Pregnancy is a time of great physiological change, and while many of these changes are normal and expected, others may pose risks to both the mother and fetus. Among the most concerning of these complications is pregnancy-induced hypertension, commonly abbreviated as PIH. Understanding what is PIH pregnancy induced hypertension is essential not only for expectant mothers but also for clinicians, caregivers, and policymakers focused on maternal and fetal health. With cardiovascular disorders being a leading cause of maternal morbidity and mortality, gaining awareness of the signs, implications, and management strategies for PIH is of paramount importance.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention

Defining PIH and How It Differs from Chronic Hypertension
Pregnancy-induced hypertension refers to the development of high blood pressure during pregnancy in a woman who previously had normal blood pressure levels. PIH typically arises after the 20th week of gestation and is distinct from chronic hypertension, which is present before pregnancy or appears before the 20-week mark. In many cases, PIH resolves postpartum, but it may also progress into more severe hypertensive disorders such as preeclampsia or eclampsia if left unmanaged.
The defining characteristic of PIH pregnancy is an elevation in blood pressure exceeding 140/90 mm Hg on two separate readings taken at least four hours apart. Notably, this increase is not accompanied by significant proteinuria or signs of organ damage in its earliest stages, which differentiates it from preeclampsia. However, distinguishing between these conditions can sometimes be complex, especially if a woman has overlapping risk factors or if diagnostic resources are limited. It is essential to recognize that PIH is not merely a variation of normal pregnancy physiology; it is a medical condition that warrants careful monitoring.

Risk Factors and Epidemiological Insights
The risk of developing PIH pregnancy is influenced by a variety of genetic, lifestyle, and demographic factors. First-time pregnancies, or primigravida status, significantly elevate the likelihood of PIH. Women under the age of 20 or over the age of 35 also face higher risks. Other contributing factors include obesity, a personal or family history of hypertension, multiple gestations such as twins or triplets, and underlying conditions like diabetes or autoimmune disorders.
Racial and ethnic disparities are also evident in the prevalence of PIH. Studies have shown that African American women are at a disproportionately higher risk, which may be attributed to a combination of socioeconomic factors, access to healthcare, and genetic predispositions. Understanding these patterns can help healthcare providers better allocate resources and tailor prenatal care to populations most in need.
It is also important to note that the incidence of PIH has increased in recent years, partly due to rising obesity rates and older maternal age at conception. As such, public health initiatives that promote healthy preconception and prenatal habits may play a critical role in reducing the incidence and severity of pregnancy-induced hypertension.
Pathophysiological Mechanisms Behind PIH
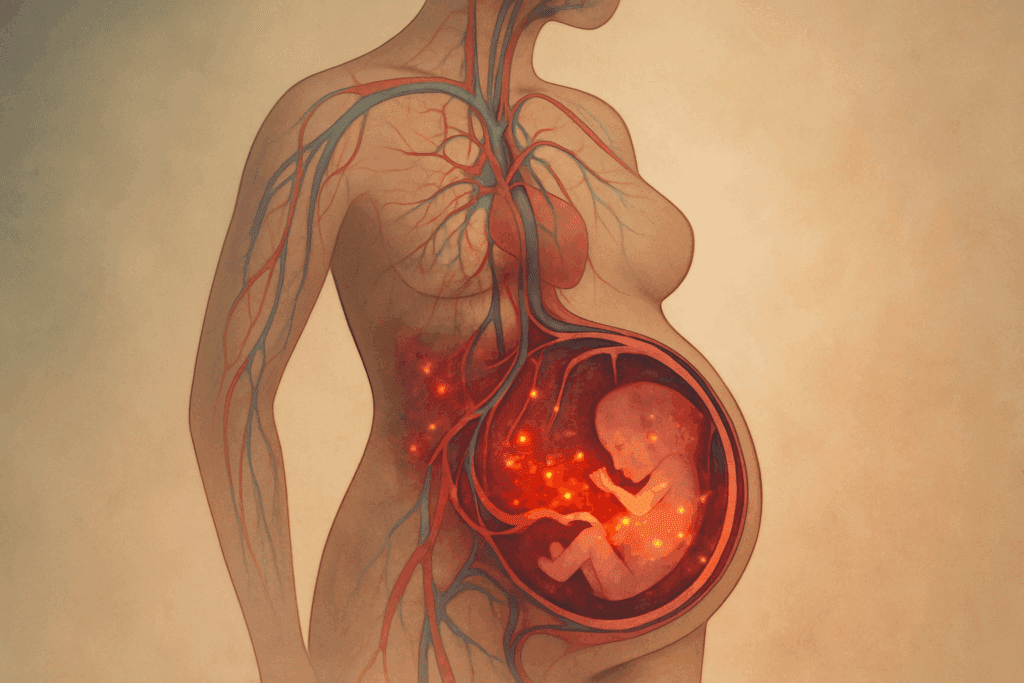
The pathophysiology of PIH is complex and not yet fully understood, but several theories offer insights into its development. One prominent hypothesis involves abnormal placentation, which leads to poor perfusion and oxygenation of the placenta. This, in turn, triggers the release of inflammatory mediators and antiangiogenic factors into the maternal bloodstream, resulting in systemic endothelial dysfunction.
This endothelial dysfunction is central to the vascular changes seen in PIH pregnancy. It contributes to increased vascular resistance and elevated blood pressure. Additionally, an imbalance in prostacyclin and thromboxane—two hormones that regulate vasodilation and platelet aggregation—further exacerbates the hypertensive state. Genetic and immunologic factors are also thought to play roles, as maternal immune maladaptation to paternal antigens in the placenta may contribute to inflammation and vascular irregularities.
Emerging research is beginning to explore the role of oxidative stress and the renin-angiotensin system in PIH development. These findings not only deepen our understanding of the condition but also open avenues for targeted therapeutic interventions. Recognizing that PIH is not a random event but a multifactorial process grounded in identifiable biological pathways enhances our ability to diagnose and treat it more effectively.
Recognizing the Signs and Symptoms
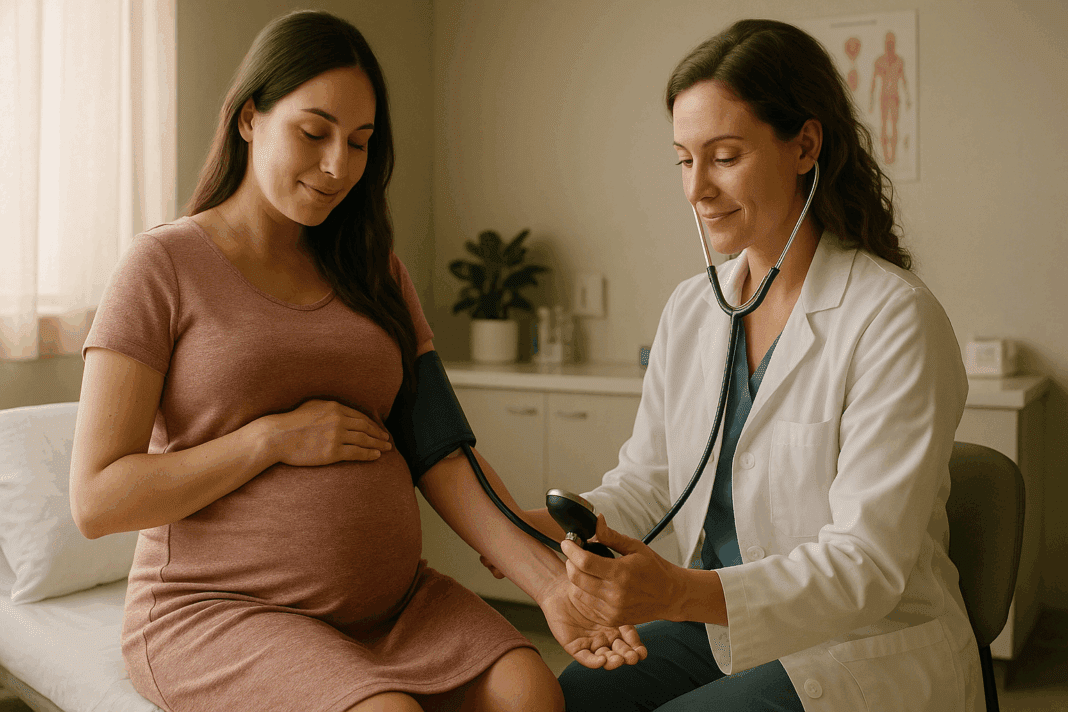
Early detection of PIH is crucial in preventing its progression to more severe hypertensive disorders. However, one of the challenges with managing what is PIH pregnancy induced hypertension lies in its frequently subtle onset. In many cases, women may not exhibit noticeable symptoms in the early stages, making routine prenatal blood pressure checks essential.
When symptoms do appear, they may include headaches, visual disturbances such as blurred vision or seeing spots, swelling in the hands and face, and sudden weight gain. These manifestations are often the result of increased vascular permeability and fluid retention. In more advanced stages or in the transition to preeclampsia, symptoms may also involve right upper quadrant abdominal pain, nausea, vomiting, and decreased urine output, indicating potential liver or kidney involvement.
Because these symptoms can be mistaken for normal pregnancy discomforts, both patients and healthcare providers must remain vigilant. Educating expectant mothers about the warning signs of PIH and encouraging open communication during prenatal visits can significantly improve outcomes. In cases where symptoms are present, prompt diagnostic testing and close monitoring are essential.
Diagnostic Criteria and Clinical Evaluation
The diagnosis of PIH is primarily based on blood pressure measurements and the exclusion of other hypertensive disorders. According to guidelines from the American College of Obstetricians and Gynecologists (ACOG), a diagnosis is made when systolic blood pressure reaches or exceeds 140 mm Hg or diastolic pressure exceeds 90 mm Hg on two occasions at least four hours apart, after 20 weeks of gestation.
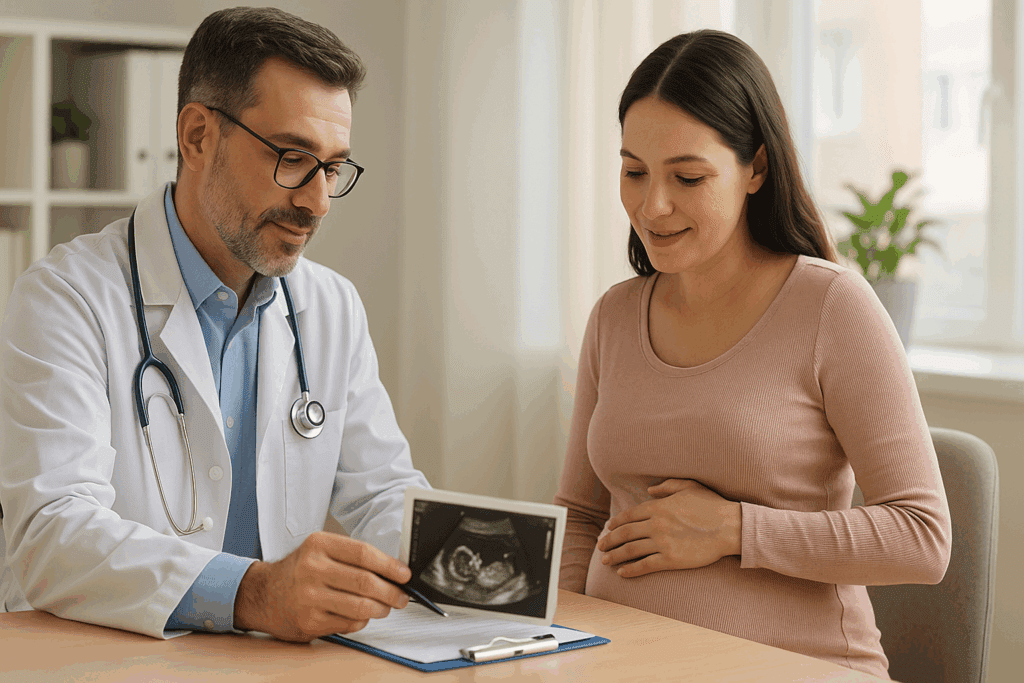
In the absence of proteinuria or organ dysfunction, these readings are indicative of gestational hypertension or PIH. However, clinicians must also evaluate for evolving signs that may suggest progression to preeclampsia. These may include abnormalities in liver enzymes, renal function tests, and platelet counts. Fetal monitoring via ultrasound and non-stress tests may also be warranted to assess intrauterine growth and amniotic fluid levels, as PIH can affect placental function.
It’s worth emphasizing that PIH is a diagnosis of exclusion, meaning other potential causes of elevated blood pressure must be ruled out. This includes chronic hypertension, white coat hypertension, and transient blood pressure elevations due to stress or activity. As such, a comprehensive clinical evaluation that includes patient history, laboratory tests, and fetal assessment is crucial.

Potential Complications for Mother and Baby
When left untreated, PIH can lead to serious health complications for both the mother and the developing fetus. For mothers, the most concerning risks include the development of preeclampsia, eclampsia (seizures), placental abruption, and HELLP syndrome (Hemolysis, Elevated Liver enzymes, and Low Platelet count). These conditions can result in significant morbidity and even mortality if not promptly addressed.
From a cardiovascular perspective, PIH pregnancy significantly increases the maternal risk of long-term hypertension and cardiovascular disease later in life. Women with a history of PIH are more likely to develop chronic hypertension, stroke, and heart disease, highlighting the importance of long-term follow-up and lifestyle modification after delivery.
Fetal complications are equally serious and may include intrauterine growth restriction (IUGR), preterm birth, low birth weight, and in severe cases, stillbirth. These outcomes are largely attributed to impaired placental blood flow, which compromises the delivery of oxygen and nutrients to the fetus. In some cases, early delivery may be the only viable option to protect the health of both mother and baby, underscoring the delicate balance clinicians must navigate.
Management and Treatment Strategies
The management of PIH pregnancy hinges on the severity of the condition and the gestational age at diagnosis. In mild cases, expectant management with close monitoring of maternal blood pressure and fetal well-being may be appropriate. This often includes more frequent prenatal visits, blood pressure checks, urine testing, and ultrasounds to assess fetal growth.
Lifestyle modifications such as reducing sodium intake, increasing rest, and staying well-hydrated can also help manage mild hypertension during pregnancy. However, in more severe cases, pharmacological intervention may be necessary. Medications like labetalol, nifedipine, and methyldopa are commonly used due to their established safety profiles during pregnancy.
Hospitalization may be required in situations where blood pressure is dangerously elevated, or when signs of preeclampsia emerge. In such cases, corticosteroids may be administered to accelerate fetal lung maturity if early delivery is anticipated. Ultimately, delivery is the only definitive cure for PIH, and timing the delivery to maximize outcomes for both mother and baby is a critical aspect of management.
Postpartum Considerations and Long-Term Health
Although PIH typically resolves within 12 weeks after delivery, postpartum monitoring remains essential. Some women may continue to experience elevated blood pressure or may go on to develop chronic hypertension. This transition is not always immediately apparent, which makes postpartum follow-up care just as important as prenatal management.
Additionally, women who have experienced PIH pregnancy are at a heightened risk for cardiovascular disorders later in life. Studies have linked a history of PIH to increased rates of heart failure, stroke, and metabolic syndrome. For this reason, postpartum care should include counseling on cardiovascular risk reduction through diet, exercise, and regular health screenings.
Breastfeeding is generally encouraged, as it provides health benefits for both mother and baby and may contribute to improved metabolic profiles postpartum. Emotional and psychological support is also vital, as the stress of a complicated pregnancy can have lasting mental health impacts. Providers should remain attentive to signs of postpartum depression or anxiety, which may be exacerbated by the experience of PIH.
The Importance of Preventive Care and Public Health Initiatives
Preventing PIH requires a multifaceted approach that begins even before conception. Preconception counseling can identify modifiable risk factors such as obesity, poorly controlled diabetes, or unmanaged hypertension. Weight management, smoking cessation, and regular exercise are all strategies that can reduce the risk of developing PIH during pregnancy.
Healthcare access plays a critical role in the prevention and early detection of PIH. Expanding access to prenatal care, especially in underserved communities, ensures that potential warning signs are caught early and managed appropriately. Telehealth and mobile health clinics may offer innovative solutions for reaching women who face barriers to traditional care.
Public health campaigns that raise awareness about what is PIH pregnancy induced hypertension can empower women to take an active role in their health. Educational programs aimed at both healthcare providers and patients can foster a collaborative approach to prenatal care, where early warning signs are not only recognized but acted upon swiftly. Addressing social determinants of health such as housing, nutrition, and transportation also plays a role in reducing PIH-related disparities.
Emerging Research and Future Directions
Scientific research continues to expand our understanding of the mechanisms and long-term effects of PIH. Genetic studies are exploring specific gene variants that may predispose certain women to hypertension during pregnancy. These insights could eventually pave the way for personalized medicine approaches, where risk assessments and preventive strategies are tailored to individual genetic profiles.
Biomarker research is also making strides. Identifying specific proteins or hormonal patterns that predict PIH before clinical symptoms emerge could revolutionize early detection and intervention. Additionally, studies are evaluating the potential of novel antihypertensive therapies that target the underlying pathophysiology rather than simply managing symptoms.
As the body of knowledge grows, there is increasing recognition of the importance of including diverse populations in research. Ensuring that findings are generalizable across racial, ethnic, and socioeconomic groups is vital for equitable healthcare delivery. Collaboration between obstetricians, cardiologists, and public health experts will be key to translating research into practice.
Frequently Asked Questions (FAQ) About PIH Pregnancy
1. Can stress or anxiety during pregnancy increase the risk of PIH?
While stress and anxiety are not direct causes of PIH pregnancy, they can exacerbate physiological responses that contribute to elevated blood pressure. Chronic stress activates the body’s sympathetic nervous system and can lead to increased levels of cortisol and adrenaline, which may influence vascular tone and cardiac output. This heightened state of physiological arousal may, in turn, make it more difficult to control blood pressure, particularly in women who are already at risk for what is PIH pregnancy induced hypertension. Moreover, anxiety can affect sleep quality and dietary habits—two factors that indirectly influence cardiovascular health during pregnancy. Therefore, implementing stress-reduction strategies such as prenatal yoga, mindfulness meditation, and regular mental health check-ins can serve as supportive measures in PIH management.
2. How does PIH affect postpartum recovery and future pregnancies?
Experiencing PIH pregnancy can significantly alter a woman’s postpartum recovery trajectory. Not only may blood pressure remain elevated for weeks after delivery, but women with a history of PIH are also at an increased risk for cardiovascular complications later in life. Additionally, what is PIH pregnancy induced hypertension often recurs in subsequent pregnancies, with the likelihood increasing if the condition was severe or appeared early. This necessitates proactive preconception counseling and cardiovascular screening in women planning future pregnancies. Lifestyle interventions—such as weight management, physical activity, and blood pressure monitoring—can improve maternal outcomes in later pregnancies and mitigate long-term risks.
3. Are there nutritional interventions that may help prevent PIH?
Although no diet can guarantee prevention of PIH pregnancy, emerging research highlights the potential of specific nutritional strategies in reducing risk. Diets rich in potassium, calcium, and magnesium—such as the DASH diet—have been shown to support healthy blood pressure levels during pregnancy. Antioxidant-rich foods, including berries and leafy greens, may counteract oxidative stress, a known contributor to vascular dysfunction in what is PIH pregnancy induced hypertension. Omega-3 fatty acids found in flaxseed, walnuts, and fatty fish may also improve endothelial function and reduce systemic inflammation. Importantly, reducing sodium intake and avoiding ultra-processed foods are foundational to any nutritional strategy targeting blood pressure regulation.
4. Can wearable health technologies assist in managing PIH at home?
Wearable health technologies have emerged as valuable tools in managing chronic conditions, and their role in monitoring PIH pregnancy is growing. Devices such as smartwatches and connected blood pressure monitors allow expectant mothers to track their vitals in real time, providing actionable insights between prenatal visits. For individuals experiencing what is PIH pregnancy induced hypertension, these tools can detect fluctuations early and prompt timely medical intervention. Some devices even include features such as guided breathing exercises and stress tracking, which can help lower sympathetic nervous system activity. However, users should be cautious not to rely solely on these technologies; regular clinical evaluations remain essential.
5. What are the psychological effects of experiencing PIH during pregnancy?
The psychological toll of PIH pregnancy can be substantial, particularly when it leads to hospitalization, bed rest, or early delivery. Women may experience heightened levels of anxiety, depression, or feelings of failure due to complications that disrupt their expectations for a healthy pregnancy. Moreover, what is PIH pregnancy induced hypertension often introduces uncertainty about both maternal and fetal health, compounding emotional stress. Support groups, counseling services, and patient education programs tailored to hypertensive disorders of pregnancy can play a crucial role in emotional recovery. Encouraging open dialogue between patients and providers about mental health is an essential aspect of holistic care.
6. How is PIH different from white coat hypertension during pregnancy?
Distinguishing PIH pregnancy from white coat hypertension—a condition where blood pressure rises in clinical settings due to anxiety—is critical for proper diagnosis and treatment. While both conditions involve elevated readings, white coat hypertension typically resolves outside the medical environment and does not carry the same risks as what is PIH pregnancy induced hypertension. Ambulatory blood pressure monitoring over a 24-hour period can help differentiate between the two. Persistent elevation at home as well as in clinical settings usually indicates true gestational hypertension. Accurate diagnosis ensures that resources and interventions are appropriately directed, preventing over-treatment or underestimation of cardiovascular risk.
7. Can exercise be safely incorporated into the routine of someone diagnosed with PIH?
Exercise can be beneficial for women with PIH pregnancy, provided it is tailored to their individual health status and approved by their healthcare provider. Low-impact activities such as walking, prenatal yoga, and aquatic exercises may help reduce blood pressure, improve circulation, and enhance overall well-being. Importantly, physical activity can also serve as a stress-relieving outlet, which indirectly supports cardiovascular health in cases of what is PIH pregnancy induced hypertension. However, high-intensity workouts or exercises that pose a fall risk should be avoided, particularly in women with additional complications such as preeclampsia. Regular communication with a care team ensures that exercise is both safe and effective.
8. Are there long-term cardiovascular risks associated with PIH beyond the postpartum period?
Yes, PIH pregnancy has been linked to a heightened risk of cardiovascular disease well beyond the childbearing years. Research indicates that women who experience what is PIH pregnancy induced hypertension are more likely to develop chronic hypertension, heart failure, and stroke later in life. These risks persist even in women whose blood pressure normalizes after delivery. The underlying vascular changes, such as endothelial dysfunction and arterial stiffness, may have lasting effects. For this reason, long-term follow-up care that includes regular cardiovascular screening, lipid panels, and lifestyle counseling is essential for women with a history of PIH.
9. How does PIH influence decisions around delivery timing and method?
PIH pregnancy often complicates the decision-making process around labor and delivery, especially when blood pressure control becomes difficult. In cases where what is PIH pregnancy induced hypertension is mild and the pregnancy is nearing full term, vaginal delivery may still be a viable option. However, if PIH worsens or shows signs of progression toward preeclampsia, early induction or cesarean delivery may be recommended to protect maternal and fetal health. Fetal growth restriction, abnormal Doppler findings, and deteriorating maternal labs are among the indicators that influence timing decisions. The ultimate goal is to balance the risks of prematurity with those posed by continued intrauterine exposure to hypertensive conditions.
10. What innovations are on the horizon for PIH prediction and prevention?
The future of PIH pregnancy care is poised to benefit from significant technological and clinical advancements. Researchers are exploring biomarkers such as placental growth factor (PlGF) and soluble fms-like tyrosine kinase-1 (sFlt-1) as early indicators of what is PIH pregnancy induced hypertension, potentially allowing for earlier diagnosis and targeted interventions. Artificial intelligence models are also being developed to analyze patient data and predict risk profiles with high accuracy. On the prevention front, clinical trials are evaluating the efficacy of low-dose aspirin and novel antihypertensive therapies that are specifically designed for pregnancy. As our understanding of PIH evolves, these innovations hold promise for more personalized and effective maternal care.
Why Understanding PIH Pregnancy Is Essential for Long-Term Cardiovascular and Maternal Health
Awareness and understanding of what is PIH pregnancy induced hypertension have never been more important. This condition is not just a temporary complication confined to the months of gestation—it carries significant implications for lifelong cardiovascular health. Timely diagnosis, comprehensive management, and robust postpartum care are essential to mitigating both immediate and long-term risks.
By fostering a deeper understanding of PIH among clinicians, patients, and public health professionals, we can move toward a healthcare model that emphasizes prevention, early intervention, and sustained wellness. Continued investment in research, education, and equitable healthcare access will be vital in reducing the burden of PIH and its associated complications. Ultimately, protecting maternal health during pregnancy protects cardiovascular health for a lifetime, making the recognition and management of PIH a critical public health priority.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
What is pregnancy-induced hypertension (PIH)?
Hypertensive Disorders of Pregnancy
Pregnancy-Induced Hypertension: Its Impact on Maternal and Fetal Health