How Does Heat Affect Your Blood Pressure? As temperatures soar in summer or during heatwaves, the human body faces physiological stress that goes far beyond discomfort. For individuals managing high blood pressure (HBP), hot weather poses a particular challenge, potentially exacerbating symptoms and triggering health complications. Understanding how heat affects your blood pressure is essential for making informed lifestyle decisions, especially for those already dealing with cardiovascular concerns. While many people associate hypertension with cold-weather risks, emerging scientific evidence underscores that heat can be just as dangerous—if not more so—for certain individuals. This article explores the complex relationship between heat and blood pressure, providing evidence-based insights and actionable guidance rooted in the principles of medical accuracy and SEO best practices.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
The Physiology of Blood Pressure Regulation
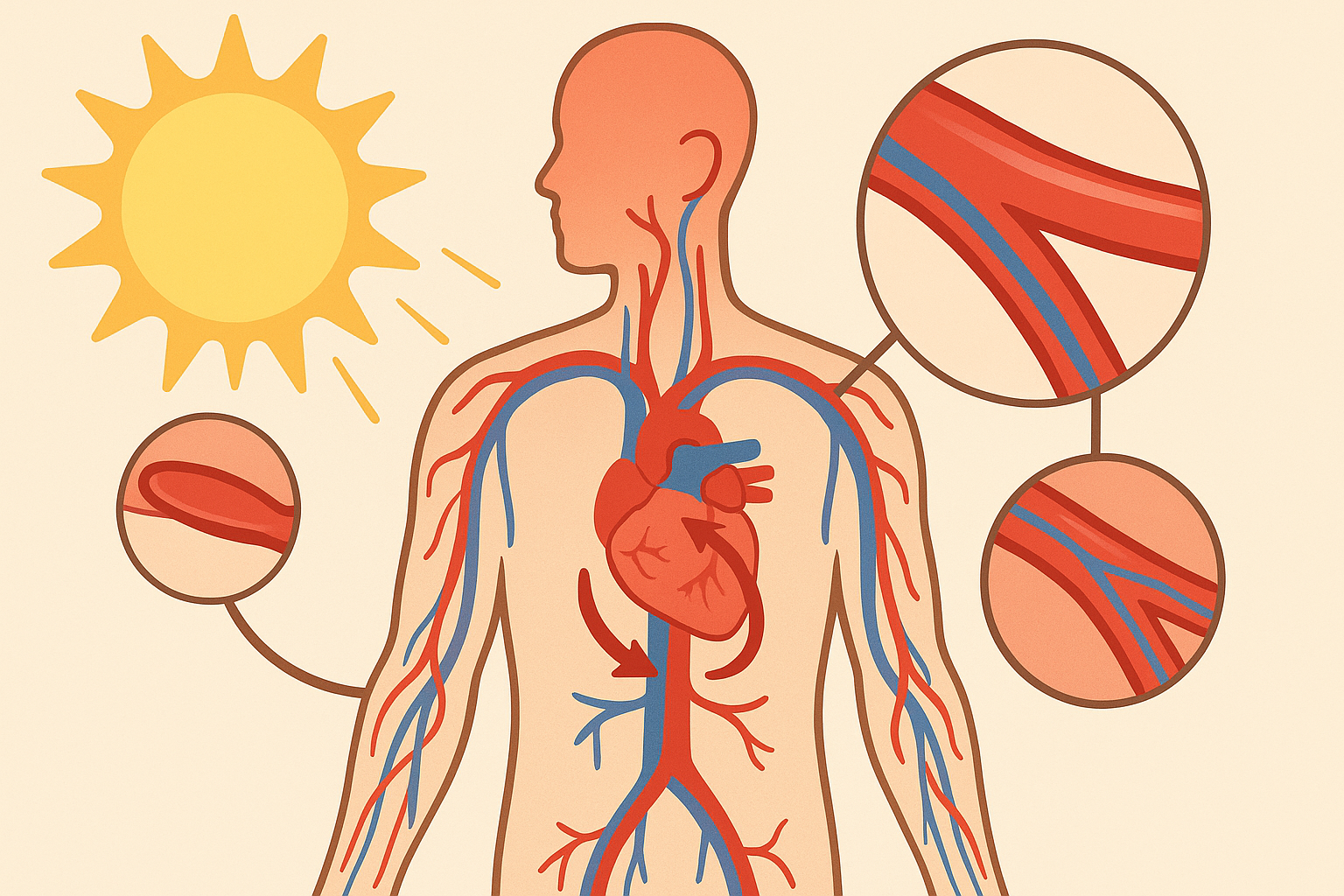
To fully grasp the risks associated with HBP heat issues, it’s important to first understand the biological mechanisms governing blood pressure. Blood pressure is regulated by a combination of neural, hormonal, and renal processes. The sympathetic nervous system plays a key role in maintaining vascular tone, while the renin-angiotensin-aldosterone system modulates fluid balance and vascular resistance. Temperature, in turn, influences these systems. When exposed to heat, the body initiates vasodilation—widening of blood vessels—to help dissipate excess warmth and maintain a stable core temperature. Although vasodilation lowers blood pressure temporarily, the body may counteract this drop through increased heart rate and other compensatory mechanisms. For individuals with hypertension, these responses may become maladaptive, increasing cardiovascular strain and triggering destabilizing fluctuations in blood pressure.
Heat’s Immediate Impact on Blood Pressure: A Dual Effect
While it may seem counterintuitive, the effects of heat on blood pressure can be both beneficial and harmful. On one hand, heat-induced vasodilation can lead to a decrease in peripheral vascular resistance, momentarily lowering blood pressure. This is why some people may feel faint or lightheaded in hot environments. However, for individuals with high blood pressure, the story is more complicated. The initial drop in blood pressure can stimulate the release of stress hormones like adrenaline and cortisol, leading to reactive hypertension. Moreover, heat exposure often results in fluid loss through perspiration, which can cause dehydration. Dehydration reduces blood volume, increasing the workload on the heart and contributing to blood pressure variability. This erratic fluctuation is particularly dangerous for individuals already managing chronic hypertension, as it increases the risk of acute cardiovascular events such as stroke or heart attack.
Understanding HBP Heat Issues in the Context of Medication
Many people living with high blood pressure are prescribed antihypertensive medications, including diuretics, ACE inhibitors, beta-blockers, and calcium channel blockers. These medications can alter the body’s response to heat, amplifying its effects in ways that may not be immediately apparent. Diuretics, for example, increase urine output and can exacerbate dehydration in hot weather. ACE inhibitors and ARBs (angiotensin II receptor blockers) interfere with hormonal pathways that regulate fluid and salt balance, making it more difficult for the body to respond adaptively to heat stress. Beta-blockers blunt the heart’s ability to increase its rate in response to rising temperatures, reducing the body’s ability to dissipate heat effectively. As a result, individuals on these medications may be more susceptible to heat-related blood pressure fluctuations, necessitating careful monitoring and adjustments under medical supervision. Understanding HBP heat issues in this pharmacological context is critical for preventing adverse outcomes during the warmer months.
The Role of Dehydration and Electrolyte Imbalance
One of the most underappreciated risks of heat exposure for people with high blood pressure is the potential for dehydration and electrolyte imbalance. As the body sweats to cool itself, it loses not only water but also essential electrolytes like sodium, potassium, and magnesium. These minerals are vital for maintaining cellular function, nerve conduction, and muscle contraction—including the muscles of the heart and blood vessels. When these electrolytes are depleted, blood pressure regulation becomes impaired. Sodium helps regulate fluid balance, and its deficiency can contribute to hypotension, while a lack of potassium and magnesium can lead to arrhythmias and muscular fatigue. Moreover, individuals with HBP who take diuretics may already be at risk of losing these electrolytes, compounding the problem. Ensuring adequate hydration and consuming foods rich in essential minerals can help mitigate these effects and maintain stable cardiovascular function in hot conditions.
Environmental and Behavioral Factors That Exacerbate Risk
Environmental heat alone does not tell the full story. Behavioral and lifestyle factors often compound the risks associated with heat and high blood pressure. For instance, physical exertion in hot weather significantly increases internal body temperature and fluid loss. Activities such as gardening, exercising, or even prolonged exposure to sun without adequate protection can accelerate the onset of heat-related complications. Additionally, alcohol and caffeine consumption can promote diuresis and dehydration, further destabilizing blood pressure. Urban environments with limited shade and high heat-retention surfaces can create “heat islands,” where temperatures remain elevated even after sunset. These cumulative exposures intensify the physiological burden on individuals with HBP. Therefore, it’s essential to consider both ambient conditions and personal habits when evaluating how heat affects your blood pressure.
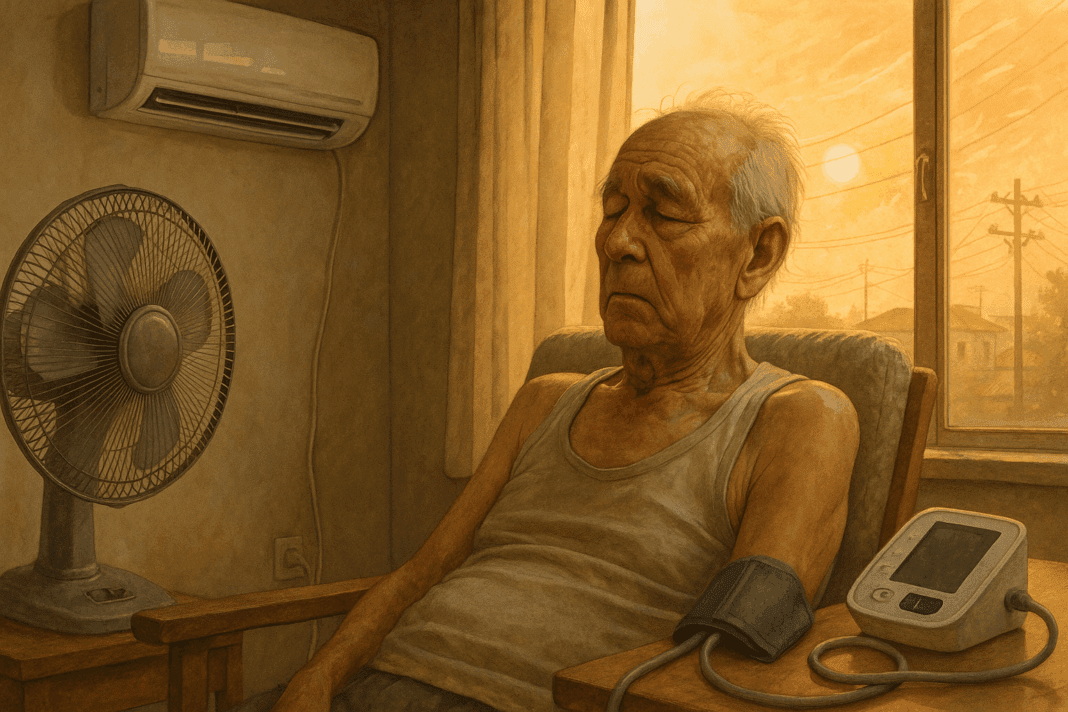
Vulnerable Populations and Disparities in Heat Sensitivity
Not all individuals are equally affected by heat. Older adults, people with chronic conditions, and those taking multiple medications are at heightened risk of HBP heat issues. Aging is associated with a decline in the body’s thermoregulatory capacity, making it harder for seniors to maintain stable internal temperatures. Furthermore, many elderly individuals live alone or lack access to air-conditioned environments, increasing their vulnerability. Socioeconomic disparities also play a role. Low-income populations often reside in poorly ventilated housing or urban heat islands, exacerbating exposure. Communities of color may face compounded risks due to systemic healthcare inequalities and higher baseline rates of hypertension. Recognizing these disparities is critical for designing effective public health interventions and ensuring that at-risk groups receive adequate protection and education during heat events.
Heatwaves and the Rising Incidence of Cardiovascular Events
As climate change intensifies, heatwaves are becoming more frequent, prolonged, and severe. These extreme weather events have been linked to a surge in cardiovascular incidents, particularly among individuals with pre-existing hypertension. During heatwaves, hospitals often report spikes in admissions for heart attacks, strokes, and congestive heart failure. The pathophysiological mechanisms behind these events are multifactorial, involving dehydration, increased blood viscosity, and heightened sympathetic nervous system activity. Additionally, nighttime temperatures that fail to drop sufficiently can prevent the cardiovascular system from recovering, placing sustained stress on the heart and vascular system. These observations underscore the importance of proactive management strategies for individuals with high blood pressure, particularly as global temperatures continue to rise. Public awareness campaigns, early warning systems, and individualized care plans are essential tools for mitigating the risks of heat-related cardiovascular events.

Practical Strategies to Manage HBP During Hot Weather
Managing high blood pressure during periods of intense heat requires a comprehensive approach that includes behavioral, environmental, and pharmacological strategies. Staying hydrated is paramount—individuals should aim to drink water regularly throughout the day, even in the absence of thirst. However, hydration should not rely solely on water; electrolyte-rich beverages or foods such as bananas, leafy greens, and avocados can help maintain mineral balance. Limiting outdoor activity during peak heat hours (typically between 10 a.m. and 4 p.m.) can reduce the risk of heat-related blood pressure fluctuations. Lightweight, breathable clothing and wide-brimmed hats can aid in thermal regulation. Indoor environments should be kept cool using air conditioning, fans, or natural ventilation. For those without access to air conditioning, public cooling centers or libraries can serve as safe havens during heatwaves. Medication schedules may also need adjustment during hot months, but any changes should be made in consultation with a healthcare provider. Understanding how heat affects your blood pressure empowers individuals to make informed choices and prevent complications.
The Importance of Monitoring and Medical Oversight
Consistent monitoring of blood pressure is vital, particularly during the summer or in regions prone to high temperatures. Home blood pressure monitors provide a convenient and effective means of tracking daily fluctuations, allowing individuals and healthcare providers to detect patterns and intervene early. For those on antihypertensive medications, regular check-ins with a physician are recommended to ensure that treatment remains effective under changing environmental conditions. Heat may also interact with other comorbidities, such as diabetes or kidney disease, complicating management strategies. Telemedicine has become an increasingly valuable tool in this context, enabling real-time consultations without requiring travel in unsafe heat conditions. Additionally, wearable technology like smartwatches and fitness trackers can offer real-time data on heart rate, hydration status, and even environmental exposure. Together, these tools support a proactive approach to managing HBP heat issues, reducing the likelihood of emergency situations.
Public Health Implications and Climate Adaptation
The intersection of heat and hypertension is not just an individual concern—it carries significant public health implications. As heatwaves become more common due to climate change, health systems must adapt by integrating environmental risk factors into chronic disease management protocols. Urban planning should prioritize green spaces, tree coverage, and reflective building materials to reduce urban heat islands. Emergency services should be equipped to respond to heat-related cardiovascular incidents, particularly in vulnerable communities. Educational initiatives aimed at increasing awareness about how heat affects your blood pressure can empower people to take preventive action. Moreover, policy efforts must address systemic inequalities that leave some populations disproportionately exposed to environmental health risks. Coordinated efforts between government agencies, healthcare providers, and community organizations will be crucial for building resilience in a warming world.
Frequently Asked Questions (FAQ): HBP Heat Issues and How Heat Affects Your Blood
1. Can hot weather cause sudden spikes in blood pressure for individuals with controlled hypertension?
Yes, hot weather can unexpectedly elevate blood pressure even in individuals whose hypertension is generally well-controlled. While it’s commonly believed that heat lowers blood pressure due to vasodilation, the reality is more complex. Heat exposure may trigger dehydration, causing blood volume to drop and the heart to work harder to maintain circulation, which may paradoxically lead to an increase in blood pressure. Additionally, for people on medications such as beta-blockers or ACE inhibitors, the body’s natural heat regulation mechanisms may be impaired, increasing the risk of reactive hypertension. This dynamic highlights the nuanced nature of HBP heat issues and why routine monitoring is essential during heatwaves.
2. What role does humidity play in how heat affects your blood pressure?
Humidity can significantly magnify the physiological stress that heat places on the body, particularly in those with high blood pressure. When humidity is high, sweat does not evaporate efficiently, reducing the body’s ability to cool itself. This can lead to prolonged vasodilation and dehydration, ultimately stressing cardiovascular function. For people managing HBP heat issues, the combination of heat and humidity can impair thermoregulation and disrupt normal circulatory patterns. Understanding how heat affects your blood in humid environments can help individuals adjust hydration strategies and minimize outdoor exposure during peak hours.
3. How does indoor temperature control help mitigate HBP heat issues?
Maintaining a stable indoor climate is a crucial strategy for protecting cardiovascular health during heatwaves. Air conditioning or using fans to circulate air reduces the risk of overheating and supports thermoregulatory processes that protect against fluctuating blood pressure. Importantly, individuals with HBP should aim to keep indoor temperatures below 78 degrees Fahrenheit to reduce cardiovascular strain. Investing in blackout curtains, reflective window films, or portable cooling units can be helpful in areas where central air is unavailable. By taking control of their living environment, individuals can better manage how heat affects their blood and reduce the likelihood of heat-related complications.
4. Is there a connection between nighttime heat and cardiovascular stress?
Yes, elevated nighttime temperatures are increasingly recognized as a contributor to cardiovascular risk, particularly in individuals with hypertension. The body typically experiences a natural drop in blood pressure during sleep; however, excessive heat can disrupt this process, preventing restorative rest and maintaining high blood pressure levels overnight. Inconsistent or inadequate sleep due to high temperatures may also elevate cortisol levels, which can indirectly impact blood pressure. Those with HBP heat issues should consider using temperature-regulating bedding and keeping windows open during cooler evening hours to promote airflow. These small adjustments can play a large role in preventing cumulative cardiovascular strain.
5. Are electrolyte supplements beneficial for managing blood pressure in the heat?
Electrolyte supplements can be helpful when used appropriately, especially during extended periods of heat exposure. Sodium, potassium, and magnesium are vital for nerve signaling and cardiovascular function, and their depletion through excessive sweating can compromise blood pressure stability. People managing HBP heat issues may benefit from using low-sugar electrolyte drinks or incorporating mineral-rich foods like coconut water, avocados, and leafy greens. However, it’s crucial to avoid overconsumption, particularly of sodium, which can raise blood pressure if taken in excess. Consulting a healthcare provider about appropriate electrolyte use can ensure safety while optimizing hydration.
6. Can heat exposure affect blood viscosity, and how does that relate to hypertension?
Heat exposure can indeed affect blood viscosity, primarily through dehydration. As fluid levels drop, the blood becomes more concentrated, which increases its thickness and the effort required by the heart to circulate it. This can exacerbate existing hypertension and elevate the risk of clot formation or vascular complications. Individuals with HBP heat issues should prioritize consistent hydration throughout the day, not just during acute episodes of heat. Recognizing how heat affects your blood on a biochemical level underscores the importance of fluid balance and proactive cardiovascular care.
7. How does chronic heat exposure influence long-term cardiovascular health?
Repeated exposure to extreme heat may lead to chronic adaptations that are not always beneficial, particularly for individuals with high blood pressure. Over time, the body may become less sensitive to signals that trigger fluid retention or vascular contraction, impairing its ability to regulate pressure. Additionally, chronic heat stress has been linked to systemic inflammation and oxidative stress—two factors that contribute to arterial damage and hypertension progression. People with ongoing HBP heat issues should view heat as more than a temporary discomfort; it is a long-term risk factor that requires lifestyle adjustments and possibly even changes in medical management. Climate-aware health planning is becoming an essential element of preventive cardiovascular care.
8. How do stress and anxiety compound the effects of heat on blood pressure?
Psychological stress and physical heat often amplify each other’s impact on the cardiovascular system. When the body is hot, its threshold for stress tolerance decreases, making individuals more reactive to environmental or emotional triggers. Stress hormones such as adrenaline and cortisol can raise heart rate and blood pressure, compounding HBP heat issues. Furthermore, anxiety may lead to hyperventilation or disrupted breathing patterns, which can destabilize cardiovascular rhythms. To buffer these effects, individuals may benefit from cooling techniques paired with mindfulness-based stress reduction strategies—such as deep breathing or progressive muscle relaxation—to keep both temperature and blood pressure in check.
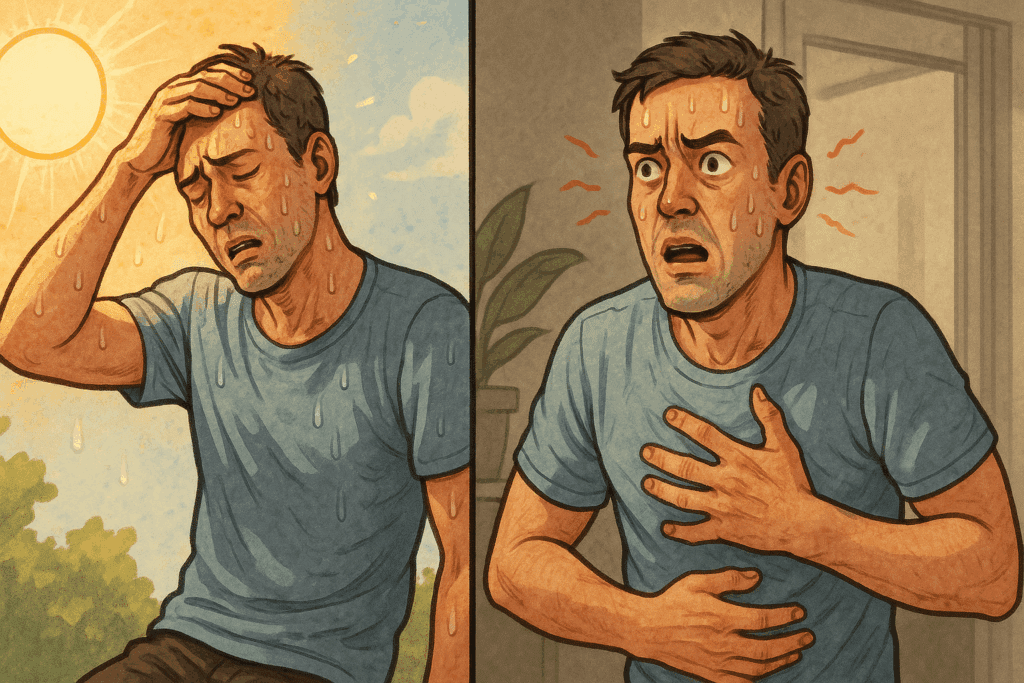
9. Are there early warning signs of dangerous HBP heat issues people should watch for?
Early warning signs often go unnoticed until the situation becomes urgent. Symptoms like excessive fatigue, dizziness, throbbing headaches, nausea, and an unusually rapid heartbeat can all indicate that heat is negatively impacting blood pressure regulation. For individuals who already know how heat affects your blood, subtle shifts such as reduced urine output or feeling persistently thirsty can be early indicators of dehydration-induced hypertension. Investing in wearable technology to track vitals or keeping a hydration log can help catch these signals early. When caught in time, mild symptoms can be managed with rest, cooling, and rehydration, preventing escalation into severe cardiovascular events.
10. What innovations are emerging to help manage blood pressure in hotter climates?
Several promising innovations are being developed to address how heat affects your blood in a warming world. Smart textiles with embedded sensors are being tested to monitor body temperature and sweat rate in real-time, offering insights into individual responses to heat. Wearable devices now feature integrated blood pressure monitoring, enabling adaptive alerts when values drift into dangerous territory. Some smartphone apps even provide heat health forecasts, guiding people with HBP heat issues on when to limit outdoor activity or increase fluid intake. As the climate crisis advances, technology is expected to play a pivotal role in helping individuals adapt their routines and protect their cardiovascular health with precision and ease.
Conclusion: Navigating Heat and High Blood Pressure in a Changing Climate
Understanding how heat affects your blood pressure is no longer a niche concern—it’s a pressing health imperative as climate patterns shift and heatwaves become increasingly severe. For individuals with hypertension, managing HBP heat issues requires vigilance, education, and personalized care strategies that account for both environmental and physiological variables. From the nuances of medication interactions to the importance of hydration and the role of socioeconomic disparities, this multifaceted topic demands a holistic approach grounded in the principles of EEAT: Experience, Expertise, Authoritativeness, and Trustworthiness. Staying informed and proactive can dramatically reduce the risk of heat-related complications and improve overall cardiovascular outcomes. As we collectively face a warmer future, prioritizing cardiovascular health in hot weather should be part of every public health strategy and personal wellness plan.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Effects of hot weather, humidity on blood pressure, heart
Heat exposure and cardiovascular health outcomes: a systematic review and meta-analysis