Introduction: Why the Esophagus Deserves More Attention
The human digestive system is a marvel of biological engineering, transforming the food we eat into nutrients essential for survival. While the stomach and intestines often dominate discussions about digestion, the esophagus plays a quietly vital role that is frequently overlooked. To understand what happens at the esophagus, it is important to look beyond its anatomical simplicity and delve into its nuanced functions, interrelated systems, and implications for overall gut health. The esophagus serves as a crucial passageway that does more than merely shuttle food; it initiates complex neuromuscular interactions, safeguards the airway, and coordinates with the central nervous system to ensure seamless digestion.
You may also like: Macronutrients vs Micronutrients: What the Simple Definition of Macronutrients Reveals About Your Diet and Health
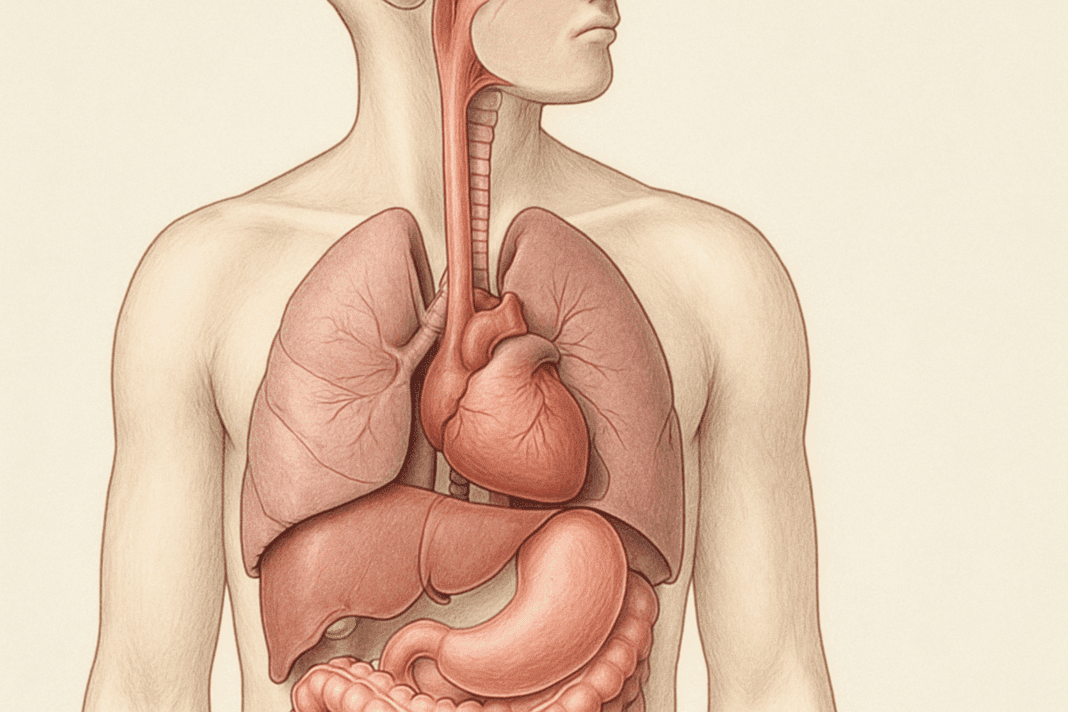
Anatomy and Structure of the Esophagus
At its core, the esophagus is a muscular tube approximately 8 to 10 inches long, stretching from the throat (pharynx) to the stomach. It traverses the thoracic cavity, passing behind the trachea and heart, through the diaphragm, and into the abdominal cavity. Structurally, it consists of multiple layers: a mucosal lining, submucosal tissue rich in glands, a muscularis layer responsible for movement, and an outer adventitial covering. These layers work in harmony to fulfill the esophagus function in the digestive system. The inner lining secretes mucus that facilitates the smooth passage of food, while the muscular layer contracts rhythmically to propel the food bolus downward in a process called peristalsis. This coordinated muscular action is essential for delivering food safely and efficiently to the stomach, particularly when gravity is not aiding the process, such as when lying down or swallowing upside down.
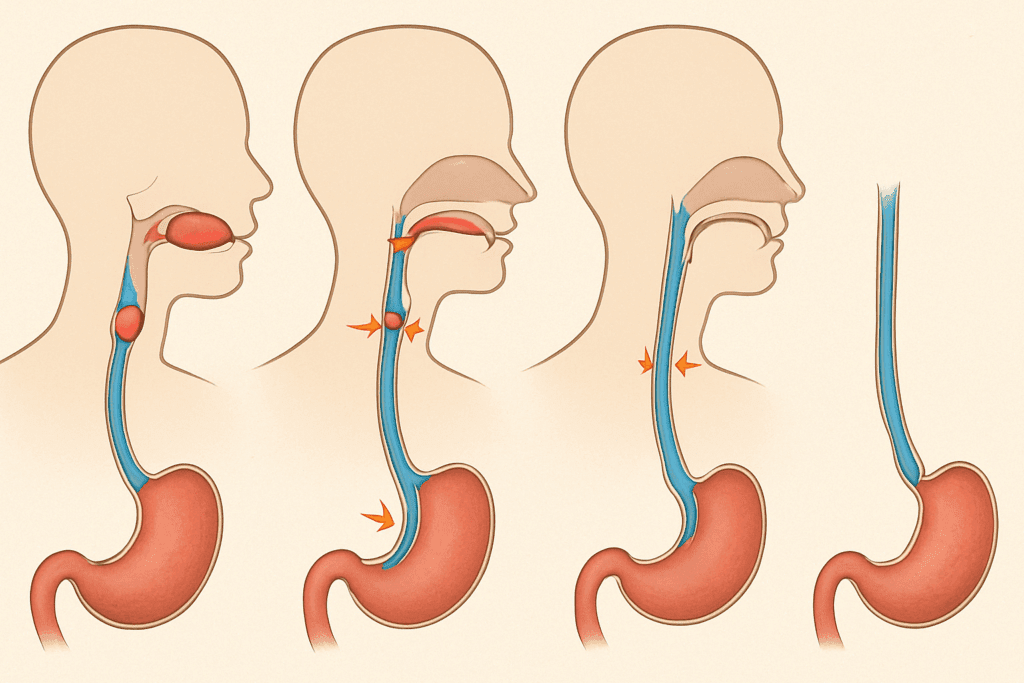
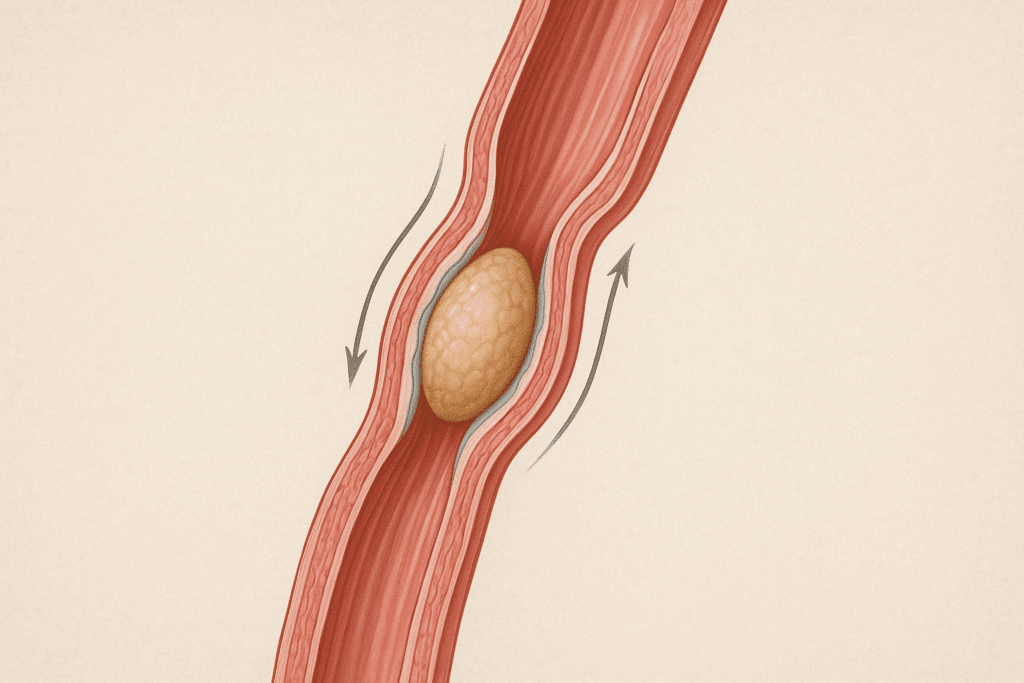
How the Esophagus Works: From Swallowing to Stomach
A deeper exploration into what happens at the esophagus reveals that its operation begins even before the first bite is swallowed. Chewing activates sensory receptors in the mouth that signal the brain to prepare the digestive system for incoming material. Once a bolus is formed and swallowed, the upper esophageal sphincter (UES) relaxes, allowing it to enter the esophagus. This action triggers peristaltic waves—sequential contractions of the esophageal muscles—that move the bolus downward toward the stomach. During this journey, the lower esophageal sphincter (LES) remains closed to prevent gastric reflux. When the bolus reaches the LES, it temporarily relaxes to allow entry into the stomach, then tightens again to maintain a barrier against stomach acid. Each of these events reflects a complex interaction between voluntary and involuntary neural controls that exemplify the esophagus function in the digestive system.
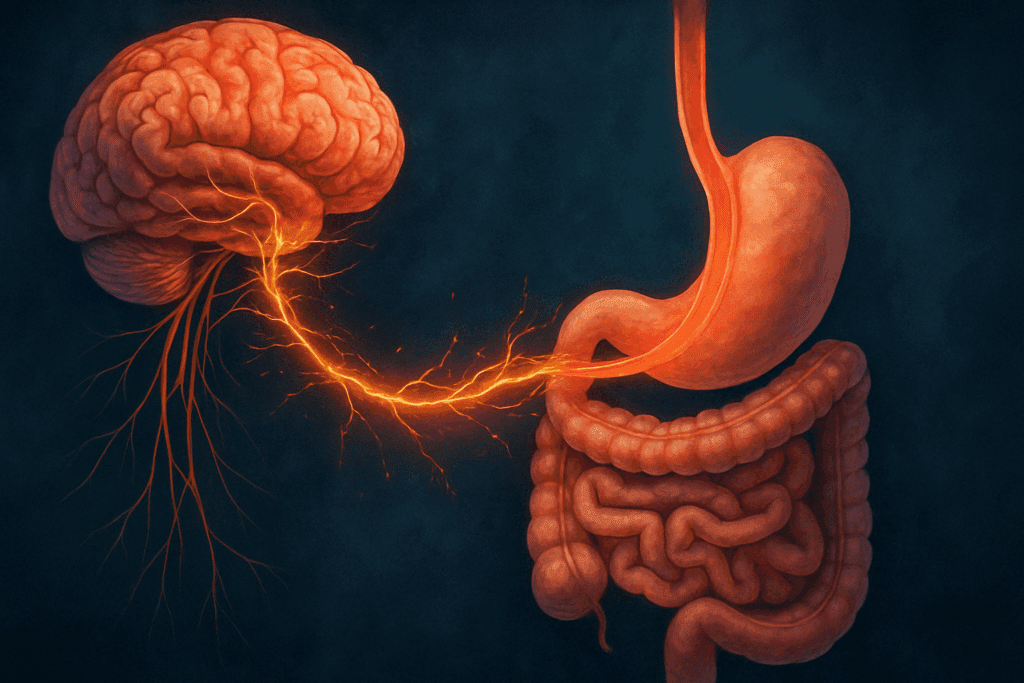
The Gut-Brain Connection: Esophageal Function and Emotional Health
Contrary to the simplistic view of the esophagus as a passive conduit, emerging studies have illustrated its responsiveness to a range of mechanical, chemical, and even emotional stimuli. For example, the perception of stress or anxiety can affect esophageal motility, sometimes resulting in symptoms like globus sensation (a feeling of a lump in the throat) or functional chest pain. These phenomena underscore the gut-brain axis, a bidirectional communication system linking emotional and cognitive centers of the brain with peripheral intestinal functions. Understanding what happens at the esophagus, therefore, also requires considering how systemic physiological and psychological factors influence esophageal behavior. Such insights are especially relevant in modern wellness contexts where gut health is increasingly linked to mental well-being.
Common Esophageal Disorders and Their Impacts
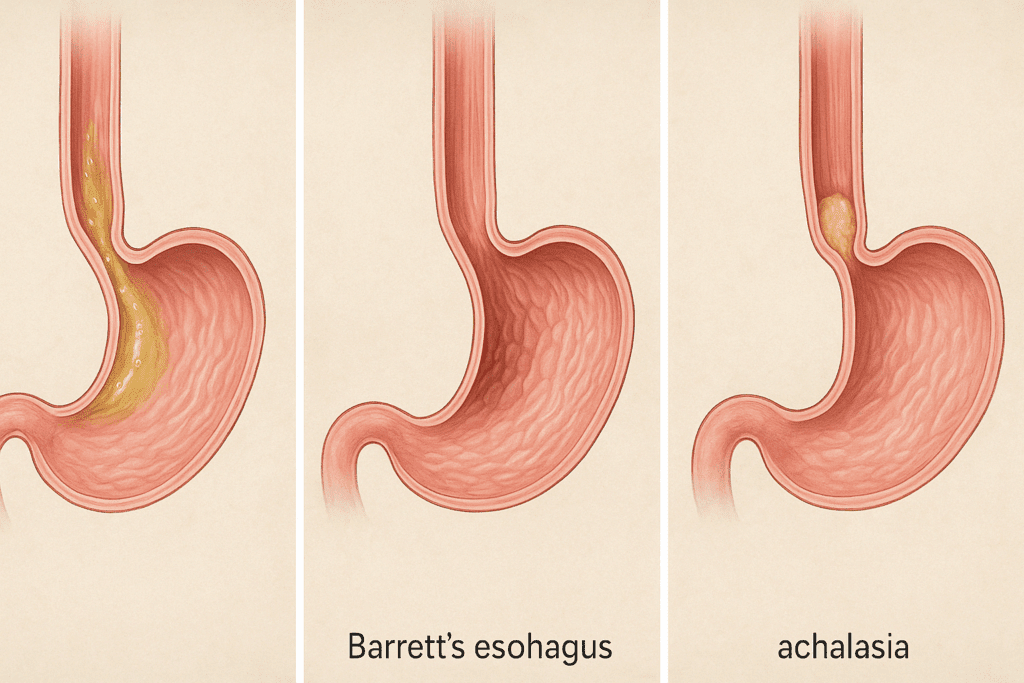
From a clinical perspective, disorders of the esophagus can significantly impair digestive efficiency and quality of life. Conditions such as gastroesophageal reflux disease (GERD), esophagitis, achalasia, and Barrett’s esophagus stem from malfunctions in the esophagus function in the digestive system. GERD, for instance, results when the LES fails to close properly, allowing stomach acid to flow backward into the esophagus, causing irritation and inflammation. Left untreated, chronic GERD can lead to esophagitis or Barrett’s esophagus, a condition involving precancerous changes in the esophageal lining. Achalasia, on the other hand, is a rare disorder where the LES fails to relax, obstructing food passage and leading to difficulty swallowing. These examples illustrate that disruptions in esophageal function are not just uncomfortable—they are potentially dangerous, demanding timely medical attention and management.
Nutrition and Its Role in Supporting Esophageal Health
Esophageal health is intricately tied to nutritional habits, making it a topic of growing relevance within the context of diet and prevention. The foods we choose to consume can either support or sabotage the delicate balance of function along the digestive tract. For individuals with sensitive esophageal linings, acidic, spicy, or heavily processed foods can exacerbate inflammation and contribute to symptoms like heartburn or regurgitation. On the contrary, a diet rich in anti-inflammatory foods—such as leafy greens, whole grains, bananas, and lean proteins—can help soothe and protect the esophageal mucosa. When examining what happens at the esophagus, it becomes clear that food serves not only as fuel but as a modulator of digestive tract integrity. Avoiding late-night meals, eating slowly, and maintaining an upright posture after eating are additional strategies that can protect esophageal function and enhance gut health.
Diagnostic Tools for Evaluating Esophageal Function
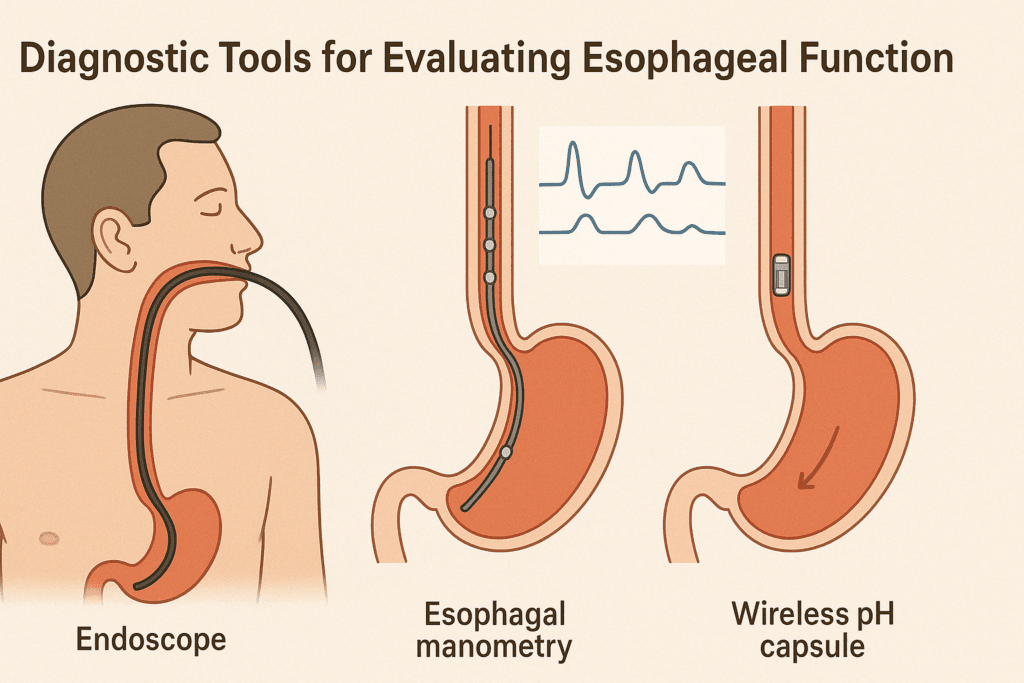
Another important dimension in understanding the esophagus function in the digestive system lies in the realm of diagnostics and preventive screenings. Technologies such as endoscopy, esophageal manometry, and pH monitoring have allowed clinicians to evaluate esophageal structure and function with remarkable precision. Endoscopy, for example, provides a visual assessment of the esophageal lining, identifying inflammation, ulcers, strictures, or abnormal cellular changes. Esophageal manometry measures the rhythmic contractions and pressure within the esophagus, offering insights into conditions like achalasia or diffuse esophageal spasm. These diagnostic tools not only aid in the detection of pathology but also help guide dietary and therapeutic interventions that are tailored to individual needs. With the rising awareness around preventative health, early identification of esophageal dysfunction is increasingly prioritized as a key strategy for safeguarding long-term digestive wellness.
Lifestyle Factors and Their Influence on the Esophagus
Furthermore, lifestyle factors outside of diet also shape esophageal health. Smoking, alcohol consumption, obesity, and sedentary habits have all been implicated in compromised esophageal function. Nicotine and alcohol can weaken the LES, increasing the risk of acid reflux, while obesity raises intra-abdominal pressure, further stressing the esophageal barrier. Incorporating regular physical activity and maintaining a healthy weight are foundational strategies for preventing reflux-related conditions. Even sleep position plays a role; studies have shown that elevating the head during sleep or sleeping on the left side can reduce nighttime reflux episodes. Such practical insights reinforce that understanding what happens at the esophagus is not solely a matter of anatomy but one of lifestyle integration. A comprehensive view that considers diet, movement, sleep, and stress management offers the most effective blueprint for esophageal and overall gut health.
The Esophageal Microbiome: A New Frontier in Gut Science
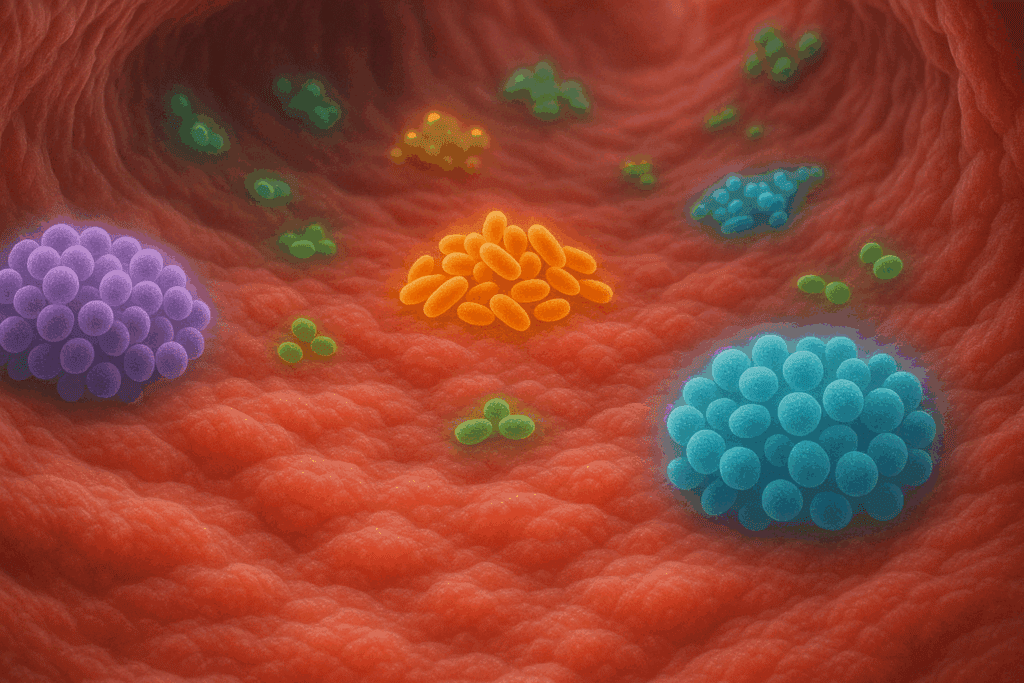
Interestingly, new frontiers in microbiome research are beginning to shine a light on the esophagus as more than a sterile tube. Traditionally, the esophagus was not considered a site of microbial activity due to its transit function and exposure to saliva and gastric acid. However, recent studies have identified distinct microbial communities residing in the esophagus, including various species of Streptococcus, Prevotella, and Veillonella. These microbes may play roles in modulating immune responses, maintaining mucosal integrity, and even influencing disease susceptibility. Disruptions in this microbiome—termed dysbiosis—have been linked to conditions such as esophagitis and Barrett’s esophagus. While the research is still evolving, these findings offer promising avenues for probiotic or microbiota-targeted therapies aimed at restoring balance within this underappreciated section of the digestive tract. It also reinforces that the esophagus function in the digestive system may be more dynamic and interactive than previously understood.
Pediatric and Geriatric Perspectives on Esophageal Health
Pediatric esophageal health introduces another layer of complexity, as developmental differences affect structure and function. In infants, the LES is not fully developed, which is why reflux or “spitting up” is common in the early months. While most infants outgrow this condition, persistent or severe cases may indicate gastroesophageal reflux disease or structural anomalies like esophageal atresia. Early detection and management are crucial in such scenarios to prevent feeding difficulties, respiratory complications, and developmental delays. Pediatric specialists often focus on optimizing feeding techniques, positioning strategies, and in rare cases, surgical correction. A thorough grasp of what happens at the esophagus during early life stages provides valuable insights for parents and healthcare providers aiming to support healthy growth and development from infancy onward.
Age-related changes in esophageal function also warrant attention, particularly among older adults. Aging is associated with decreased muscle tone and slower peristalsis, which can impair the timely movement of food and increase the risk of dysphagia (difficulty swallowing). In addition, older adults may experience diminished sensitivity in the esophageal lining, making them less likely to notice or report symptoms of reflux or irritation. These physiological shifts necessitate tailored dietary recommendations, such as softer food textures, smaller meals, and prolonged chewing to facilitate easier swallowing. Furthermore, older adults may be more susceptible to polypharmacy, where multiple medications contribute to esophageal irritation or impaired motility. Recognizing these age-specific considerations enhances our broader understanding of esophagus function in the digestive system and helps ensure that interventions remain appropriately individualized.
Promoting Wellness Through Esophageal Awareness
In the realm of prevention and wellness, empowering individuals with actionable knowledge about esophageal health can significantly reduce the burden of digestive disorders. Educational initiatives that promote awareness of early warning signs—such as persistent heartburn, difficulty swallowing, chronic cough, or unexplained weight loss—enable timely medical consultation and intervention. Simple lifestyle modifications like avoiding tight-fitting clothing around the abdomen, limiting caffeine, and practicing mindful eating can have profound effects on esophageal resilience. Understanding what happens at the esophagus is no longer a niche topic reserved for specialists; it is essential information for anyone seeking to maintain long-term gut health. The rise of wearable devices and health tracking apps further empowers individuals to monitor symptoms and triggers, creating a more proactive and personalized approach to digestive care.
Innovation in Esophageal Treatment and Diagnosis
Technological innovation continues to reshape how we assess and support esophageal health. The development of minimally invasive diagnostic tools, such as capsule endoscopy and wireless pH monitoring, has made it easier for individuals to undergo thorough evaluations without extensive discomfort. Meanwhile, advances in surgical and therapeutic interventions—from LINX devices that reinforce the LES to endoscopic ablation for precancerous changes—offer new hope for patients with chronic or advanced esophageal conditions. As precision medicine evolves, integrating genetic, microbiomic, and lifestyle data will likely enhance our ability to tailor treatments that optimize esophagus function in the digestive system for each unique individual. The intersection of science, technology, and personalized care represents the future of esophageal wellness.
Frequently Asked Questions: What Happens at the Esophagus and Its Role in Digestive Health
1. How does posture affect what happens at the esophagus during digestion? Posture plays a more significant role in esophageal health than most people realize. Upright posture supports gravity in moving the food bolus downward and helps the lower esophageal sphincter stay closed to prevent reflux. Slouching, especially post-meal, can increase pressure on the abdomen and compromise the esophagus function in the digestive system by encouraging acid to flow backward. Studies have shown that people who habitually recline after eating are at greater risk for developing gastroesophageal reflux symptoms. Incorporating simple habits like walking after meals or eating in an upright seated position can dramatically improve what happens at the esophagus after swallowing.
2. Can emotional stress directly influence esophageal function? Yes, emotional stress can significantly affect esophageal motility and perception. Stress can disrupt autonomic nervous system regulation, leading to erratic peristalsis and spasms. This can result in non-cardiac chest pain, difficulty swallowing, or a tightness in the throat. The esophagus function in digestive system operations is partially governed by the brain-gut axis, which means that psychological well-being influences physical digestion. Understanding what happens at the esophagus in response to emotional triggers helps us appreciate why stress-reducing strategies like meditation or biofeedback can alleviate esophageal discomfort.
3. Are there any early signs of esophageal dysfunction people often miss? Subtle symptoms such as mild throat clearing, occasional hoarseness, or a persistent dry cough are often overlooked but can indicate esophageal issues. These early signs typically stem from minor reflux events that irritate the upper airway. When assessing what happens at the esophagus, it becomes clear that the tissue is highly sensitive to even minimal exposure to stomach contents. People may not experience heartburn but still suffer from “silent reflux,” which can be diagnosed through specialized pH monitoring. Early attention to these signs can prevent progression to more serious esophageal conditions.
4. What role does hydration play in supporting esophageal function? Hydration is essential for the smooth transit of food and the prevention of esophageal irritation. Adequate fluid intake helps maintain a well-lubricated mucosal lining, facilitating easier swallowing and reducing the likelihood of food sticking mid-esophagus. Dehydration can make the esophagus more susceptible to spasms or minor abrasions, especially in older adults. What happens at the esophagus when fluid intake is inadequate often involves slower motility and increased discomfort. In the broader context of esophagus function in digestive system maintenance, water also assists in neutralizing gastric acid, offering additional protection against reflux.
5. How does aging affect what happens at the esophagus during meals? With aging, esophageal motility tends to slow, and the coordination between swallowing muscles can weaken. This can lead to incomplete clearance of food, increasing the risk of aspiration or sensation of food being stuck. As part of the aging process, the esophagus function in digestive system performance gradually becomes less efficient, particularly when paired with multiple medications or systemic diseases. Older adults may also become desensitized to typical reflux symptoms, delaying diagnosis. Proactive adjustments such as smaller meal portions and texture-modified diets can help support esophageal function later in life.
6. Is there a connection between breathing patterns and esophageal function? Breathing and swallowing are intricately coordinated activities. Disruptions in breathing patterns, particularly in individuals with chronic obstructive pulmonary disease (COPD) or sleep apnea, can negatively impact esophageal clearance. Dysfunctional breathing increases intra-abdominal pressure, which alters what happens at the esophagus during digestion and rest. Shallow breathing may reduce diaphragm support for the lower esophageal sphincter, increasing the likelihood of reflux. Strengthening diaphragmatic breathing techniques may offer therapeutic benefits by enhancing the esophagus function in digestive system regulation.
7. What innovations are emerging in the field of esophageal diagnostics? Recent advancements include wireless pH monitoring capsules, which patients can swallow to track acid exposure without a nasal tube. High-resolution manometry offers improved detection of subtle motility disorders by mapping pressure zones throughout the esophagus in real time. These tools provide a deeper understanding of what happens at the esophagus beyond surface symptoms, especially in patients with unexplained dysphagia or chest discomfort. Esophageal impedance testing is another innovation that helps detect non-acid reflux events. Together, these emerging technologies refine our approach to diagnosing abnormalities in esophagus function in the digestive system.
8. Can exercise influence esophageal health positively or negatively? Moderate exercise has a positive influence on digestion by enhancing peristalsis and promoting healthy weight maintenance. However, intense workouts—particularly those involving core strain or inverted positions—can exacerbate reflux symptoms. Athletes performing high-impact sports may experience transient disruptions in what happens at the esophagus due to sudden changes in intra-abdominal pressure. To protect esophagus function in digestive system balance, it’s advisable to avoid vigorous activity immediately after meals and to wear loose-fitting clothing during workouts. Tailoring physical activity based on reflux patterns can optimize digestive comfort and performance.
9. How does the esophagus adapt to frequent acid exposure over time? Chronic exposure to gastric acid may lead to cellular changes in the esophagus lining, a process known as metaplasia. This adaptive response forms the basis of Barrett’s esophagus, where the normal squamous cells are replaced by columnar cells better suited to withstand acid but with increased cancer risk. In understanding what happens at the esophagus long-term, it’s clear that repeated damage pushes the tissue into a defensive mode that sacrifices normal function. Patients with long-standing reflux require monitoring to detect these precancerous changes early. This reinforces why preserving esophagus function in digestive system processes must be a long-term health priority.
10. Are there any promising therapies focused specifically on esophageal wellness? Beyond acid blockers and surgery, newer therapies aim to support the esophagus holistically. Esophageal-directed physical therapy is being explored to strengthen swallowing muscles and enhance neuromuscular coordination. Nutraceuticals such as alginate-based compounds form a physical barrier to protect the esophageal lining from acid without affecting systemic pH. Researchers are also investigating targeted microbiome therapies that could influence what happens at the esophagus by modulating inflammation and mucosal health. These innovations highlight the evolving understanding of esophagus function in the digestive system and underscore the shift toward integrative, precision-focused care.
Conclusion: Promoting Gut Wellness Through Esophageal Health
Reflecting on the complexity and significance of what happens at the esophagus reveals that this seemingly simple structure holds a pivotal role in digestive and overall wellness. It is not merely a passive passageway but a dynamic participant in a deeply integrated system. The esophagus function in the digestive system encompasses precise muscular coordination, barrier protection, microbial interaction, and responsiveness to diet and emotional states. Its health influences everything from nutrient absorption to immune defense and even mental well-being. Recognizing its importance empowers individuals to make informed lifestyle and dietary choices that protect this essential component of their gastrointestinal health.
As scientific understanding continues to evolve, so too does our appreciation for the esophagus as more than a background player in digestion. Preventive care, early intervention, and lifestyle alignment stand as pillars of esophageal health promotion. Through mindfulness in eating, attention to symptoms, and collaboration with healthcare providers, individuals can protect and enhance this critical digestive pathway. Understanding what happens at the esophagus opens the door to a more informed and proactive approach to gut health—one where prevention, personalization, and daily choices converge to support long-term vitality and wellness.