of atrial stiffness or infiltrative cardiomyopathies, the overall efficiency of ventricular filling may decrease. This can lead to reduced stroke volume and lower systolic vascular pressure, emphasizing the indirect but vital contribution of atrial diastole to arterial hemodynamics.
Moreover, atrial relaxation facilitates the creation of a suction effect that aids venous return. This passive mechanism supports continuous circulation and indirectly stabilizes arterial pressure by promoting effective ventricular filling. When atrial relaxation is dysfunctional, it may manifest as elevated pulmonary pressures, diminished exercise tolerance, or impaired diastolic function, further illustrating its systemic implications.
The Force Exerted on Venous Walls During Atrial Relaxation
Just as atrial contraction exerts modest force on the venous system, atrial relaxation has complementary effects. During atrial relaxation, the atrial chambers expand to accommodate incoming venous blood. This expansion creates a slight vacuum effect, encouraging blood flow from the veins into the atria. The force exerted on venous walls during atrial relaxation is thus characterized by a decrease in resistance and pressure, which facilitates venous drainage and supports overall circulatory flow.
This phase of the cardiac cycle is particularly important in conditions where venous return is compromised. In patients with heart failure or pericardial constraint, the ability of the atria to fully relax and accommodate blood is diminished. This can lead to increased venous pressures, distension, and symptoms such as jugular venous distention and peripheral edema. Recognizing the subtle but significant role of atrial relaxation in venous dynamics is crucial for understanding the full scope of cardiovascular physiology.
Furthermore, the effective transmission of low-pressure gradients during atrial relaxation underscores the need for intact structural and functional properties of the atrial myocardium. Conditions such as atrial fibrosis, inflammation, or scarring can disrupt this process, leading to altered venous return and systemic congestion. Therapeutic strategies aimed at preserving atrial compliance and diastolic function may therefore hold promise in mitigating these adverse outcomes.
The Interplay Between Blood Pressure and Arterial Pressure in Clinical Practice
Although often used interchangeably, blood pressure and arterial pressure are not entirely synonymous. Blood pressure typically refers to the pressure within the arteries, which is what clinicians measure when assessing cardiovascular health. Arterial pressure, however, can more broadly encompass pressure within all arteries, including systemic and pulmonary circulations. Understanding the nuances between these terms enhances diagnostic accuracy and guides therapeutic interventions.
In clinical settings, precise knowledge of arterial pressure components allows for targeted management of various cardiovascular conditions. For example, elevated systolic arterial pressure may indicate increased stroke volume or decreased arterial compliance, while low systolic pressure might suggest reduced cardiac output or hypovolemia. By interpreting these values in the context of atrial and ventricular mechanics, healthcare providers can make informed decisions about fluid management, vasopressor use, and long-term antihypertensive therapy.
Moreover, integrating information about the force exerted on arterial walls during atrial contraction and relaxation provides valuable insight into diastolic function and preload status. Similarly, evaluating the force exerted on venous walls during both atrial and ventricular activity sheds light on venous return and right heart function. These assessments are particularly important in patients with complex hemodynamic profiles, such as those with heart failure with preserved ejection fraction or pulmonary hypertension.
Frequently Asked Questions: Understanding Forces in Cardiovascular Pressure Dynamics
What role does body posture play in the force exerted on arterial walls during atrial contraction?
Body posture significantly affects how gravity influences blood distribution and pressure gradients within the cardiovascular system. When standing, gravity increases the demand on the heart to pump blood upward, which can alter the force exerted on arterial walls during atrial contraction. This added resistance may slightly increase preload and impact the timing of atrial systole. Conversely, in a supine position, venous return is enhanced, potentially modifying the preload and the subsequent contribution of atrial contraction to arterial blood pressure. Although subtle, these posture-related shifts can influence both clinical assessments and interpretations of hemodynamic changes.
How does age impact the force exerted on the venous walls during atrial contracting?
With age, structural changes in the atrial myocardium and venous compliance can significantly influence the force exerted on the venous walls during atrial contracting. Fibrosis and atrial dilation, common in aging hearts, may weaken the contractile efficiency of the atria, reducing their ability to create sufficient forward flow and briefly increasing venous backpressure. Additionally, aged veins often lose their elasticity, making them more susceptible to volume shifts. This combination can lead to more pronounced venous pulsations and, in some cases, venous congestion. Therefore, understanding age-related changes is essential when evaluating abnormal venous responses during atrial contraction.
Can respiratory patterns alter the force exerted on venous walls during ventricular contraction?
Yes, respiratory movements, especially during deep inhalation, can modulate intrathoracic pressure and influence the force exerted on venous walls during ventricular contraction. Inspiration decreases intrathoracic pressure, facilitating venous return, while expiration may transiently impede it. These fluctuations alter central venous pressure, especially during the ventricular systolic phase, and can enhance or reduce venous wall distension depending on the timing. This respiratory-induced variability is particularly relevant during cardiopulmonary assessments and when interpreting jugular venous pulsations. Clinicians often use respiratory phases to better differentiate normal from pathological waveforms in central venous pressure tracings.
Why does atrial relaxation matter for arterial pressure stability?
Although atrial relaxation does not directly produce a powerful forward flow, its role in maintaining arterial pressure stability is often underappreciated. During atrial relaxation, effective ventricular filling is supported, which ensures consistent stroke volume and stable arterial blood pressure. The force exerted on arterial walls during atrial relaxation is indirect, yet it supports preload dynamics that influence subsequent systolic output. Any dysfunction in this phase can cause erratic filling patterns and reduce the reliability of arterial perfusion, especially during increased physiological demand. Conditions like restrictive cardiomyopathy demonstrate how impaired atrial relaxation can contribute to systolic variability and compromised systemic circulation.
How do exercise and physical conditioning affect the force exerted on venous walls during atrial relaxation?
In individuals who engage in regular endurance training, atrial compliance and venous tone often improve, enhancing the efficiency of venous return during atrial relaxation. The force exerted on venous walls during atrial relaxation becomes more synchronized and better regulated in trained hearts, facilitating optimal preload without excessive venous distension. Athletes frequently demonstrate superior ventricular filling due to enhanced atrial function, which supports greater stroke volume. This dynamic adaptability contrasts with deconditioned individuals, who may experience sluggish venous return and inefficient atrial diastolic filling. Thus, exercise not only strengthens myocardial contractility but also refines relaxation mechanics to support circulatory resilience.
How does blood viscosity affect what influences systolic vascular pressure?
Blood viscosity is a lesser-known but critical factor that influences systolic vascular pressure. When blood is more viscous, as in conditions like polycythemia vera or dehydration, it resists flow more strongly, increasing peripheral vascular resistance and elevating systolic pressure. Conversely, in anemic states or with overhydration, reduced viscosity may lead to lower systolic readings due to diminished resistance. These changes can also alter the workload of the left ventricle, potentially leading to compensatory hypertrophy over time. Hence, assessing hematological status is crucial when evaluating the underlying factors of altered systolic vascular pressure.
Are there neurological mechanisms that impact the force exerted on arterial walls during atrial contraction?
Yes, the autonomic nervous system, particularly the sympathetic branch, plays a critical role in modulating the force exerted on arterial walls during atrial contraction. Increased sympathetic tone can enhance atrial contractility through beta-adrenergic stimulation, slightly increasing the contribution of atrial systole to ventricular filling and indirectly affecting arterial pressure. Neurohormonal surges during stress or illness often amplify this effect, which may be observed in hypertensive responses or elevated heart rates. Parasympathetic influence, primarily via the vagus nerve, can reduce atrial contractility and blunt these effects. The interplay between these autonomic influences adds a layer of complexity to cardiac performance, especially during dynamic or pathological states.
How does venous valve dysfunction alter the force exerted on the venous walls during atrial contracting?
In the presence of venous valve incompetence, the force exerted on the venous walls during atrial contracting can cause retrograde blood flow, exacerbating venous pooling and congestion. Normally, venous valves prevent backflow during increased atrial pressure, but when these structures fail, atrial systole can transmit pressure waves inefficiently or even counterproductively. Patients with this condition may present with varicosities, dependent edema, or visible jugular pulsations that reflect disrupted pressure gradients. Such dysfunctions are particularly notable during elevated atrial pressures, as seen in right heart failure or tricuspid valve disease. Timely diagnosis is critical to prevent chronic venous insufficiency and its complications.
In what clinical scenarios does the force exerted on venous walls during ventricular contraction become diagnostically relevant?
The force exerted on venous walls during ventricular contraction is diagnostically significant in conditions like constrictive pericarditis and severe tricuspid regurgitation. In these scenarios, increased right ventricular pressures can cause pronounced “v” waves in venous pressure tracings and visible jugular pulsations. These findings serve as noninvasive markers for clinicians assessing right-sided hemodynamics. Moreover, understanding this force helps differentiate among causes of elevated central venous pressure, such as distinguishing between fluid overload and mechanical impediments to venous return. As a result, these observations are invaluable during echocardiographic evaluation and right-heart catheterization.
What are the clinical implications of misinterpreting blood pressure and arterial pressure interchangeably?
Misusing the terms “blood pressure” and “arterial pressure” interchangeably can lead to diagnostic inaccuracies, especially when managing complex cardiovascular conditions. While arterial pressure refers specifically to pressure within arteries, blood pressure can encompass systemic and pulmonary circulations under varying conditions. Failure to make this distinction might overlook elevated pulmonary arterial pressures in cases of pulmonary hypertension or misinterpret systemic hypotension as purely cardiac in origin. Moreover, targeted therapies often differ based on which type of pressure is affected, requiring clinicians to be precise in their terminology and measurements. Recognizing these nuances ensures more personalized and effective cardiovascular care, particularly in advanced heart failure management and invasive monitoring.
Final Reflections: How Understanding Systolic Vascular Pressure Enhances Cardiovascular Care
Systolic vascular pressure is not merely a numerical value on a blood pressure cuff; it is a reflection of the dynamic and multifaceted forces that govern cardiovascular function. From the subtle contributions of atrial contraction to the powerful thrust of ventricular systole, each phase of the cardiac cycle plays a role in shaping arterial and venous pressures. The force exerted on arterial walls during atrial contraction may seem minor, yet it has important implications for ventricular preload and overall stroke volume. Likewise, the force exerted on the venous walls during atrial contracting or during ventricular contraction provides insights into circulatory efficiency and the potential for congestion or reflux.
By exploring what influences systolic vascular pressure—including cardiac output, vascular resistance, arterial compliance, and neurohormonal factors—clinicians and researchers gain a deeper appreciation of how to optimize hemodynamic performance in both acute and chronic settings. Recognizing the roles of the force exerted on venous walls during atrial relaxation and the force exerted on arterial walls during atrial relaxation further completes the picture of how the heart and vasculature coordinate to sustain life.
Ultimately, advancing our understanding of these interconnected forces allows for more precise, individualized, and effective approaches to diagnosing and treating cardiovascular disorders. In an era of increasingly sophisticated cardiovascular care, such knowledge is not only beneficial but essential for improving patient outcomes and promoting long-term cardiovascular health.
cardiac hemodynamics, heart chamber function, preload and afterload dynamics, ventricular systole mechanics, atrial systole physiology, blood flow regulation, cardiovascular pressure gradients, venous return mechanisms, central venous pressure insights, arterial elasticity and aging, cardiac cycle phases, stroke volume modulation, heart valve dynamics, circulatory efficiency, right heart function, atrial compliance, vascular resistance and hypertension, myocardial performance, echocardiographic hemodynamics, systemic circulation health
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.