Fluctuations in blood pressure are not uncommon, particularly in response to everyday stressors, physical exertion, or emotional distress. However, for some individuals, these fluctuations become a recurring pattern that raises significant health concerns. Known medically as labile hypertension or labile blood pressure, this condition is characterized by sudden and unpredictable spikes and drops in blood pressure levels. Unlike sustained hypertension, labile hypertension is intermittent but can still pose serious risks to cardiovascular health and overall well-being.
Labile blood pressure is often misunderstood or dismissed as mere stress-induced variability. Yet, emerging research highlights that reactive high blood pressure episodes, even if temporary, can contribute to vascular damage, heart strain, and an increased risk of major cardiovascular events. Understanding what labile hypertension is, how it manifests, and what it means for long-term heart health is critical, not only for clinicians but also for individuals seeking clarity and control over their cardiovascular risk profile. As we explore the causes, symptoms, diagnostic challenges, and management strategies associated with this dynamic condition, it becomes clear that labile hypertension demands the same degree of attention as its more persistent counterparts.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Defining Labile Hypertension and Reactive High Blood Pressure
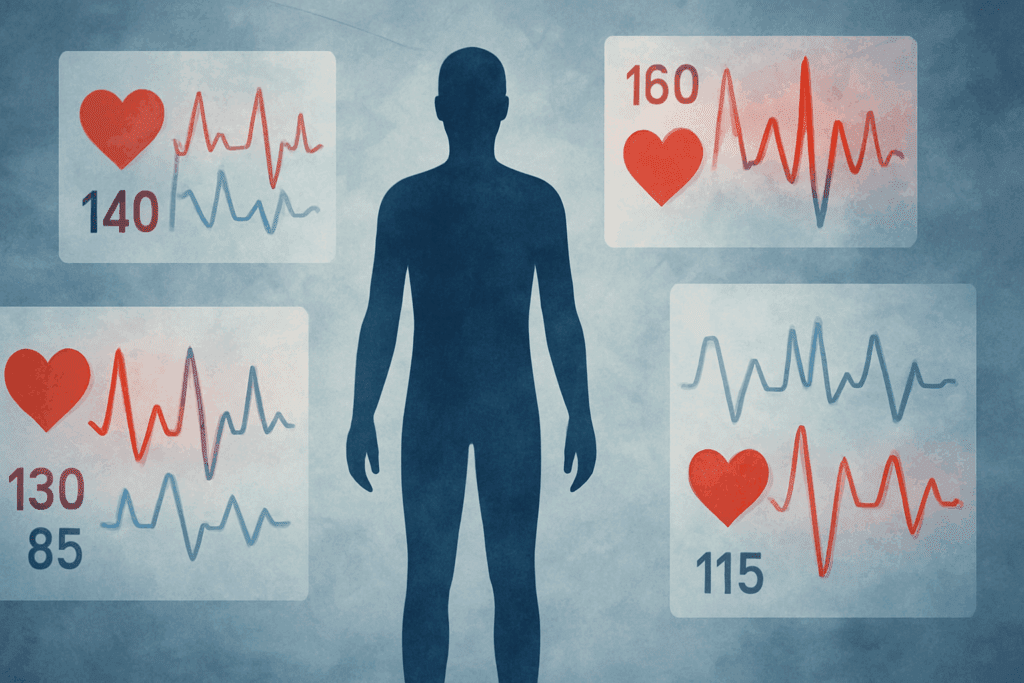
Labile hypertension is a type of blood pressure irregularity defined by sudden changes in systolic and/or diastolic pressure, often without a predictable pattern. These fluctuations may occur several times a day or across longer intervals, depending on the individual and the underlying causes. Although labile blood pressure does not always persist at hypertensive levels, the periodic elevation can still be harmful, especially when combined with other cardiovascular risk factors.
One of the hallmark traits of labile hypertension is its reactivity to emotional, psychological, or situational stimuli. This has led to the interchangeable use of the term “reactive high blood pressure” in clinical discussions. In reactive high blood pressure, the cardiovascular system overreacts to stress, causing temporary spikes in pressure that may return to baseline once the stimulus is removed. For many, this means that visits to a doctor’s office—commonly referred to as “white coat syndrome”—can trigger elevated readings that do not reflect their usual resting values.
Despite its transitory nature, labile hypertension can be difficult to diagnose. Routine in-office blood pressure checks may miss these episodic spikes, leading to underdiagnosis or misclassification. Ambulatory blood pressure monitoring, which records readings over a 24-hour period, is often more effective in detecting the pattern of variability that defines labile BP. Understanding the nuance of labile htn is essential for tailoring treatment plans and avoiding the potential pitfalls of over- or under-treatment.
Physiological and Psychological Triggers Behind Labile BP
The underlying causes of labile blood pressure are multifaceted, involving both physiological and psychological dimensions. Stress remains one of the most consistent triggers. When an individual encounters a stressful situation, the body’s sympathetic nervous system activates, releasing catecholamines such as adrenaline and noradrenaline. These chemicals elevate heart rate, constrict blood vessels, and ultimately raise blood pressure. In people with labile hypertension, this response is often exaggerated or dysregulated.
Sleep deprivation, caffeine intake, and alcohol consumption can also play a role in blood pressure variability. For individuals sensitive to these factors, even moderate consumption can lead to significant spikes. Similarly, hormonal fluctuations—particularly in women during the menstrual cycle or menopause—have been linked to unstable blood pressure patterns. Physical conditions such as thyroid dysfunction or adrenal gland disorders can also precipitate labile BP, particularly when these conditions affect the production of hormones involved in blood pressure regulation.
Emotional sensitivity and personality traits may further contribute to reactive high blood pressure. People with anxiety disorders, panic disorders, or those who are particularly prone to rumination often experience exaggerated cardiovascular responses to stress. This connection between mental health and cardiovascular reactivity underlines the importance of a holistic approach to diagnosis and management. It also reinforces that labile blood pressure is not merely a behavioral issue but a legitimate physiological condition.
The Diagnostic Challenges of Labile Hypertension
Diagnosing labile hypertension requires a nuanced approach due to its transient and unpredictable nature. Standard blood pressure measurements taken in a clinical setting may not capture the full spectrum of variability experienced by the patient. As such, ambulatory blood pressure monitoring (ABPM) or home blood pressure tracking over several days or weeks is often recommended to detect patterns consistent with labile htn.
One challenge is differentiating labile hypertension from white coat hypertension. While both involve elevated readings in specific settings, labile BP tends to occur across various environments and situations, not just in medical settings. This distinction is important because treatment strategies differ depending on the root cause and the persistence of elevated readings. Misdiagnosing labile hypertension as sustained hypertension could result in unnecessary pharmacological interventions, while missing it entirely could delay needed treatment and lifestyle modifications.
Healthcare providers must also consider the patient’s psychological profile and stress levels when evaluating blood pressure variability. Questionnaires and assessments that screen for anxiety, depression, or emotional distress can offer valuable insights into potential triggers for reactive high blood pressure. Laboratory tests to rule out endocrine disorders or metabolic imbalances are equally important. Ultimately, a comprehensive, patient-centered approach to diagnosis helps avoid oversimplification and ensures that labile hypertension is properly understood and addressed.
How Labile Blood Pressure Affects Long-Term Cardiovascular Health
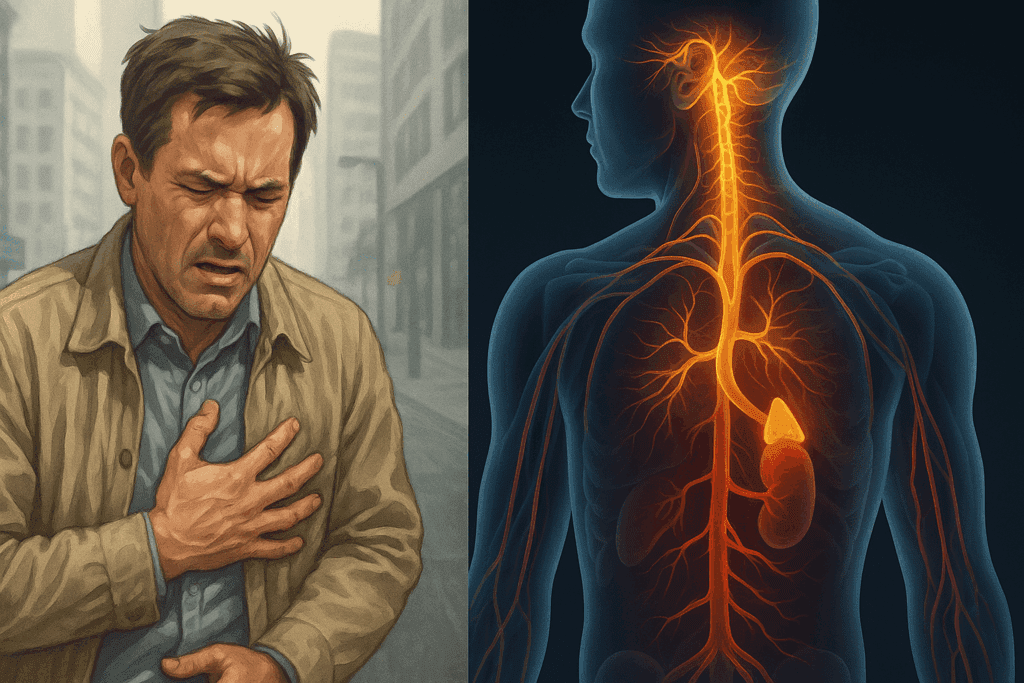
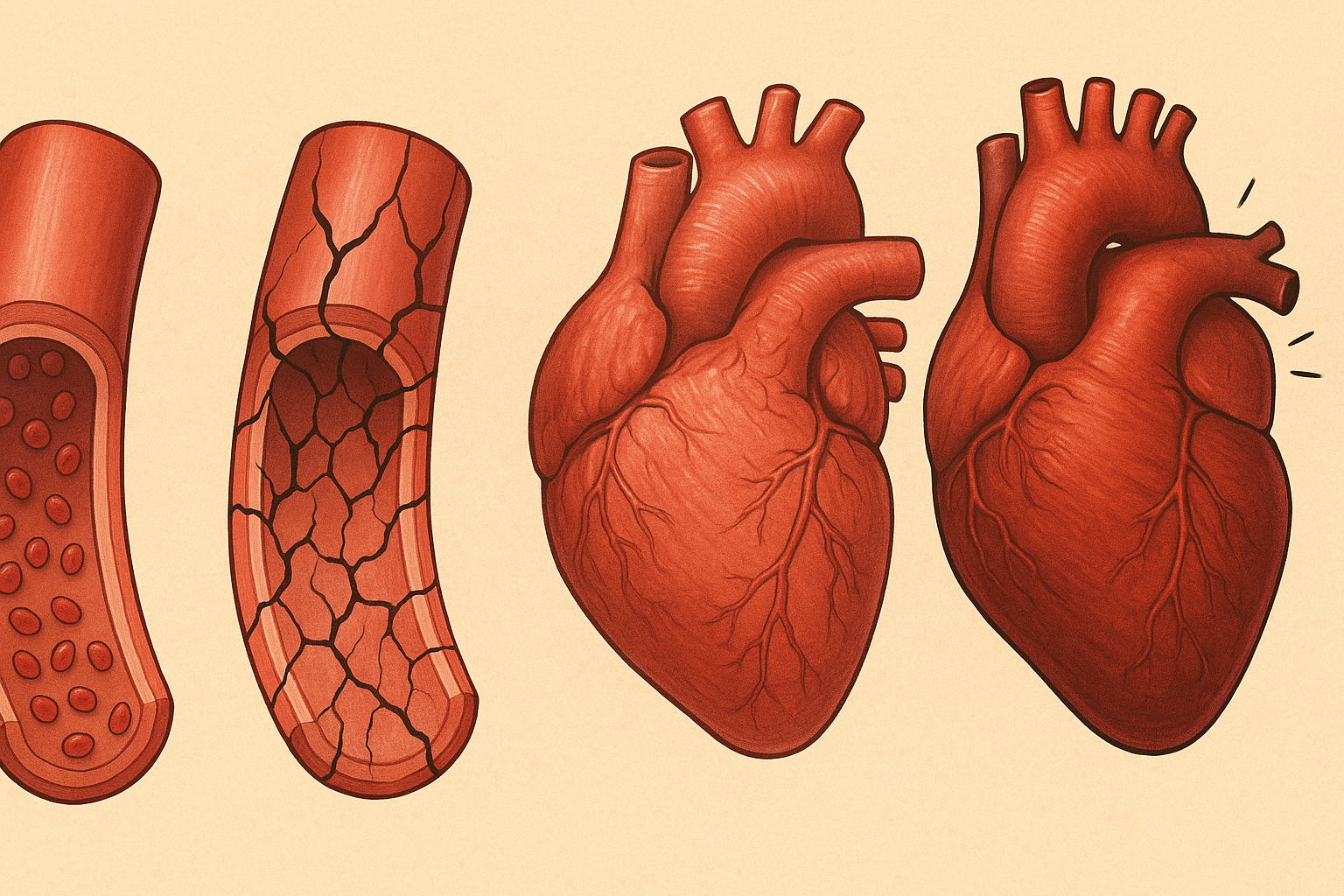
Although labile hypertension is often regarded as a temporary or benign condition, growing evidence suggests that it may have long-term implications for cardiovascular health. Repeated episodes of high blood pressure, even if short-lived, can exert cumulative stress on the blood vessels and the heart. Over time, this stress may lead to endothelial dysfunction, which impairs the ability of blood vessels to dilate properly and increases the risk of atherosclerosis.
The heart, too, is affected by repeated pressure spikes. Reactive high blood pressure can contribute to left ventricular hypertrophy, a condition in which the heart muscle thickens in response to increased workload. This structural change can decrease the heart’s efficiency and increase the risk of arrhythmias, heart failure, and ischemic events. Furthermore, the fluctuating nature of labile blood pressure may complicate the detection and management of sustained hypertension, leading to delayed intervention.
Another concern is the psychological toll of unpredictable blood pressure swings. Patients with labile hypertension often report heightened anxiety about their cardiovascular status, which in turn can trigger further episodes. This creates a feedback loop that exacerbates both psychological and physiological symptoms. The interplay between mind and body in labile BP underscores the importance of integrated care strategies that address both mental health and physical health in tandem.
Lifestyle Modifications for Managing Labile Hypertension
Managing labile hypertension effectively often begins with lifestyle modifications tailored to the individual’s specific triggers and health profile. Stress reduction is paramount. Techniques such as mindfulness meditation, progressive muscle relaxation, yoga, and biofeedback have been shown to lower reactivity to stress and stabilize blood pressure over time. These interventions not only reduce the frequency of blood pressure spikes but also enhance overall well-being and resilience.
Dietary choices also play a critical role in blood pressure regulation. A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats—such as the DASH (Dietary Approaches to Stop Hypertension) diet—can provide essential nutrients like potassium, magnesium, and calcium, which help modulate vascular tone. Limiting sodium intake is particularly important, as excessive salt can increase fluid retention and exacerbate blood pressure variability. Hydration, too, should not be overlooked, as dehydration can cause transient increases in blood pressure.
Regular physical activity is another cornerstone of labile hypertension management. Aerobic exercise, such as walking, swimming, or cycling, helps improve cardiovascular fitness, reduce stress, and support autonomic balance. However, individuals with labile BP should approach exercise cautiously, avoiding high-intensity workouts that may provoke exaggerated blood pressure responses. Working with a qualified health professional can ensure that physical activity is both safe and effective.

Pharmacological Approaches and Individualized Treatment Plans
While lifestyle changes form the foundation of labile hypertension management, pharmacological interventions may be necessary in some cases. The decision to use medication depends on the frequency and severity of blood pressure spikes, the presence of comorbid conditions, and the patient’s overall cardiovascular risk. Importantly, the goal is not simply to lower blood pressure but to stabilize it, minimizing the oscillations that characterize labile htn.
Beta-blockers are often used to blunt the sympathetic nervous system’s response to stress, thereby reducing the likelihood of reactive high blood pressure episodes. In patients with coexisting anxiety or panic disorders, these medications may serve dual purposes. Calcium channel blockers and ACE inhibitors may also be employed, particularly if the patient exhibits signs of persistent hypertension in addition to labile episodes.
Given the unpredictable nature of labile blood pressure, treatment must be highly individualized. A one-size-fits-all approach is rarely effective. Some patients may benefit from as-needed medications that they take when they anticipate stressful situations, while others may require daily therapy. Frequent monitoring, open communication with healthcare providers, and regular adjustments to the treatment plan are key to achieving optimal outcomes.
The Role of Emotional Regulation and Psychological Support
Emotional well-being plays a central role in managing labile blood pressure. Because reactive high blood pressure often stems from or is exacerbated by psychological triggers, addressing emotional health is not a peripheral concern—it is a central therapeutic target. Psychological interventions such as cognitive-behavioral therapy (CBT) have been shown to reduce the frequency and intensity of stress responses that contribute to blood pressure spikes.
Mindfulness-based stress reduction (MBSR) programs, which combine meditation, body awareness, and gentle movement, can help individuals develop a greater sense of control over their internal states. These techniques reduce sympathetic arousal and enhance parasympathetic activity, supporting a more balanced autonomic nervous system response. Over time, these practices can reduce the likelihood of labile BP episodes and improve quality of life.
Support groups, counseling, and psychoeducation can also provide valuable tools for individuals coping with labile hypertension. Understanding the condition, learning to recognize triggers, and developing proactive coping strategies can foster a sense of empowerment. For many, the reassurance of knowing that labile BP is a recognized and manageable condition can be transformative.
Understanding the Question: What Does High Return Pressure Mean?
The term “high return pressure” occasionally surfaces in discussions related to cardiovascular physiology, often leading to confusion. In clinical terms, this phrase is not commonly used in contemporary medical literature, and it may be a misinterpretation or simplification of concepts such as venous return pressure, central venous pressure (CVP), or afterload. Understanding what high return pressure means requires delving into these related concepts to clarify their relevance to cardiovascular function.
Central venous pressure reflects the amount of blood returning to the heart and the heart’s ability to pump that blood into the pulmonary circulation. Elevated CVP can indicate fluid overload, heart failure, or impaired venous return, and it may contribute to labile hypertension in certain contexts. If the heart is struggling to manage the returning volume, transient spikes in pressure may occur. In such cases, high return pressure is essentially a reflection of upstream resistance or cardiac inefficiency.
Clarifying this term is important because misinterpretation can lead to misunderstanding a patient’s condition or the mechanisms behind fluctuating blood pressure. For patients with labile BP, discussions about venous return, preload, and sympathetic tone are more clinically appropriate. Healthcare providers should ensure that terminology is both accurate and accessible to promote better patient understanding and care adherence.
Frequently Asked Questions (FAQ) About Labile Hypertension and Reactive High Blood Pressure
1. Can labile hypertension increase the risk of cognitive decline or neurological disorders?
Yes, emerging research suggests that labile hypertension may contribute to an elevated risk of cognitive impairment, particularly in older adults. The brain’s blood vessels are highly sensitive to rapid changes in pressure, and frequent episodes of labile blood pressure may lead to microvascular damage over time. This can compromise cerebral perfusion, potentially accelerating conditions such as vascular dementia or mild cognitive impairment. Reactive high blood pressure episodes also tend to coincide with stress, which activates inflammatory pathways that may further influence brain health. While the relationship is still under investigation, maintaining stable blood pressure levels appears essential for long-term cognitive resilience.
2. How does labile BP affect individuals during physical exertion or exercise?
People with labile BP often report exaggerated blood pressure responses to even moderate physical activity, especially when they are unconditioned or emotionally tense. This reactivity can create a barrier to exercise adherence, as individuals may become fearful of triggering hypertensive spikes. However, research indicates that tailored aerobic exercise programs, introduced gradually, can actually improve autonomic regulation in those with labile hypertension. Over time, consistent movement helps the cardiovascular system adapt more efficiently to physical stressors, reducing the severity and frequency of reactive high blood pressure episodes. It’s essential to consult with a healthcare provider to create a personalized fitness plan that balances safety with therapeutic benefit.
3. Are there any gender-specific patterns associated with labile htn?
Yes, gender differences have been observed in the presentation and progression of labile htn. Women, particularly during hormonal transitions such as menopause, may experience more pronounced fluctuations in blood pressure due to shifts in estrogen levels. This can heighten their sensitivity to emotional triggers, making reactive high blood pressure more prevalent in female patients. Men, on the other hand, often show a stronger association between labile hypertension and lifestyle-related factors like alcohol use and high-stress occupations. Understanding these gender-based nuances allows for more individualized treatment strategies and underscores the importance of a biopsychosocial approach to cardiovascular care.
4. What role does sleep quality play in labile blood pressure management?
Sleep quality is a critical yet often overlooked component in the management of labile blood pressure. Individuals with labile hypertension frequently report poor sleep, interrupted by anxiety, nightmares, or sleep apnea—all of which can drive up nighttime blood pressure. The autonomic nervous system requires restorative sleep to maintain balance, and its dysregulation can lead to increased sympathetic activity, a hallmark of reactive high blood pressure. Establishing consistent sleep hygiene routines and addressing underlying sleep disorders can dramatically reduce the occurrence of labile BP spikes. Some clinicians may recommend sleep studies for patients who exhibit labile htn along with signs of chronic fatigue or excessive daytime sleepiness.
5. Can labile hypertension be a precursor to more persistent forms of high blood pressure?
Yes, for some individuals, labile hypertension serves as an early warning sign of future sustained hypertension. Over time, repeated blood pressure spikes may induce vascular remodeling and endothelial damage, setting the stage for chronic elevation in resting blood pressure. Monitoring labile BP closely allows for early intervention through lifestyle changes or targeted pharmacotherapy to potentially delay or prevent the transition to chronic hypertension. This is particularly important in younger adults, where early-stage labile htn might otherwise be dismissed as stress-related without a deeper investigation. Recognizing this progression pathway can help reduce long-term cardiovascular risk.
6. How does emotional intelligence influence the frequency of reactive high blood pressure episodes?
Emotional intelligence (EI)—the ability to identify, understand, and regulate one’s emotions—has a strong correlation with blood pressure stability. Individuals with higher EI are better equipped to manage psychological stressors that can otherwise trigger reactive high blood pressure. Practicing emotional regulation techniques, such as mindfulness-based emotional awareness, can buffer the impact of external stress on labile BP. On the contrary, those with lower EI may exhibit more frequent hypertensive episodes, especially in socially demanding or conflict-prone environments. Integrating emotional intelligence training into cardiovascular care may offer a novel, non-pharmacologic approach to managing labile hypertension.
7. Is there a connection between gut health and labile BP regulation?
Recent studies suggest that the gut-brain-heart axis plays a meaningful role in blood pressure variability, including labile BP. Imbalances in the gut microbiome can influence systemic inflammation, hormone regulation, and even neurotransmitter production—all of which affect cardiovascular reactivity. In cases of labile hypertension, individuals may benefit from gut-supportive interventions such as probiotics, high-fiber diets, and prebiotic-rich foods. These dietary choices help stabilize not just digestion, but also stress response and blood pressure control. Although this field is still evolving, the interplay between gut health and reactive high blood pressure represents a promising area of future research.
8. How does chronic pain interact with labile hypertension?
Chronic pain and labile hypertension often coexist, and their relationship is mediated by shared physiological pathways involving the autonomic nervous system. Persistent pain activates sympathetic responses that can contribute to reactive high blood pressure episodes, especially in those with heightened pain sensitivity. Moreover, medications used to treat chronic pain—such as NSAIDs or certain antidepressants—may influence blood pressure stability. Patients with both conditions may require interdisciplinary care involving pain specialists, cardiologists, and behavioral health providers. Addressing chronic pain may be a critical yet underappreciated step in the long-term management of labile htn.
9. What does high return pressure mean in the context of labile hypertension?
While the term is not commonly used in standard cardiology texts, high return pressure may refer to elevated central venous pressure or increased preload in the heart. In patients with labile blood pressure, this can suggest impaired cardiac compliance or inefficient venous return, potentially exacerbating hypertensive variability. If venous return exceeds the heart’s ability to pump effectively, pressure builds in the system, influencing both systolic and diastolic values. Understanding what high return pressure means in this context requires evaluating cardiac output, fluid status, and autonomic regulation. Diagnostic tools such as echocardiography or CVP monitoring may help clarify its relevance in patients with reactive high blood pressure.
10. Are there occupational risks associated with labile BP?
Certain professions inherently elevate the risk for labile BP due to their psychological and physiological demands. High-stress roles—such as those in emergency medicine, law enforcement, finance, or caregiving—are often associated with increased episodes of reactive high blood pressure. The constant emotional arousal and cognitive load in these jobs may contribute to autonomic dysregulation, a key feature of labile hypertension. Implementing workplace wellness programs, stress management interventions, and supportive organizational cultures can help mitigate these risks. For individuals in these professions, regular blood pressure monitoring and early lifestyle modifications can serve as vital preventive measures against long-term cardiovascular consequences.
Bringing It All Together: Why Recognizing and Managing Labile Hypertension Matters
Labile hypertension, once considered a minor variation of normal blood pressure responses, is increasingly recognized as a meaningful clinical condition with important implications for cardiovascular health. While it may not meet the criteria for sustained hypertension, its episodic spikes—especially when triggered by emotional or physiological stressors—can lead to cumulative damage and increased cardiovascular risk over time. The fluctuating nature of labile blood pressure makes it challenging to diagnose and manage, but not impossible. With the right tools, monitoring strategies, and individualized treatment plans, patients can gain control over their condition and improve long-term outcomes.
Importantly, the term reactive high blood pressure helps frame the condition in a way that underscores the body’s heightened responsiveness to external stimuli. It is this reactivity that makes labile htn distinct from other forms of hypertension and requires a multifaceted approach that includes emotional regulation, lifestyle interventions, and, when necessary, pharmacological support. Understanding what does high return pressure mean in this context also enriches the conversation, helping clinicians and patients alike navigate the complex physiology of cardiovascular function.
For healthcare professionals, recognizing labile blood pressure as a legitimate cardiovascular concern necessitates ongoing education, compassionate patient engagement, and comprehensive evaluation strategies. For patients, the journey involves building awareness, adopting healthy coping mechanisms, and developing trust in a collaborative healthcare plan. Together, these efforts ensure that labile hypertension is no longer overlooked but addressed with the care, nuance, and precision it deserves.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.