Hypertension, often referred to as high blood pressure, is a leading risk factor for cardiovascular disease worldwide. Its silent progression can quietly damage arteries and organs over time, making early recognition and management crucial for long-term health. The condition is not uniform; instead, it is classified into stages that reflect the severity of blood pressure elevation and its potential impact on health. For patients and clinicians alike, understanding the four stages of hypertension is essential for early intervention, informed decision-making, and proactive risk reduction. This article delves deeply into the medical definitions, clinical implications, and prognosis associated with each stage, including stage 2 hypertension and grade 3 hypertension, while addressing frequently asked questions such as how many stages of hypertension is there and what the term “500 blood pressure” might mean in a clinical context.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Defining Blood Pressure and Hypertension
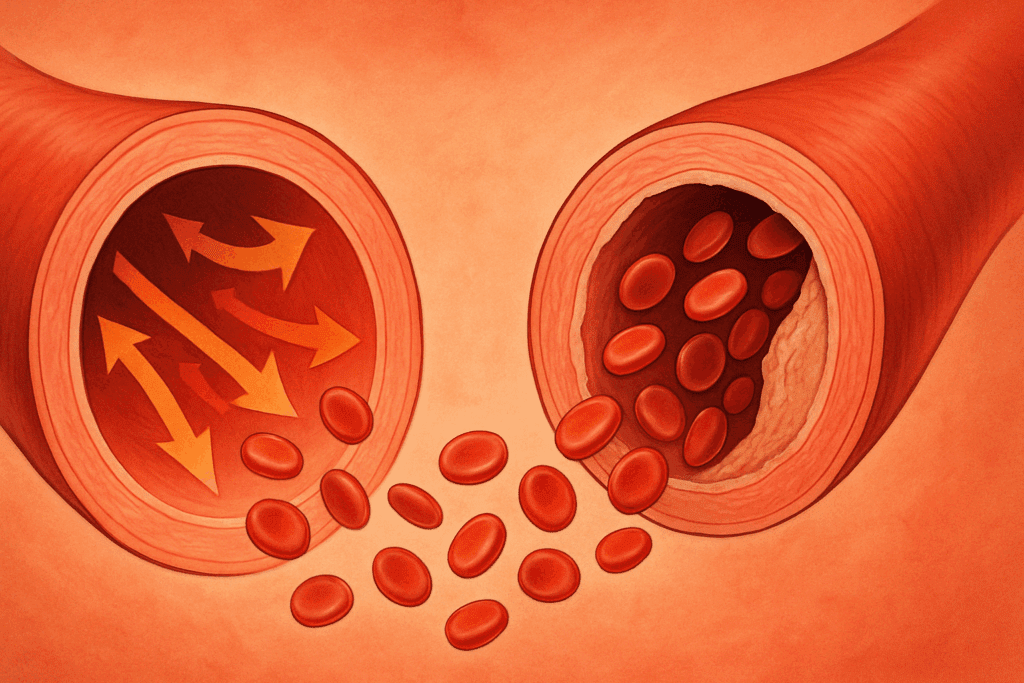
Blood pressure is the force exerted by circulating blood against the walls of the body’s arteries, the major blood vessels in the body. It is recorded as two numbers: systolic pressure (the pressure when the heart beats) over diastolic pressure (the pressure when the heart rests between beats). Normal blood pressure is typically considered to be less than 120/80 mm Hg. When blood pressure remains consistently elevated, the condition is classified as hypertension.
Hypertension is diagnosed when an individual’s blood pressure readings consistently fall outside the normal range. It is often dubbed the “silent killer” because it may not present noticeable symptoms until significant damage has occurred. If left untreated, high blood pressure can lead to heart attack, stroke, kidney disease, and other serious health problems. Understanding the nuances of the four stages of hypertension allows for better prevention strategies and targeted treatment.
How Many Stages of Hypertension Is There?
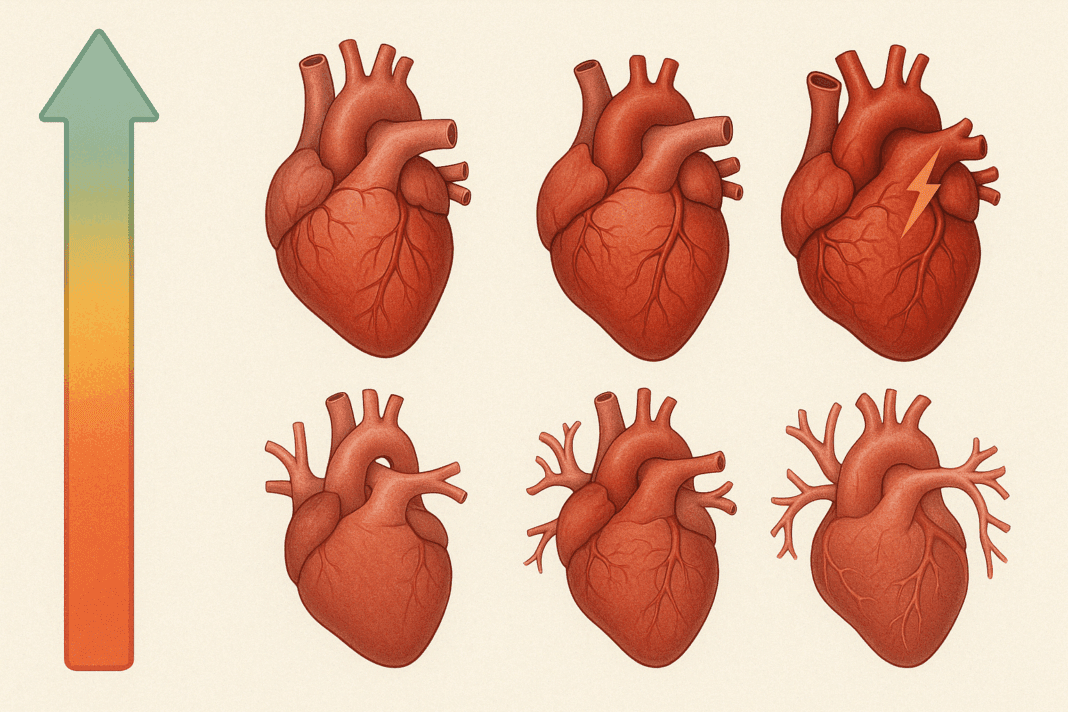
A common question patients ask is: how many stages of hypertension is there? The answer lies in clinical guidelines published by organizations such as the American Heart Association and the World Health Organization. Typically, hypertension is divided into four stages: normal blood pressure, elevated blood pressure, stage 1 hypertension, and stage 2 hypertension. Some countries and health authorities may use slightly different terminology, such as “grade 3 hypertension,” but the fundamental classifications are based on the same principles.
Each stage reflects a progressive elevation in systolic and/or diastolic pressure and an associated increase in cardiovascular risk. Recognizing where an individual falls on this spectrum allows clinicians to tailor interventions that are both preventative and therapeutic. From lifestyle changes to pharmacologic treatments, management strategies vary by stage and are grounded in evidence-based practices.

Normal and Elevated Blood Pressure: The Pre-Hypertensive Spectrum
Before hypertension officially begins, there are ranges considered normal or elevated. A blood pressure reading of less than 120/80 mm Hg is classified as normal. These individuals are considered at low risk for cardiovascular disease, though other risk factors such as age, family history, or lifestyle may still warrant attention. Maintaining a healthy diet, engaging in regular physical activity, limiting sodium intake, and managing stress are essential even at this stage.
Elevated blood pressure is defined as systolic pressure between 120-129 mm Hg with a diastolic pressure less than 80 mm Hg. Though not officially classified as hypertension, this stage signals increased risk. At this point, physicians typically recommend lifestyle modifications to prevent progression. The distinction between elevated blood pressure and stage 1 hypertension is subtle yet significant, as even marginal increases in pressure can accelerate vascular aging and end-organ damage.
Stage 1 Hypertension: The Beginning of Clinical Concern
Stage 1 hypertension is diagnosed when systolic pressure ranges from 130 to 139 mm Hg or diastolic pressure ranges from 80 to 89 mm Hg. This is the first level where clinicians begin to consider pharmacologic intervention, particularly if the patient has additional risk factors such as diabetes, chronic kidney disease, or a history of cardiovascular events.
The prognosis for individuals in this stage varies depending on how quickly and effectively blood pressure is controlled. If lifestyle changes such as dietary improvements, weight loss, and physical activity are implemented promptly, many individuals can return to a lower-risk category without the need for medication. Nevertheless, stage 1 hypertension is a wake-up call, indicating that vascular resistance is increasing and that early damage may already be underway.
Stage 2 Hypertension Prognosis and Management
Stage 2 hypertension is defined by a systolic reading of 140 mm Hg or higher or a diastolic reading of 90 mm Hg or higher. At this level, the condition poses a significant risk for heart attack, stroke, and other cardiovascular complications. The stage 2 hypertension prognosis depends heavily on how soon treatment is initiated and how aggressively it is managed.
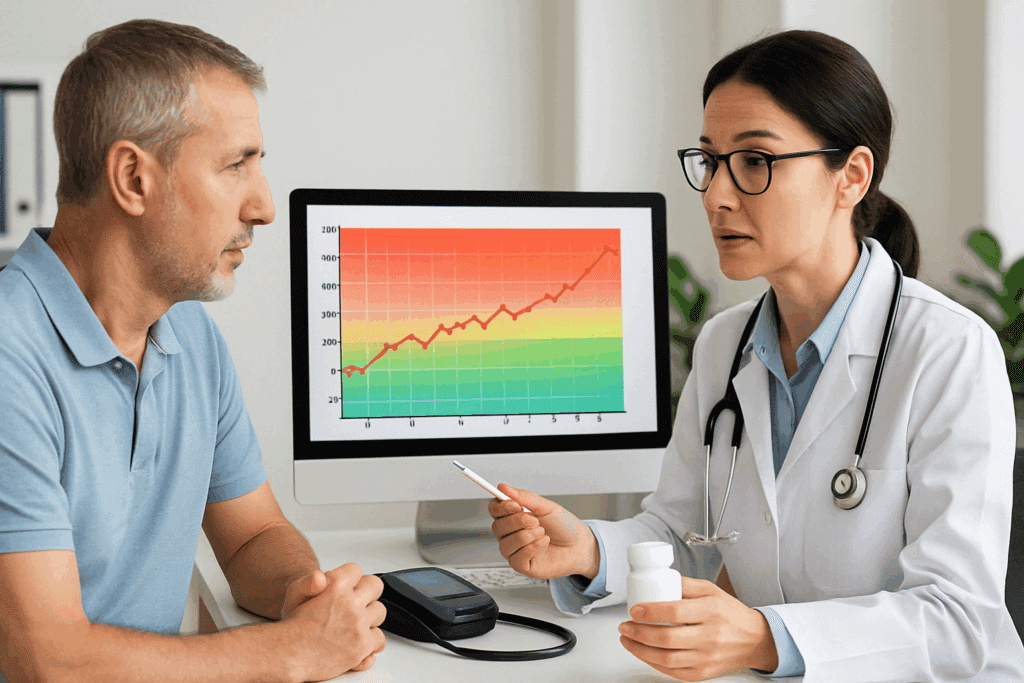
For most individuals, stage 2 hypertension requires a combination of medications to achieve target blood pressure levels. Common drug classes include ACE inhibitors, calcium channel blockers, diuretics, and beta-blockers. Importantly, medication must be paired with sustained lifestyle modifications to ensure optimal outcomes. Patients are advised to monitor their blood pressure regularly, adhere strictly to prescribed treatments, and undergo periodic evaluations to assess progress and adjust therapy.
While some individuals can achieve adequate control within a few months, others may require long-term medication and monitoring. The key to improving stage 2 hypertension prognosis lies in patient education, adherence, and a collaborative care model involving primary care providers, cardiologists, dietitians, and sometimes behavioral health professionals.
Grade 3 Hypertension: Severe and Urgent Risk
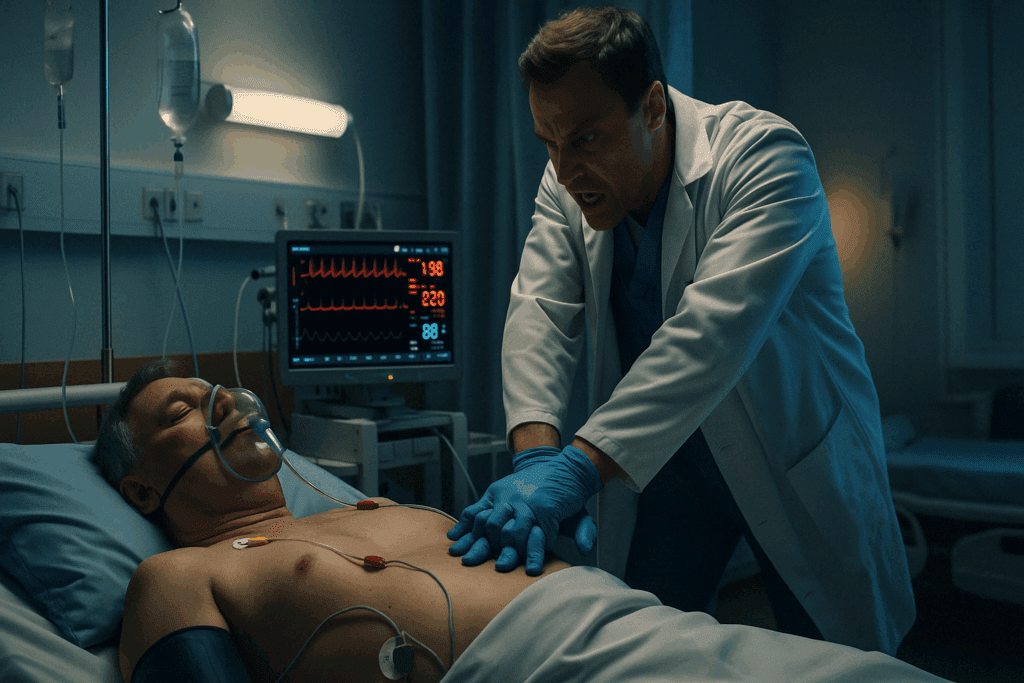
In certain international classification systems, particularly those used in Europe, stage 2 hypertension is further subdivided to identify those with the most severe elevations in blood pressure. Grade 3 hypertension refers to a systolic reading of 180 mm Hg or higher and/or a diastolic reading of 110 mm Hg or higher. At this point, the risk of acute cardiovascular events becomes exceedingly high, and immediate medical intervention is critical.
Grade 3 hypertension is often associated with end-organ damage, which may include left ventricular hypertrophy, retinal changes, kidney impairment, or cerebrovascular abnormalities. Symptoms such as headaches, visual disturbances, or chest pain may occur, indicating a hypertensive crisis. Hospitalization and intravenous medications may be necessary in these cases to reduce blood pressure safely and prevent further harm.
Long-term management focuses on aggressive blood pressure control, often with multiple medications and frequent follow-up. Patients must be monitored for complications, and lifestyle changes become not just advisable but essential. For many, grade 3 hypertension represents a turning point—one that underscores the need for ongoing vigilance and strict adherence to treatment protocols.
Understanding “500 Blood Pressure”: Clinical Interpretation and Urgency
The phrase “500 blood pressure” may sound hyperbolic, but it sometimes surfaces in anecdotal discussions, emergency room scenarios, or as a dramatized reference to extreme hypertensive crises. Clinically, a blood pressure reading approaching or exceeding 250/150 mm Hg is already considered life-threatening. A “500 blood pressure” would not be physiologically compatible with life, as such extreme pressures would likely result in immediate vascular rupture, stroke, or cardiac arrest.
Still, the expression serves as a powerful reminder of how dangerously high blood pressure can rise in untreated or poorly managed cases. Patients presenting with extremely elevated readings often have underlying conditions such as pheochromocytoma, renal artery stenosis, or severe medication noncompliance. These scenarios require immediate intervention, often in an intensive care setting, with continuous monitoring and rapid-acting intravenous drugs.
The takeaway for patients and clinicians is that uncontrolled hypertension can escalate quickly, and regular monitoring is essential to catch dangerous trends before they lead to irreversible damage. It also emphasizes the importance of patient education in recognizing warning signs and seeking help before a hypertensive emergency arises.

How Many Stages of Blood Pressure Are There: A Reiteration of Risk Stratification
When asking how many stages of blood pressure are there, it’s essential to view blood pressure not just as numbers but as indicators of vascular health. As noted earlier, the four stages—normal, elevated, stage 1 hypertension, and stage 2 hypertension—provide a framework for risk stratification. However, the clinical journey does not stop there. Within each stage, individual variability in risk is influenced by comorbidities, genetics, lifestyle, and adherence to therapy.
In addition to the basic stages, clinicians often consider hypertensive urgency and emergency as separate clinical entities. Hypertensive urgency refers to severely elevated blood pressure without signs of end-organ damage, whereas hypertensive emergency includes symptoms and evidence of acute damage. These classifications underscore the dynamic nature of blood pressure and the need for nuanced clinical judgment.
Ultimately, categorizing blood pressure into stages allows for targeted, evidence-based interventions. It also empowers patients to understand their condition, engage with their care plan, and take proactive steps to protect their cardiovascular health.
The Role of Lifestyle in Managing Hypertension Across All Stages
Regardless of stage, lifestyle factors play a crucial role in both the development and management of hypertension. Diet, exercise, stress management, and substance use can all influence blood pressure levels. The DASH (Dietary Approaches to Stop Hypertension) diet, for instance, has been proven to lower blood pressure through increased consumption of fruits, vegetables, lean proteins, and low-fat dairy, while limiting saturated fats and sodium.
Regular aerobic activity, such as brisk walking, swimming, or cycling, has been shown to reduce systolic blood pressure by an average of 5 to 10 mm Hg in many individuals. Stress-reduction techniques such as mindfulness meditation, yoga, and biofeedback also contribute to improved cardiovascular outcomes. Smoking cessation and limiting alcohol intake further amplify the benefits of other interventions.
Patients often underestimate the power of consistent lifestyle choices, but these changes can yield significant improvements, particularly in the earlier stages of hypertension. Even in stage 2 or grade 3 hypertension, lifestyle optimization remains a cornerstone of care, enhancing the effectiveness of medication and reducing long-term risk.
Patient Education and Long-Term Prognosis
Effective management of hypertension depends not only on clinical interventions but also on patient understanding and engagement. Education about the stages of hypertension, potential complications, and the rationale for treatment empowers individuals to take ownership of their health. Tools such as home blood pressure monitors, medication reminders, and mobile health apps can support adherence and promote regular self-assessment.
Patients should also be counseled on the importance of regular check-ups, laboratory evaluations, and screenings for associated conditions such as dyslipidemia, diabetes, and kidney disease. A team-based approach that includes physicians, nurses, pharmacists, dietitians, and behavioral health professionals can help address the multifaceted nature of hypertension and improve long-term outcomes.
Prognosis varies by stage but is strongly influenced by how quickly and effectively blood pressure is controlled. For many individuals, early detection and intervention can significantly reduce the risk of cardiovascular events and improve quality of life. Even those with advanced disease can achieve meaningful improvements through comprehensive, multidisciplinary care.
Frequently Asked Questions: Advanced Insights on Hypertension and Cardiovascular Risk
What makes early detection of stage 1 hypertension critical even if symptoms aren’t present?
Many individuals underestimate the implications of early-stage hypertension simply because they feel fine. However, even in the absence of symptoms, elevated blood pressure can initiate subtle damage to blood vessels, the heart, and kidneys. Early intervention in stage 1 offers the best chance to reverse or control the condition before it progresses to the more serious stages. Recognizing where one falls within the four stages of hypertension helps inform preventative strategies that might include targeted lifestyle adjustments or minimal pharmacological support. The longer stage 1 goes unnoticed or untreated, the greater the likelihood that the condition will escalate toward stage 2, which has a less favorable prognosis.
How does stress influence progression across the four stages of hypertension?
Chronic stress doesn’t just impact mood—it can have measurable physiological effects that worsen blood pressure. Elevated cortisol and adrenaline levels from prolonged stress may contribute to endothelial dysfunction, vascular constriction, and increased heart rate. These responses can drive an individual from elevated blood pressure into stage 1 hypertension and beyond. While stress alone may not explain how many stages of hypertension is there, it is a powerful modifier of risk across all stages. Developing coping mechanisms—like cognitive behavioral therapy or structured relaxation techniques—can be a vital part of long-term blood pressure management.
What does a hypertensive crisis look like, and how does it relate to the term ‘500 blood pressure’?
While the phrase “500 blood pressure” is not a clinically recognized value, it has become a colloquial expression for extremely dangerous hypertensive states. In real-world terms, readings above 180/120 mm Hg can signal a hypertensive emergency, often involving organ damage. Patients experiencing symptoms like chest pain, confusion, or vision changes in such a context need immediate medical attention. Though 500 blood pressure isn’t physiologically survivable, its frequent mention underlines the importance of recognizing the signs of grade 3 hypertension before a true crisis occurs. These emergencies often stem from untreated or undiagnosed late-stage hypertension and highlight the urgency of consistent monitoring.
How does stage 2 hypertension prognosis differ for younger versus older adults?
Age can significantly shape the trajectory of stage 2 hypertension prognosis. In younger adults, early diagnosis followed by aggressive management can often normalize blood pressure within months or years, potentially preventing long-term complications. In contrast, older adults often present with co-existing conditions such as atherosclerosis or diabetes, which complicate treatment and worsen outcomes. Lifestyle flexibility and physiological resilience tend to favor younger individuals, while older patients may require more nuanced medication regimens. Regardless of age, however, understanding the four stages of hypertension allows healthcare providers to tailor interventions that consider both chronological and biological age.
Can medication alone effectively manage grade 3 hypertension, or is lifestyle modification still essential?
Medication is indispensable in treating grade 3 hypertension due to its severe and immediate risks. However, relying solely on pharmaceuticals without addressing root causes—such as obesity, sedentary behavior, and high sodium intake—can limit the long-term effectiveness of treatment. Many patients find that medication brings their numbers down temporarily, but sustained improvement is more likely when combined with dietary changes, increased physical activity, and stress reduction. Longitudinal studies suggest that lifestyle modification enhances medication efficacy, lowers the required dosage over time, and reduces the likelihood of relapse. This synergy is especially crucial in the more dangerous stages, where prognosis hinges on comprehensive management.
How many stages of blood pressure are there, and can someone fluctuate between them frequently?
Clinically, when asking how many stages of blood pressure are there, four primary categories are commonly used: normal, elevated, stage 1 hypertension, and stage 2 hypertension. However, fluctuations are not uncommon—especially in people with stress sensitivity, inconsistent medication adherence, or erratic dietary habits. For example, a person might test as stage 1 in a high-stress environment but return to elevated or even normal levels under relaxed conditions. Ambulatory blood pressure monitoring over 24 hours can help clarify where someone consistently falls within the four stages of hypertension. These fluctuations are important to track, as repeated transitions into higher stages can accelerate vascular damage and complicate treatment planning.
How can wearable technology improve outcomes in people with stage 2 hypertension?
Emerging technologies like smartwatches and at-home monitoring devices are changing how we approach hypertension management. For those with stage 2 hypertension, real-time feedback from wearables can encourage medication adherence, reinforce healthy behaviors, and alert users to concerning spikes. These tools also facilitate more accurate conversations between patients and providers by offering longitudinal data rather than isolated clinic readings. By understanding how many stages of hypertension is there, users can contextualize their numbers and use alerts as a prompt for proactive interventions. This personalized approach empowers patients, especially those with a stage 2 hypertension prognosis, to take daily control of their cardiovascular risk profile.
Are there gender-specific differences in hypertension progression, particularly toward grade 3 hypertension?
Research has shown that men and women may experience different patterns of blood pressure elevation and response to treatment. For example, premenopausal women generally have lower hypertension rates, but postmenopausal women may experience more rapid progression to stage 2 or grade 3 hypertension due to hormonal shifts. Additionally, some antihypertensive medications may be metabolized differently by gender, influencing efficacy. Understanding these distinctions is vital when navigating the four stages of hypertension, as women may be underdiagnosed or misclassified if gender-based differences are not accounted for. Clinicians who personalize their approach based on sex-specific trends may see improved outcomes, particularly in cases with a poor stage 2 hypertension prognosis.
Is it possible to reverse stage 1 or stage 2 hypertension without medication?
For many patients in the earlier stages, particularly stage 1, non-pharmacologic interventions can lead to normalization of blood pressure. These include weight loss, reduced sodium intake, increased potassium consumption, regular physical activity, and stress management. Even stage 2 hypertension prognosis can improve markedly when lifestyle changes are implemented diligently, although medication is usually recommended as part of an initial strategy. The body’s response varies widely, but the underlying principle is that the earlier the intervention, the greater the likelihood of reversal. Tracking progress over time with a clear understanding of how many stages of blood pressure are there helps patients and providers evaluate treatment effectiveness and make informed adjustments.
Why do some individuals remain asymptomatic even with dangerously high readings like grade 3 hypertension?
The absence of symptoms in severe cases is a known and troubling aspect of hypertension. The vascular system can adapt gradually to rising pressure, masking the damage that is accumulating internally. This means a person could live with grade 3 hypertension and still feel relatively normal—until a stroke or heart attack reveals the hidden toll. This silent nature is one reason clinicians stress routine monitoring, particularly for those with risk factors like family history or obesity. Misunderstandings around terms like “500 blood pressure” sometimes stem from this paradox, as people assume they would “feel” unwell if they were truly in danger. Unfortunately, that is not always the case—hence the importance of vigilance and regular health checks.
Reflecting on the Four Stages of Hypertension and Their Impact on Heart Health
Understanding the four stages of hypertension is more than an academic exercise—it is a practical tool for guiding clinical care and empowering patients. From elevated blood pressure to grade 3 hypertension, each stage presents a unique set of challenges and opportunities for intervention. Whether patients are just beginning to see rising numbers or are already navigating the complexities of stage 2 hypertension prognosis, the key to success lies in early detection, consistent management, and a holistic approach to cardiovascular health.
By addressing the question of how many stages of hypertension is there and elucidating what these classifications mean in real-world terms, we offer a roadmap for managing a condition that affects millions globally. From debunking myths surrounding “500 blood pressure” to contextualizing the urgency of grade 3 hypertension, this article has aimed to inform, engage, and empower. Hypertension need not be a silent killer if we approach it with vigilance, education, and an unwavering commitment to heart health.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
What Are the Stages of Hypertension?