High blood pressure, or hypertension, is one of the most prevalent cardiovascular disorders worldwide, contributing significantly to the risk of heart attack, stroke, and kidney disease. While lifestyle factors like diet, exercise, and stress management are well-known influences on blood pressure, what is less often discussed—but equally important—is the role that medications can play in elevating blood pressure. For many individuals, this connection between medication and blood pressure is hidden in plain sight, quietly influencing health outcomes and often going unrecognized. Understanding whether a medication can cause high blood pressure or raise existing levels is essential for both patients and healthcare professionals aiming to maintain optimal cardiovascular health.
The question “Can medication cause high blood pressure?” is not hypothetical—it is grounded in scientific evidence and clinical practice. Numerous commonly prescribed and over-the-counter drugs can, in fact, lead to elevated blood pressure levels. These medications range from anti-inflammatory agents to antidepressants, decongestants, hormonal treatments, and even certain types of birth control. By exploring the mechanisms behind these effects and identifying which drugs pose a risk, this article aims to offer clarity and actionable guidance. When managed with awareness and care, these risks can often be mitigated or avoided entirely, helping patients maintain control over their blood pressure and overall health.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Understanding How Medications Influence Blood Pressure
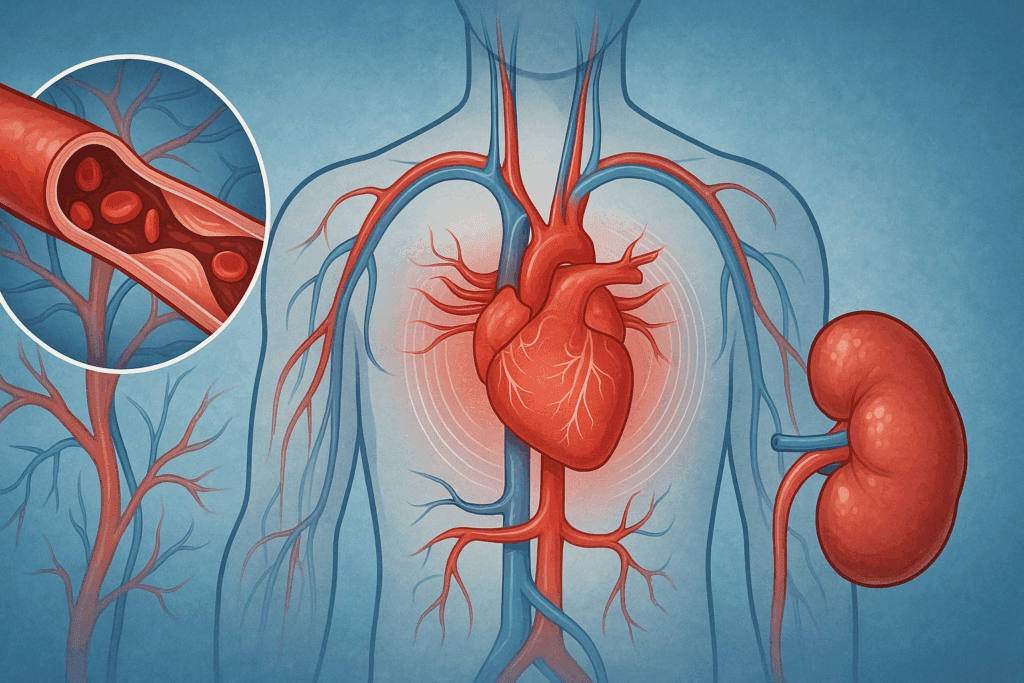
The human body maintains blood pressure through a complex interaction of the heart, blood vessels, kidneys, nervous system, and hormonal signaling. When medications interact with one or more of these systems, they can inadvertently raise blood pressure. Some drugs cause the blood vessels to constrict, increasing vascular resistance and thus pressure. Others promote fluid retention, which raises the volume of blood circulating in the body. Additionally, certain medications may affect the central nervous system, leading to increased sympathetic activity that accelerates the heart rate and tightens blood vessels.
For example, nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen are known to cause sodium and water retention, while also reducing kidney function and altering prostaglandin synthesis. These combined effects can result in significant elevations in blood pressure, especially in people already diagnosed with hypertension. Recognizing these physiological pathways is crucial in understanding how a seemingly benign over-the-counter medicine to increase blood pressure unintentionally may disrupt a patient’s treatment plan for hypertension.

Which Medications Commonly Raise Blood Pressure?
A wide array of medications has been implicated in raising blood pressure. Among the most well-known are NSAIDs such as ibuprofen (brand name Advil) and naproxen (brand name Aleve). Studies have shown that these drugs can interfere with the efficacy of high blood pressure medications and may independently elevate blood pressure in susceptible individuals. The question “does Aleve raise blood pressure?” has been answered affirmatively by numerous clinical trials. In fact, even short-term use of Aleve or Advil can raise BP, particularly when taken at higher doses or combined with other medications.
Other categories of drugs to raise blood pressure include certain antidepressants—especially serotonin-norepinephrine reuptake inhibitors (SNRIs) and monoamine oxidase inhibitors (MAOIs). These medications can influence blood pressure by altering neurotransmitter levels that regulate vascular tone. Decongestants containing pseudoephedrine or phenylephrine are also notorious for raising blood pressure, as they work by narrowing blood vessels to reduce nasal swelling but in doing so, increase systemic blood pressure. Even some herbal supplements and natural remedies have been shown to interfere with blood pressure control.
Hormonal treatments, including corticosteroids and some forms of birth control, can act as medication to raise BP through mechanisms such as fluid retention and increased vascular sensitivity to circulating hormones. These effects underscore the need to thoroughly evaluate all medications a patient is taking—including those not primarily intended to affect blood pressure—when managing hypertension.

Spotlight on NSAIDs: Does Aleve Raise Blood Pressure?
NSAIDs are among the most frequently used over-the-counter medications in the world, often taken without a second thought for pain relief, fever reduction, or inflammation. However, for individuals concerned about their cardiovascular health, it is essential to consider the potential impact of drugs like Aleve and Advil on blood pressure. The clinical evidence supporting the connection is robust. NSAIDs reduce the production of prostaglandins, which help maintain blood flow to the kidneys. When prostaglandin levels drop, the kidneys may retain more sodium and water, increasing blood volume and pressure.
So, can Aleve raise blood pressure? Yes, and the risk is especially notable in older adults, individuals with pre-existing hypertension, or those with compromised kidney function. Even if taken occasionally, the question “does Aleve elevate blood pressure?” becomes more than just a theoretical concern; it represents a tangible risk that should be carefully considered in the context of long-term blood pressure management.
Ibuprofen, another common NSAID, raises similar concerns. When patients ask, “does ibuprofen raise BP?” or “does Advil raise BP?”, clinicians must evaluate both the dosage and frequency of use. The more frequently these medications are used, the higher the likelihood that they will contribute to or exacerbate hypertension. This is why many healthcare providers advise patients with high blood pressure to avoid NSAIDs when possible and seek alternative pain management options.

The Impact of Decongestants and Cold Medications
Decongestants such as pseudoephedrine and phenylephrine are commonly found in over-the-counter cold and flu medications. While effective at relieving nasal congestion, these compounds act by constricting blood vessels in the nasal passages—a mechanism that unfortunately also affects blood vessels throughout the body. As a result, they represent a class of meds to raise blood pressure, particularly when taken over multiple days or in high doses.
For someone with borderline or diagnosed hypertension, these medications can tip the balance, leading to elevated blood pressure readings that may persist beyond the period of illness. The relationship between decongestants and blood pressure is well-documented in medical literature, and many healthcare professionals caution against their use in patients who are already on medication to control hypertension. In some cases, the disruption to HBP meds caused by adding a decongestant can result in an increase significant enough to warrant medical intervention.
This raises an important point for consumers: the inclusion of a decongestant in a combination product does not always receive the scrutiny it should. Many patients do not realize that the cold medicine they are taking contains a drug that can act as a medication to increase blood pressure. As a result, individuals must read labels carefully and consult with healthcare providers before using over-the-counter products, especially during cold and allergy seasons.
The Role of Antidepressants and Psychotropic Drugs
While the primary purpose of antidepressants is to regulate mood, some types of these drugs can have unintended cardiovascular side effects. SNRIs such as venlafaxine and desvenlafaxine are known to increase norepinephrine levels in the body, which can lead to vasoconstriction and higher blood pressure. Similarly, MAOIs can affect catecholamine levels and interfere with the body’s natural mechanisms for controlling vascular tone. These classes of medications can therefore function as drugs to increase blood pressure, especially when prescribed at higher doses.
The decision to prescribe antidepressants to a patient with existing hypertension must be made carefully, weighing the mental health benefits against the potential cardiovascular risks. Moreover, close monitoring is essential, as even a small change in dose can lead to significant fluctuations in blood pressure. Patients who are unaware of the potential side effects may not connect new symptoms—such as headaches, dizziness, or palpitations—with the introduction of a new antidepressant. Education and proactive communication between patients and providers are essential in managing these risks.
Another concern arises when patients stop or change medications abruptly. A sudden withdrawal or switch in psychotropic drugs can result in a disruption to HBP meds and destabilize blood pressure control. In these situations, medical supervision is critical to ensure a safe transition and to prevent any unintended cardiovascular consequences.

Unintentional Interactions and Polypharmacy
Polypharmacy, or the concurrent use of multiple medications, is increasingly common in older adults and individuals with chronic conditions. In these scenarios, the risk of drug interactions is elevated, and so too is the risk that a seemingly innocuous medicine may become a drug to increase blood pressure due to additive or synergistic effects. For example, a patient may be on a medication to lower blood pressure, yet also be prescribed or take over-the-counter drugs that negate its effect.
This interplay can result in a confusing clinical picture where blood pressure control becomes difficult despite adherence to prescribed treatment. In some cases, the answer to the puzzle may lie in a drug that was not initially considered a culprit. This underscores the importance of a comprehensive medication review—a process in which all drugs, including supplements and herbal remedies, are evaluated for their potential to act as medication to raise blood pressure.
Even medications not traditionally associated with cardiovascular effects, such as certain cancer therapies or immunosuppressants, can indirectly influence blood pressure by altering kidney function or vascular health. Thus, a multidisciplinary approach to medication management is essential, particularly in patients with multiple health conditions.

Safeguarding Against Medication-Induced Hypertension
Preventing and managing medication-induced hypertension requires vigilance, both on the part of the healthcare provider and the patient. Clinicians should routinely assess the blood pressure implications of all medications prescribed, including those that may seem unrelated to cardiovascular health. Patients should be encouraged to maintain an up-to-date list of all the medications they use, including over-the-counter products, and to bring this list to every medical appointment.
In cases where a necessary medication is found to raise blood pressure, there are several strategies available. Dose reduction, switching to an alternative drug, or adding a medication to counteract the hypertensive effect are all viable approaches. The key lies in early identification and individualized management. Pharmacists can also play an integral role by providing counseling on drug interactions and helping patients select safer alternatives.
Technological advancements have made self-monitoring of blood pressure easier and more accessible than ever. Patients who suspect their blood pressure may be affected by a new medication should be encouraged to use home monitoring devices and report any changes to their healthcare providers. This proactive approach helps detect subtle shifts in blood pressure before they evolve into more serious problems.
Frequently Asked Questions: Medication and High Blood Pressure
1. Can stopping blood pressure medication suddenly lead to complications if you’re also taking drugs that raise blood pressure?
Yes, abruptly discontinuing antihypertensive medications while concurrently taking drugs to raise blood pressure can create a dangerous physiological rebound. This combination may result in a dramatic and sustained increase in blood pressure, putting individuals at risk of hypertensive emergencies, which include symptoms like chest pain, shortness of breath, and even stroke. Common offenders include over-the-counter decongestants or NSAIDs that function as medication to raise blood pressure, potentially undoing weeks or months of controlled hypertension. Patients often underestimate how something as simple as cold medicine can interact with a disruption to HBP meds. This risk underscores the importance of tapering medication under medical supervision and reviewing all other substances—prescription or otherwise—that might contribute to elevated BP.
2. Are there any long-term consequences of repeatedly using meds to raise blood pressure, even if only occasionally?
While occasional use of medicine to increase blood pressure may seem harmless, repeated use over time can lead to cumulative cardiovascular strain. Subclinical elevations in blood pressure, especially when unnoticed, can progressively damage arterial walls, increasing the risk of atherosclerosis and left ventricular hypertrophy. Certain drugs to increase blood pressure, including those in over-the-counter cold remedies or anti-inflammatory medications, may subtly influence kidney function over time. When combined with other lifestyle risk factors, such as a high-sodium diet or sedentary habits, the effects of these meds to increase blood pressure may become more pronounced and harder to reverse. Long-term vigilance is key to preventing insidious damage that doesn’t manifest until much later.
3. Why do medications like Aleve and Advil affect blood pressure even though they’re not heart medications?
Although Aleve and Advil are designed to reduce inflammation and pain, they inadvertently impact kidney function and fluid retention—two factors directly involved in blood pressure regulation. NSAIDs like these inhibit prostaglandins, compounds that normally help dilate blood vessels and maintain blood flow to the kidneys. When prostaglandins are suppressed, sodium retention and vasoconstriction occur, raising blood pressure in susceptible individuals. So when patients ask, “does Aleve raise blood pressure?” or “does Advil increase blood pressure?”, the answer lies not in their intended use, but in their systemic effects. This is why doctors often advise those with high blood pressure to consider alternatives to NSAIDs for pain relief.
4. Can medication cause high blood pressure even in people with no previous history of hypertension?
Absolutely. One of the lesser-known facts is that a medication to raise blood pressure can trigger hypertension in people who have never had issues before. This is particularly common when the individual is prescribed drugs with sympathomimetic properties—such as certain antidepressants, corticosteroids, or decongestants—which activate the nervous system and promote vasoconstriction. Over time, this can condition the body into a higher baseline pressure, especially if combined with stress or poor dietary habits. Early signs might include fatigue, headaches, or blurred vision, but without routine monitoring, these effects often go unnoticed until they become more serious. Regular check-ups and tracking one’s BP are critical even for those without a known cardiovascular history.
5. How does combining multiple medications increase the risk of hypertension more than taking a single drug?
Polypharmacy significantly raises the risk that at least one medication in the mix may increase blood pressure, often without the prescribing physician being fully aware of every interaction. For example, a combination of NSAIDs, oral contraceptives, and corticosteroids may collectively act as multiple drugs to increase blood pressure, even though individually their effects might be mild. When these medications are taken together—especially without disclosure to all providers involved—the cumulative impact can disrupt blood pressure regulation profoundly. This is where medication reconciliation becomes invaluable, particularly for patients seeing multiple specialists. Pharmacists and primary care physicians play a vital role in spotting these combinations early and recommending safer alternatives.
6. Does ibuprofen raise BP more significantly than other NSAIDs like naproxen (Aleve)?
Both ibuprofen and naproxen are classified as NSAIDs, but their impact on blood pressure can vary slightly depending on the individual. While clinical studies have shown that both can cause increases in blood pressure, the duration and frequency of use often determine their relative effect. Ibuprofen is typically taken in shorter intervals, sometimes leading to acute spikes in blood pressure. In contrast, Aleve (naproxen) has a longer half-life, which may result in a more prolonged but moderate elevation. The question isn’t just “does ibuprofen raise BP?” but rather how often, at what dose, and in what combination it’s being taken with other drugs to raise blood pressure. Personalized assessment is essential to understanding the true cardiovascular impact of either option.
7. Are natural supplements safer than pharmaceuticals when it comes to medication-induced hypertension?
While many people perceive natural supplements as inherently safer, several herbal compounds can actually function as meds to raise blood pressure. Ingredients such as licorice root, yohimbine, and ephedra have all been linked to elevated blood pressure, sometimes mimicking the effects of prescription medications. Additionally, natural products are not regulated with the same rigor as pharmaceuticals, which means their potency, purity, and interaction profiles are not always well-understood. This makes it difficult to determine whether a particular supplement might be acting as a medicine to increase blood pressure. Patients should disclose all supplements to their healthcare provider and approach “natural” remedies with the same caution as they would any drug.
8. What should you do if you suspect your blood pressure is being affected by a new medication?
If you notice an unexplained increase in blood pressure after starting a new medication, it’s crucial to track readings consistently and bring your concerns to a healthcare professional. Sudden spikes or gradual elevations may suggest that a medication to increase blood pressure is interfering with your normal cardiovascular rhythm. Rather than discontinuing the medication on your own—which may pose its own risks—speak with your doctor about potential alternatives or dose adjustments. Sometimes, adding a counterbalancing drug or adjusting lifestyle factors may mitigate the hypertensive effect. Keeping a log of your symptoms and BP readings provides valuable data for clinical decisions.
9. Can Aleve elevate blood pressure even if taken only occasionally for pain relief?
Yes, occasional use of Aleve can still elevate blood pressure, especially in people who are particularly sensitive to NSAIDs or who already take other medications that affect BP. Even though a single dose may not cause long-term problems, repeated intermittent use over weeks or months may still have a cumulative effect. The answer to whether Aleve increases blood pressure lies in both individual response and concurrent medication use. For example, if someone is already on a calcium channel blocker and also takes Aleve for arthritis pain, the Aleve may blunt the effectiveness of the BP medication. This reinforces the need to ask your doctor, “can Aleve increase blood pressure in my situation?” rather than relying on general assumptions.
10. What are the emerging trends in managing medication-induced high blood pressure?
The future of managing drug-related hypertension lies in more personalized, data-driven healthcare. Advances in pharmacogenomics are helping clinicians predict how a patient will respond to specific drugs, including whether a medicine to raise blood pressure is likely to trigger a hypertensive response. Digital health tools, such as smart BP monitors and integrated medication trackers, are enabling real-time feedback that improves decision-making. There is also growing awareness of the need to monitor and adjust therapy not only based on clinical guidelines but also on individual lifestyle, genetic predispositions, and drug interaction profiles. As the field evolves, the goal is to reduce the risk that a disruption to HBP meds or an unintended drug interaction will go unnoticed. Patient empowerment through education and accessible tools will be central to this new era of cardiovascular care.
Conclusion: Why It’s Crucial to Understand Which Medications Can Increase Blood Pressure
In a healthcare landscape where medications play an indispensable role in managing disease, it is essential not to overlook their potential side effects—especially those that affect cardiovascular health. The question “can medication cause high blood pressure?” is more than a pharmacological curiosity; it is a clinically significant concern that affects millions of individuals, particularly those already at risk for hypertension or cardiovascular disease.
From over-the-counter pain relievers like Aleve and Advil to antidepressants, decongestants, and hormone-based therapies, many common medications can act as drugs to raise blood pressure, often without the patient’s awareness. Understanding the implications of these drugs and asking critical questions—like “does Aleve raise blood pressure?” or “does Advil increase blood pressure?”—can empower both patients and providers to make informed, health-conscious decisions.
Ultimately, the goal is not to avoid all medications that might influence blood pressure but to use them wisely, with full awareness of their potential effects. A patient-centered approach, grounded in open communication and continuous monitoring, can help mitigate the risks and maintain cardiovascular stability. As our understanding of these drug interactions grows, so too does our ability to personalize care, minimize harm, and optimize outcomes in the ongoing effort to combat hypertension and its many associated challenges.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Medications and supplements that can raise your blood pressure


