In the realm of cardiovascular health, few statistics are as sobering as those associated with uncontrolled hypertension. Among these, the highest blood pressure ever recorded stands as both a medical anomaly and a stark warning. This rare and extreme occurrence highlights not only the devastating potential of hypertensive crises but also the broader challenges surrounding high blood pressure management across populations. By exploring the circumstances, implications, and preventive lessons of this medical milestone, we gain a deeper understanding of how the human body responds to extreme physiological stress and how such insights can help inform more effective cardiovascular care.
Blood pressure, a critical vital sign, reflects the force of blood against artery walls as the heart pumps. While normal readings typically fall below 120/80 mmHg, readings above 180/120 mmHg constitute a hypertensive crisis, requiring immediate medical intervention. In extraordinary cases, however, blood pressure levels have surged to unprecedented heights—posing serious, and sometimes fatal, health risks. Understanding the factors behind the highest blood pressure ever recorded can help demystify extreme hypertension and reinforce the importance of early detection, lifestyle intervention, and targeted treatment.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Documented Cases and Medical Insights from the Highest BP Ever Recorded
Reports of the highest blood pressure ever recorded in medical literature have largely come from emergency departments dealing with hypertensive emergencies. One often-cited instance involved a patient whose blood pressure spiked to an astonishing 370/360 mmHg—an extraordinarily rare and life-threatening condition. This case, while extreme, serves as a powerful case study in the resilience and fragility of the cardiovascular system. Such readings far exceed the threshold for hypertensive crisis and are often accompanied by symptoms such as severe headache, blurred vision, confusion, chest pain, and organ damage.
Medical experts agree that cases like these typically result from a combination of untreated hypertension, underlying medical conditions (such as renal disease or adrenal gland tumors), and lifestyle factors including chronic stress, poor diet, and substance use. In the rare instance of the highest bp ever recorded, the patient survived—but not without extensive cardiovascular damage and a long recovery. These stories serve as cautionary tales for clinicians and patients alike, emphasizing the need for vigilant blood pressure monitoring and early therapeutic intervention.
The Pathophysiology of Severe Hypertension and Hypertensive Crisis
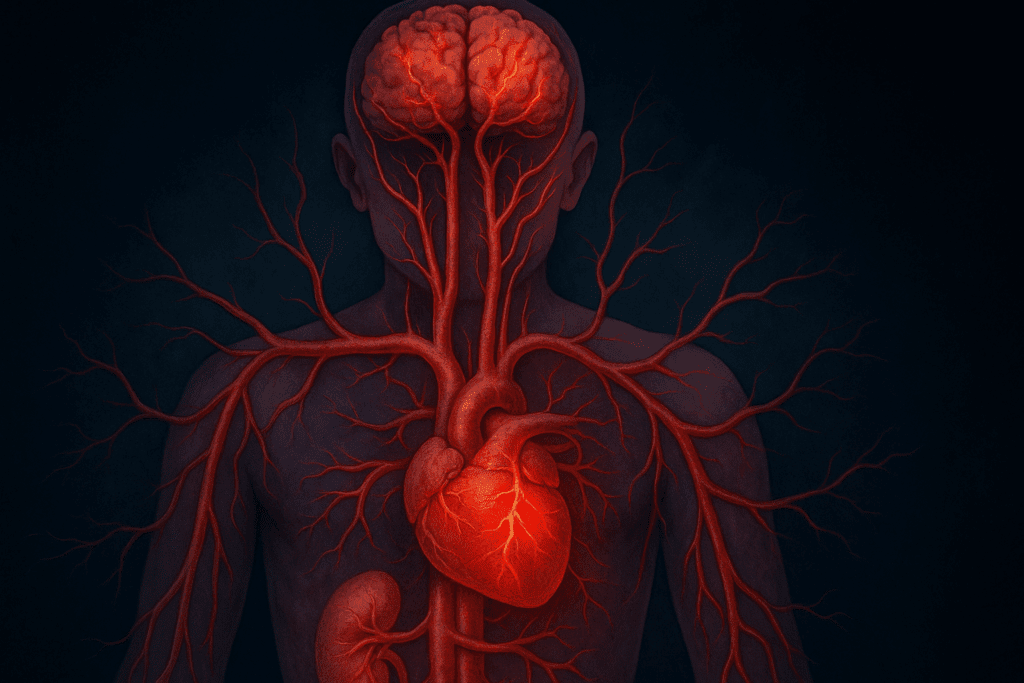
To understand how the body can withstand such extreme pressure readings, it is important to examine the pathophysiology of a hypertensive crisis. When blood pressure rises to dangerous levels, the body’s autoregulatory mechanisms—which typically maintain steady perfusion of vital organs—begin to fail. As a result, endothelial injury, vasoconstriction, and inflammation escalate, leading to potential damage in organs like the heart, brain, kidneys, and eyes.
In scenarios where individuals approach or surpass the highest blood pressure ever recorded, the risk of stroke, myocardial infarction, aortic dissection, and acute renal failure dramatically increases. The heart, in particular, faces immense strain. Sustained pressure overload can cause left ventricular hypertrophy, reduced ejection fraction, and eventually heart failure. The brain is similarly vulnerable, with hypertensive encephalopathy and hemorrhagic stroke representing common and devastating consequences of unmitigated high blood pressure.
Recognizing the Symptoms and Red Flags of a Hypertensive Emergency
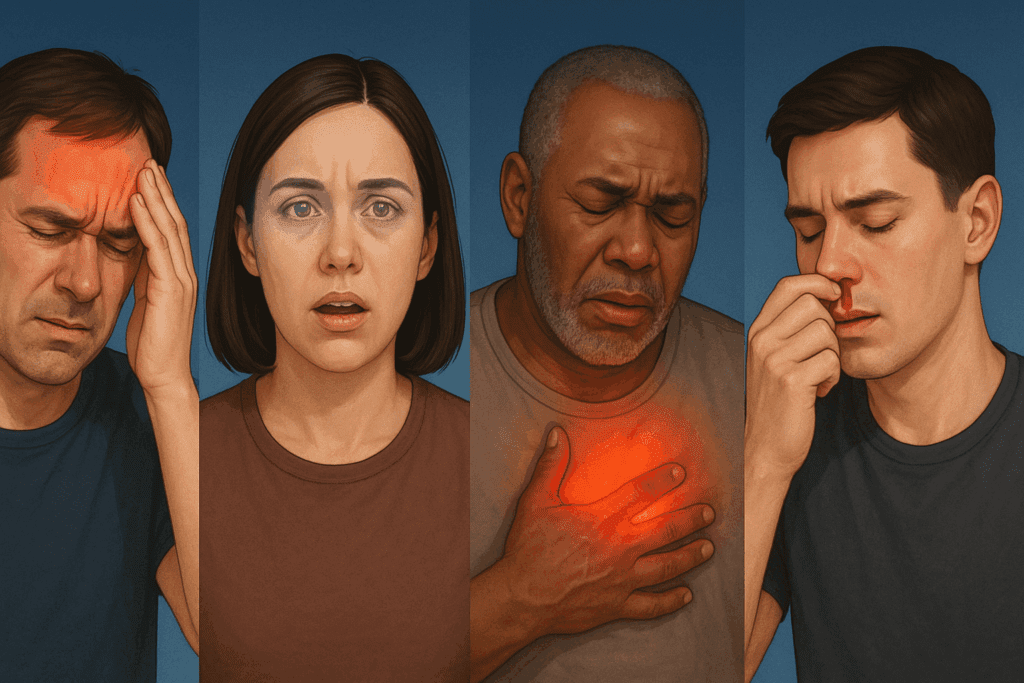
While most individuals with high blood pressure experience no symptoms—earning it the nickname “the silent killer”—a hypertensive emergency often announces itself with unmistakable warning signs. These include sudden and severe headaches, confusion, visual disturbances, chest discomfort, shortness of breath, and nosebleeds. In cases approaching the highest bp ever recorded, multiple symptoms typically present simultaneously, indicating imminent organ damage.
Prompt recognition and immediate treatment are vital to prevent irreversible harm. In emergency rooms, patients presenting with severe hypertension are typically administered intravenous antihypertensives to gradually and safely lower blood pressure. Rapid reductions are avoided to prevent ischemia in organs that have adapted to chronically high pressures. This delicate balancing act requires both clinical precision and swift decision-making.

Contributing Factors Behind Extremely High Blood Pressure Readings
The highest blood pressure ever recorded did not occur in isolation. Such extreme readings generally stem from complex interactions between genetic, environmental, and behavioral factors. Primary (essential) hypertension—responsible for the majority of cases—often emerges from a confluence of poor dietary habits, sedentary lifestyle, obesity, and excessive sodium intake. However, secondary hypertension, which results from underlying medical conditions such as chronic kidney disease, thyroid dysfunction, or pheochromocytoma, can also escalate to life-threatening levels.
Medication nonadherence plays a significant role in hypertensive crises. Studies show that individuals who discontinue their antihypertensive medications without medical guidance are at elevated risk for rebound hypertension and hypertensive emergencies. Furthermore, the use of substances such as cocaine, amphetamines, and certain over-the-counter decongestants can precipitate dangerous spikes in blood pressure. In patients with known cardiovascular risk, even temporary elevations can provoke acute events.
Understanding the Psychological and Social Dimensions of Hypertension
Though often viewed through a strictly biological lens, hypertension is deeply intertwined with psychological and social determinants of health. Chronic stress, for example, triggers sustained activation of the sympathetic nervous system, contributing to elevated blood pressure over time. Socioeconomic factors—including limited access to healthcare, food insecurity, and lack of social support—can exacerbate risk and hinder effective management.
The highest bp ever recorded may reflect not only medical neglect but also systemic gaps in public health infrastructure. Addressing these issues requires a holistic approach that considers mental health, cultural competence, and community-based interventions. Programs that incorporate behavioral counseling, patient education, and social support have shown promising outcomes in improving blood pressure control, particularly in underserved populations.
Long-Term Consequences of Uncontrolled Hypertension
Even in less extreme cases, sustained high blood pressure inflicts cumulative damage on the body. Over time, elevated pressures wear down the arterial walls, promoting atherosclerosis and increasing the risk of heart attack and stroke. The kidneys, responsible for filtering waste and regulating blood volume, are particularly sensitive to pressure overload. Hypertensive nephropathy, a leading cause of end-stage renal disease, is often preventable through diligent management of blood pressure.
In patients who have experienced readings close to or beyond the highest blood pressure ever recorded, long-term prognosis depends on the timeliness and effectiveness of intervention. Organ damage may persist even after blood pressure is brought under control, underscoring the importance of preventive care. Cardiologists often recommend comprehensive evaluations, including echocardiograms, renal function tests, and retinal imaging, to assess the extent of hypertension-induced damage.

Clinical Strategies for Preventing Hypertensive Crisis
Preventing the recurrence of hypertensive emergencies involves more than just prescribing medication. A multifaceted, patient-centered approach is essential. First and foremost, accurate diagnosis and classification of hypertension help tailor therapy to individual needs. Lifestyle modifications—including a DASH (Dietary Approaches to Stop Hypertension) diet, regular physical activity, weight management, and reduced alcohol intake—form the foundation of long-term blood pressure control.
Pharmacologic interventions must be carefully selected and monitored, taking into account patient comorbidities, drug interactions, and adherence challenges. For individuals at risk of experiencing the highest blood pressure ever recorded or a similar crisis, clinicians often opt for combination therapy and frequent follow-ups. Ambulatory blood pressure monitoring, home readings, and digital health tools can support real-time tracking and early identification of concerning trends.
Educating Patients and Communities on Blood Pressure Management
Empowering patients with knowledge is a cornerstone of effective hypertension management. Many individuals remain unaware of their blood pressure status until symptoms emerge or a routine check-up reveals a problem. Public health campaigns, workplace screenings, and community outreach initiatives can play a critical role in raising awareness and promoting regular monitoring.
Incorporating culturally sensitive education about nutrition, stress management, and medication use can further enhance engagement and outcomes. In populations where mistrust of medical systems persists, leveraging community health workers and peer educators can bridge gaps and foster trust. Addressing the root causes that contribute to poor control—such as healthcare access, cost of medications, and language barriers—is crucial to reducing the incidence of extreme hypertension.
What the Highest Blood Pressure Ever Recorded Teaches Us About Human Physiology
From a physiological standpoint, the fact that some individuals survive near-superhuman spikes in blood pressure offers insight into the body’s adaptive capacities. The cardiovascular system, though vulnerable, is remarkably resilient under stress. In documented cases of extreme hypertension, rapid vascular remodeling, collateral circulation, and neurohormonal compensations may contribute to temporary survival—though not without consequences.
Researchers studying the highest bp ever recorded are increasingly interested in genetic predispositions, endothelial function, and inflammatory markers that may distinguish high-risk individuals. These investigations hold potential for personalized medicine approaches in hypertension care. By identifying early biomarkers of hypertensive damage, clinicians may one day intervene before catastrophic levels are reached.
Reevaluating Healthcare Systems to Address the Silent Epidemic
The rarity of extreme cases like the highest blood pressure ever recorded should not obscure the broader epidemic of hypertension affecting millions worldwide. Despite the availability of effective treatments, control rates remain suboptimal in many regions, particularly in low- and middle-income countries. Fragmented healthcare delivery, insufficient follow-up, and inequities in access perpetuate poor outcomes.
To address these challenges, health systems must prioritize chronic disease management, invest in primary care infrastructure, and embrace technology-driven solutions. Digital platforms that enable remote monitoring, telemedicine consultations, and personalized education can support patient adherence and timely interventions. Population-level strategies—such as sodium reduction policies, food labeling regulations, and workplace wellness programs—also contribute to long-term risk reduction.
Frequently Asked Questions: Insights Beyond the Highest Blood Pressure Ever Recorded
1. Can emotional trauma or PTSD contribute to extreme blood pressure spikes?
Absolutely. Psychological trauma, especially post-traumatic stress disorder (PTSD), has been increasingly linked to the development of uncontrolled hypertension. Individuals living with untreated or poorly managed PTSD may experience hypervigilance, chronic anxiety, and sleep disturbances, which can activate the sympathetic nervous system and lead to persistent elevations in blood pressure. In rare instances, such surges may resemble the conditions seen in cases approaching the highest blood pressure ever recorded. Research is uncovering how stress-related hormonal imbalances, such as elevated cortisol and adrenaline, exacerbate vascular resistance and compromise cardiovascular resilience. As such, integrating trauma-informed care into hypertension management could be essential for those with a history of emotional trauma.
2. Are there any populations more genetically predisposed to extremely high blood pressure?
Emerging studies suggest that certain populations may indeed be more vulnerable to reaching hypertensive extremes due to genetic polymorphisms. For example, people of African descent are more likely to develop salt-sensitive hypertension, which can rapidly escalate without proper dietary interventions. This predisposition partially explains the higher rates of stroke and kidney failure in these populations when blood pressure is poorly managed. Although the highest bp ever recorded is an anomaly, genetic research continues to identify mutations in genes regulating aldosterone and renin that may predispose individuals to life-threatening blood pressure levels. This points toward a future where genomic screening could personalize hypertension prevention strategies.
3. How do environmental stressors influence blood pressure in vulnerable communities?
Environmental factors—such as noise pollution, urban overcrowding, poor air quality, and limited green spaces—can subtly but powerfully contribute to chronically elevated blood pressure. Individuals living in underserved areas often face these stressors daily, leading to allostatic load, which is the cumulative burden of chronic stress on the body. When layered with socioeconomic hardship and limited access to healthcare, the risk of uncontrolled hypertension, and by extension the possibility of nearing the highest blood pressure ever recorded, becomes more than a theoretical concern. These insights underline the importance of urban planning, environmental justice, and social policy in long-term cardiovascular health management. Addressing environmental contributors is not only a public health imperative but also a necessary step toward health equity.
4. Is it possible for blood pressure readings to be falsely elevated in clinical settings?
Yes, this is known as “white coat hypertension,” where patients experience elevated readings due to anxiety in clinical environments. While typically benign, repeated overestimations can lead to overtreatment or misclassification of cardiovascular risk. In extremely rare scenarios, white coat hypertension has led to readings mimicking those seen in cases of the highest blood pressure ever recorded, though such spikes usually normalize when measured in a more relaxed setting. Ambulatory blood pressure monitoring (ABPM) and home-based readings are considered more reliable for assessing true blood pressure patterns. Physicians now advocate for comprehensive monitoring before making high-stakes clinical decisions.
5. Could wearable technology play a role in preventing hypertensive crises?
Absolutely. The rapid evolution of wearable health technology now enables continuous monitoring of heart rate, stress levels, and in some cases, blood pressure. These devices may serve as early-warning systems, alerting users and clinicians to dangerous trends long before a crisis unfolds. For individuals at risk of extremely high readings, including those who have previously approached the highest blood pressure ever recorded, wearables offer a proactive means of managing health in real time. In the near future, integration with telemedicine and AI-based risk prediction could enhance their role in personalized cardiovascular care. However, validation and accuracy across diverse populations remain critical hurdles to mainstream clinical adoption.
6. How does the concept of blood pressure variability affect long-term cardiovascular risk?
Blood pressure variability (BPV) refers to fluctuations in blood pressure over time—whether daily, weekly, or seasonally. While a single extremely high reading might not match the clinical gravity of the highest bp ever recorded, wide variations in blood pressure have been shown to independently increase the risk of stroke, heart attack, and mortality. BPV can reflect poor medication adherence, inconsistent lifestyle behaviors, or underlying autonomic dysfunction. Managing BPV often requires adjusting medication timing, improving sleep quality, and addressing hidden triggers like sleep apnea or dehydration. As researchers learn more about BPV’s implications, it may become a new frontier in advanced hypertension management.
7. Are current clinical guidelines equipped to prevent such extreme blood pressure cases?
While most clinical guidelines emphasize routine screening and tiered treatment protocols, they may fall short in identifying patients at risk for exceptionally high readings. Cases nearing the highest blood pressure ever recorded often emerge from a backdrop of neglected warning signs, insufficient follow-up, or social barriers to care. Integrating social determinants of health into clinical practice guidelines could enhance early risk identification. Additionally, the push toward team-based care—where pharmacists, dietitians, and mental health professionals collaborate—shows promise in preventing escalation. Some experts argue that incorporating digital biomarkers and behavioral analytics into standard care models may be essential for forecasting hypertensive crises.
8. Can extreme hypertension alter the structure of the brain over time?
Chronic exposure to dangerously high blood pressure can indeed lead to structural changes in the brain, including microvascular damage, white matter lesions, and cortical thinning. These alterations are associated with cognitive decline, increased risk of dementia, and even personality changes. In individuals who have come close to or experienced the highest blood pressure ever recorded, long-term neurological monitoring is advised to assess damage that may not be immediately evident. Magnetic resonance imaging (MRI) and neurocognitive assessments are tools increasingly used to quantify hypertension-related brain changes. These developments are prompting more neurologists to engage in interdisciplinary hypertension care.
9. How might advancements in personalized medicine change the landscape for hypertension management?
Personalized medicine, driven by genomics and metabolomics, is revolutionizing how clinicians understand and treat complex conditions like hypertension. Rather than applying a one-size-fits-all approach, physicians can now tailor therapies based on a patient’s genetic makeup, lifestyle, and even gut microbiota. For individuals prone to extreme hypertensive episodes—including those approaching the highest bp ever recorded—this could mean more targeted interventions and fewer side effects. Pharmacogenomics, for instance, helps identify how patients metabolize antihypertensive drugs, optimizing both efficacy and safety. As these tools become more accessible, they promise to elevate the standard of care for high-risk patients.
10. What lessons can be learned from rare cases of extreme hypertension for future public health policy?
Cases involving the highest blood pressure ever recorded offer a unique lens into systemic gaps in healthcare delivery, preventive education, and equitable access. These outliers should not be dismissed as anomalies but rather analyzed for what they reveal about failure points in the system. Policy initiatives could focus on expanding access to preventive screenings, improving medication affordability, and supporting integrated care models that consider mental health and socioeconomic status. Furthermore, data from such cases can inform emergency preparedness protocols and triage guidelines. Ultimately, bridging the gap between individual medical outliers and population-level health strategies is essential for reducing the overall burden of cardiovascular disease.
Conclusion: Lessons from the Highest Blood Pressure Ever Recorded and Moving Toward Better Cardiovascular Health
The extraordinary case of the highest blood pressure ever recorded stands as a medical marvel and a cautionary symbol. While it may capture headlines, its true value lies in what it teaches us about the dangers of unchecked hypertension and the need for proactive, equitable care. For healthcare providers, it underscores the importance of early detection, comprehensive risk assessment, and individualized treatment strategies. For patients, it is a stark reminder of why routine monitoring and lifestyle choices matter.
Ultimately, the road to better cardiovascular health requires collective effort—from clinicians, patients, policymakers, and communities alike. By learning from the most extreme outcomes and committing to sustained, evidence-based care, we can reduce the burden of hypertension and safeguard the health of future generations. The insights gleaned from such rare cases help illuminate the broader path toward prevention, resilience, and a healthier society overall.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.