Blood pressure is one of the most fundamental indicators of cardiovascular health, yet its regulation remains a complex interplay of numerous physiological mechanisms. Among these, vasoconstriction plays a central role in determining how blood flows through the body. When blood vessels narrow—a process known as vasoconstriction—the dynamics of pressure, circulation, and overall heart function change significantly. Understanding how vasoconstriction affects the cardiovascular system is not only essential for managing hypertension and related conditions, but also for recognizing how a constricted artery might signal deeper systemic concerns. This article offers an in-depth, evidence-based exploration of how vasoconstriction influences blood pressure and what it may mean for long-term cardiovascular risk.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
The Physiology of Vasoconstriction and Blood Flow Regulation
Vasoconstriction is the narrowing of blood vessels resulting from the contraction of the muscular wall of the vessels, particularly in arteries and arterioles. This physiological response can be triggered by a range of stimuli, including sympathetic nervous system activation, hormonal signals like epinephrine and norepinephrine, and certain pharmacological agents. From an evolutionary perspective, vasoconstriction serves critical functions such as preserving core body temperature and redirecting blood flow to vital organs during periods of stress or danger. However, when vasoconstriction becomes chronic or inappropriately regulated, it may contribute to increased blood pressure and heightened cardiovascular risk.
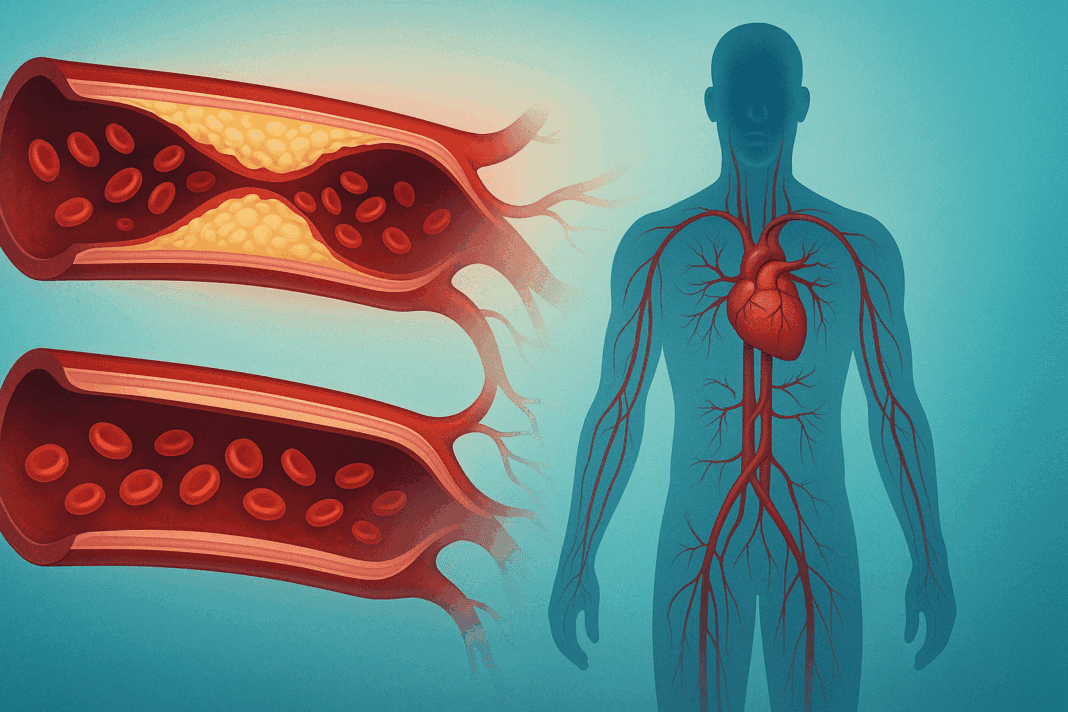
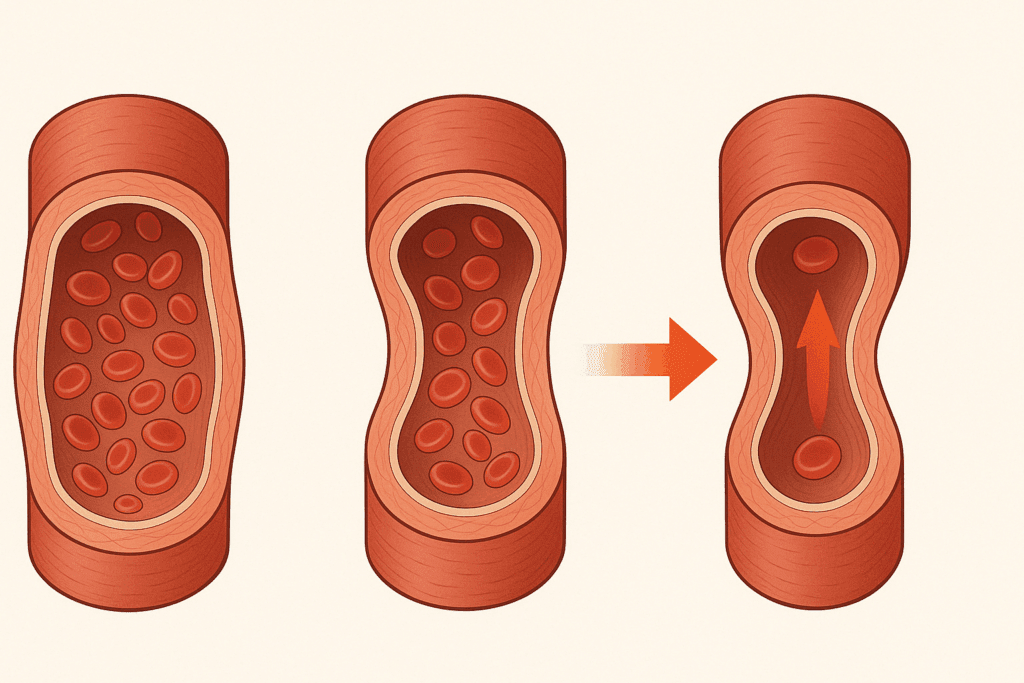
The relationship between vasoconstriction and blood pressure is inherently mechanical. When blood vessels constrict, the lumen—or inner diameter—of the arteries becomes smaller, which increases resistance to blood flow. According to Poiseuille’s law, resistance is inversely proportional to the fourth power of the radius, meaning even minor reductions in arterial diameter can produce significant increases in resistance. Consequently, to maintain adequate blood flow through a narrower pathway, the heart must pump with greater force, leading to elevated blood pressure. Thus, answering the question “does vasoconstriction increase blood pressure” involves both a theoretical understanding and an appreciation of real-world clinical implications. In most cases, the answer is yes—vasoconstriction directly contributes to increased vascular resistance and thereby raises systemic blood pressure.
Hormonal and Neurological Drivers of Vasoconstriction
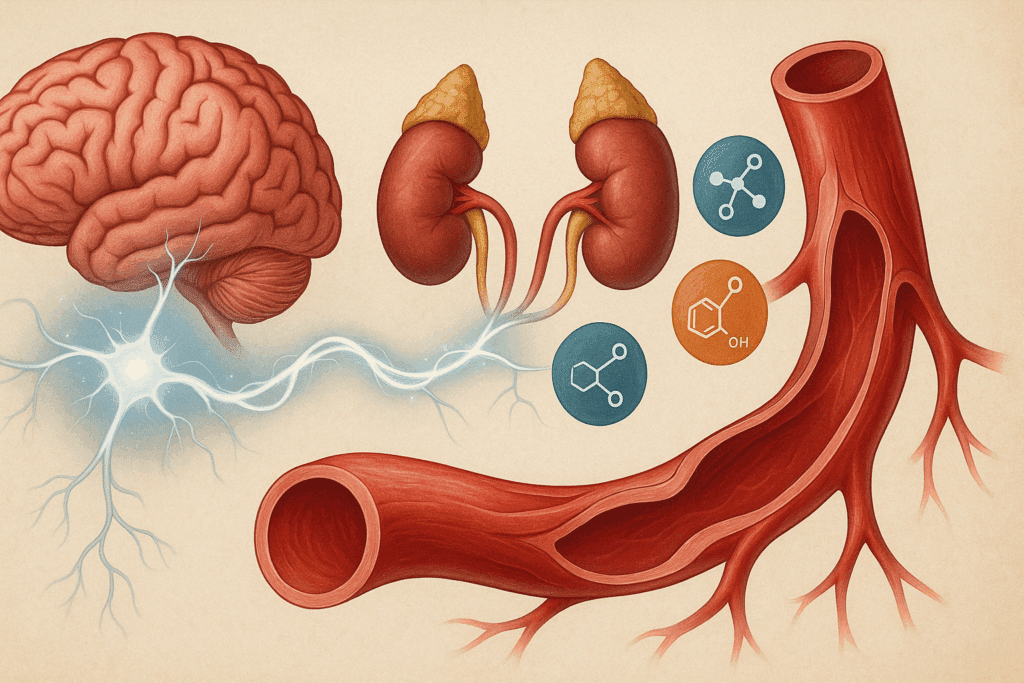
Vasoconstriction is not a random occurrence but is tightly controlled by various regulatory systems within the body. The sympathetic nervous system is a primary driver, especially during acute stress or in response to environmental changes like cold temperatures. When activated, this system releases catecholamines—particularly norepinephrine—which bind to alpha-adrenergic receptors on vascular smooth muscle, causing it to contract. This contraction results in a narrowed artery, increasing vascular tone and blood pressure.
In parallel, the renin-angiotensin-aldosterone system (RAAS) also plays a crucial role. When blood pressure drops or sodium levels are low, the kidneys release renin, which initiates a cascade leading to the production of angiotensin II. This potent vasoconstrictor acts on smooth muscle in blood vessels, further tightening the arterial walls and promoting sodium retention, which indirectly supports higher blood pressure. The hormonal orchestration of vasoconstriction illustrates how the body attempts to maintain hemodynamic stability, even if this means temporarily increasing the pressure within constricted arteries.
Pathological Vasoconstriction and Its Long-Term Implications
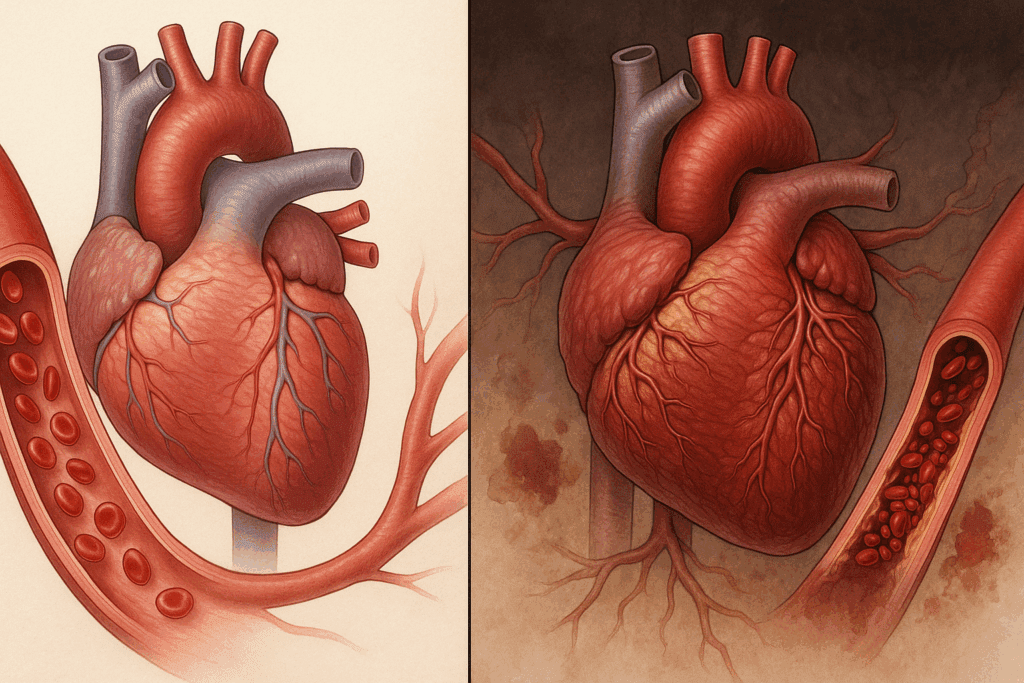
While transient vasoconstriction may be adaptive, chronic or excessive vasoconstriction can lead to pathological conditions. Hypertension, or high blood pressure, is among the most common outcomes of persistent vasoconstrictive activity. Over time, sustained elevation in vascular tone strains the heart, particularly the left ventricle, which must work harder to overcome the resistance presented by narrowed arteries. This can result in left ventricular hypertrophy, a risk factor for heart failure and arrhythmias.
Furthermore, chronically constricted arteries may impair blood flow to vital organs, including the brain, kidneys, and extremities. Ischemic damage—caused by insufficient oxygen supply—can arise in tissues that are downstream from persistently narrowed vessels. In the brain, this may manifest as transient ischemic attacks or strokes; in the kidneys, chronic ischemia may promote renal insufficiency and contribute to the progression of chronic kidney disease. Thus, the consequences of vasoconstriction extend well beyond elevated blood pressure, highlighting the importance of monitoring and managing vascular health.
Does Vasoconstriction Increase Blood Pressure in All Individuals?
Though it is generally accepted that vasoconstriction increases blood pressure, individual responses can vary significantly. Some people exhibit more robust sympathetic nervous system activation, while others may have different sensitivities to hormones like angiotensin II. Genetic factors, age, sex, and existing medical conditions all influence the extent to which vasoconstriction impacts blood pressure.
In healthy young individuals, the body may compensate for brief episodes of vasoconstriction by adjusting cardiac output or by initiating vasodilation in other vascular beds. However, in older adults or those with underlying cardiovascular conditions, these compensatory mechanisms may be blunted or impaired. For such populations, even moderate vasoconstriction can lead to clinically significant increases in blood pressure. This underscores the need for a personalized approach to blood pressure management, particularly in patients at higher cardiovascular risk.
How a Constricted Artery Reflects Systemic Vascular Health
The presence of a constricted artery is not merely a localized issue but often reflects broader systemic dysfunction. Atherosclerosis, characterized by the accumulation of plaque within arterial walls, can cause both structural narrowing and functional vasoconstriction. In such cases, the affected artery not only restricts blood flow but also loses its ability to dilate in response to increased demand. This dual impairment may manifest as angina in the heart or claudication in the legs, depending on the location of the blockage.
Moreover, a constricted artery is frequently accompanied by endothelial dysfunction—a condition in which the inner lining of blood vessels fails to produce adequate nitric oxide, a molecule essential for vasodilation. This contributes to a vicious cycle in which impaired relaxation of blood vessels perpetuates high blood pressure and further vascular injury. As such, evaluating a constricted artery can offer valuable insights into overall vascular health and inform both diagnostic and therapeutic decisions.
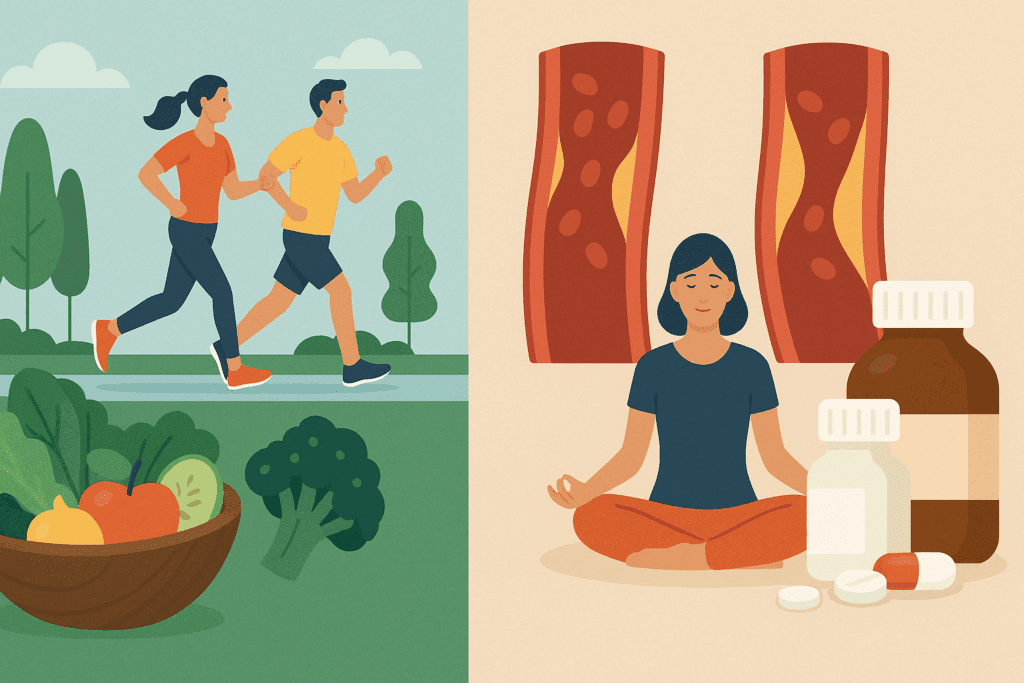
Pharmacological and Lifestyle Approaches to Managing Vasoconstriction
Given the link between vasoconstriction and elevated blood pressure, therapeutic strategies often aim to counteract excessive vascular tightening. Pharmacological agents such as calcium channel blockers, ACE inhibitors, and angiotensin receptor blockers are commonly prescribed to reduce vascular resistance. Calcium channel blockers prevent the influx of calcium ions into smooth muscle cells, inhibiting contraction and promoting vasodilation. Similarly, ACE inhibitors block the conversion of angiotensin I to angiotensin II, thereby reducing vasoconstrictive stimuli. These medications not only lower blood pressure but also improve arterial compliance and reduce the risk of end-organ damage.
Lifestyle modifications also play a vital role in regulating vascular tone. Regular aerobic exercise promotes the production of nitric oxide, enhancing endothelial function and encouraging vasodilation. A diet rich in fruits, vegetables, and omega-3 fatty acids supports vascular health, while minimizing sodium intake helps reduce fluid retention and pressure on arterial walls. Stress reduction techniques, including mindfulness and deep-breathing exercises, can lower sympathetic nervous system activity and help maintain normal vascular tone. Together, these interventions can reduce the likelihood of developing a constricted artery and mitigate the cardiovascular consequences associated with persistent vasoconstriction.
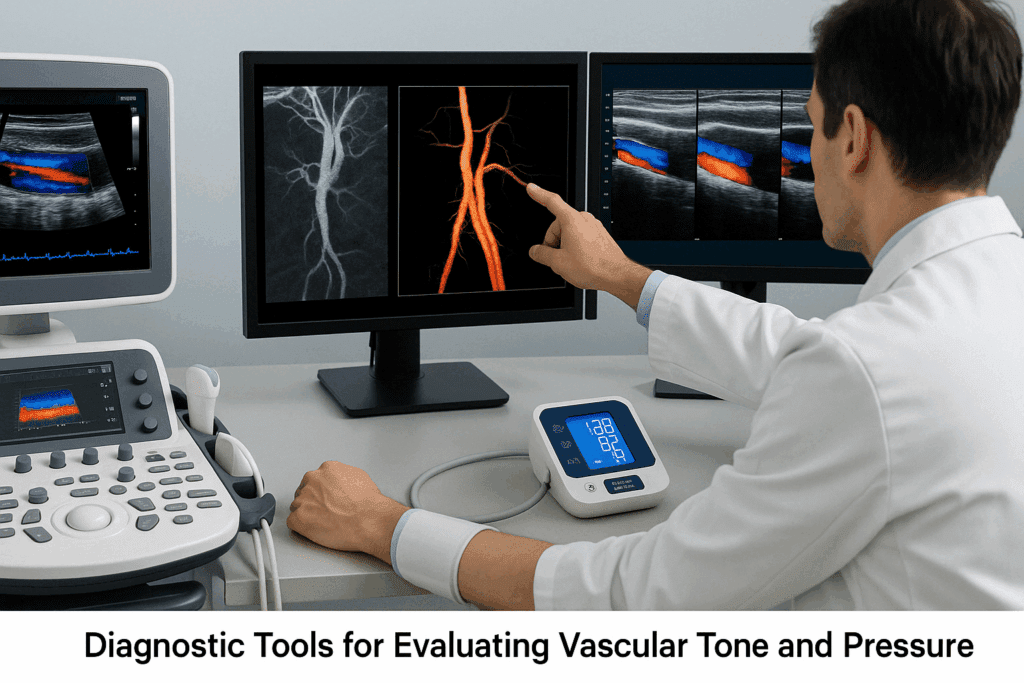
Diagnostic Tools for Evaluating Vascular Tone and Blood Pressure
Assessing the extent of vasoconstriction and its impact on blood pressure often requires a multifaceted diagnostic approach. Standard blood pressure measurement remains the primary tool for evaluating cardiovascular risk, but additional tests may provide deeper insights. Ambulatory blood pressure monitoring, for example, captures fluctuations in blood pressure throughout the day and night, revealing patterns that might suggest episodic vasoconstriction.
Doppler ultrasound and angiography are instrumental in visualizing blood flow and identifying areas of arterial narrowing. These imaging techniques can detect a constricted artery and assess whether the narrowing is due to vasoconstriction, structural abnormalities, or a combination of both. Endothelial function tests, including flow-mediated dilation, evaluate the ability of blood vessels to respond to stimuli, offering a window into vascular health at the microcirculatory level. These tools enable clinicians to distinguish between functional and structural contributors to high blood pressure, which can inform treatment decisions.
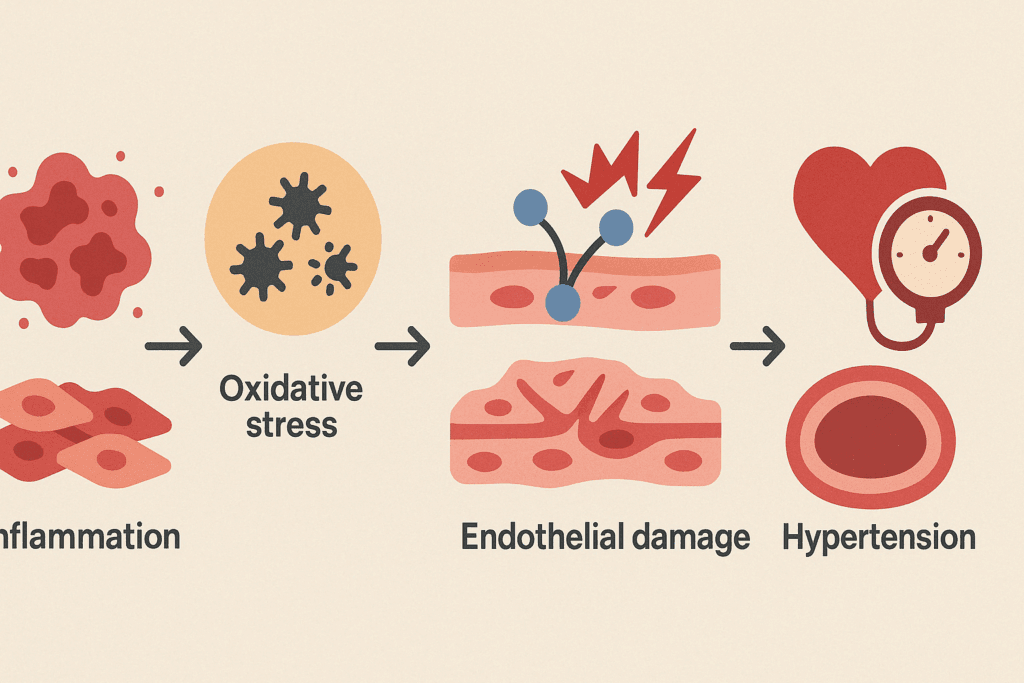
The Role of Inflammation and Oxidative Stress in Vascular Dysfunction
Emerging research highlights the role of inflammation and oxidative stress in promoting vasoconstriction and impairing vascular function. Chronic inflammation—often driven by obesity, metabolic syndrome, or autoimmune conditions—can upregulate pro-constrictive mediators and reduce nitric oxide availability. Reactive oxygen species (ROS) generated during oxidative stress can damage endothelial cells, disrupt smooth muscle function, and potentiate vasoconstrictive pathways.
This inflammatory milieu may also contribute to the development of a constricted artery by facilitating plaque formation and destabilization. Targeting these upstream factors through anti-inflammatory diets, antioxidant supplementation, or pharmacologic agents may offer a novel approach to improving vascular health. As scientific understanding evolves, therapies aimed at reducing vascular inflammation may become a cornerstone in the prevention and treatment of hypertension and related disorders.
Clinical Implications and Risk Stratification
Understanding the impact of vasoconstriction on blood pressure has profound clinical implications. Identifying individuals with heightened vasoconstrictive responses can help clinicians tailor interventions more precisely. For example, patients who exhibit excessive blood pressure surges in response to stress may benefit from beta-blockers, which blunt sympathetic nervous system activity. Similarly, those with evidence of RAAS overactivity may respond best to ACE inhibitors or ARBs.
Risk stratification also involves considering comorbid conditions. Diabetes, chronic kidney disease, and obstructive sleep apnea can exacerbate the effects of vasoconstriction on blood pressure and organ perfusion. In these cases, aggressive management of blood pressure may prevent further vascular damage and reduce the likelihood of complications such as stroke or heart failure. Thus, an individualized, multifactorial approach is essential for optimizing cardiovascular outcomes.
Public Health Considerations and Future Directions
From a public health perspective, addressing the determinants of excessive vasoconstriction requires a multifaceted strategy. Educational campaigns emphasizing the importance of dietary sodium reduction, physical activity, and stress management can promote vascular resilience across populations. Screening programs that identify individuals at risk of hypertension—especially those with a family history of cardiovascular disease—can facilitate early intervention.
Future research may yield novel therapies targeting specific molecular pathways involved in vasoconstriction. Gene editing technologies, biologics, and personalized medicine approaches hold promise for tailoring treatments based on an individual’s genetic and biochemical profile. As our understanding deepens, the ability to prevent or reverse the harmful consequences of a constricted artery may become an attainable goal for clinicians and public health experts alike.
Frequently Asked Questions: Vasoconstriction, Blood Pressure, and Constricted Arteries
1. Can psychological stress cause vasoconstriction and impact long-term blood pressure health?
Yes, chronic psychological stress can significantly influence vasoconstriction and blood pressure over time. The body’s stress response activates the sympathetic nervous system, leading to the release of hormones like norepinephrine, which can induce vasoconstriction. Over time, repeated episodes of stress-induced vasoconstriction may elevate baseline blood pressure, especially in individuals predisposed to hypertension. The link between mental health and cardiovascular health is increasingly recognized, and stress management strategies like cognitive-behavioral therapy, mindfulness meditation, and structured breathing exercises can help modulate sympathetic activation. This connection is vital when exploring whether or not vasoconstriction increases blood pressure in populations with high psychological stress exposure.
2. How does exposure to cold environments influence vasoconstriction and cardiovascular risk?
Cold temperatures naturally trigger vasoconstriction as a way to preserve body heat, but prolonged or frequent exposure can have cardiovascular consequences. In colder climates, constricted arteries become a common physiological response, particularly in extremities. This recurring vasoconstriction can elevate systemic blood pressure, especially in individuals with existing cardiovascular conditions. Seasonal blood pressure variations are a documented phenomenon, with higher incidences of cardiac events occurring in winter. Understanding that vasoconstriction increases blood pressure more prominently under cold exposure helps guide preventive strategies, such as warming measures and proper cardiovascular monitoring during colder months.
3. Are certain dietary habits linked to increased vasoconstriction or the development of constricted arteries?
Yes, diet plays a significant role in vascular tone and can either promote or inhibit vasoconstriction. High sodium intake, excessive alcohol consumption, and trans fats have all been shown to contribute to endothelial dysfunction and facilitate the formation of a constricted artery. These dietary elements may reduce the availability of nitric oxide, a critical molecule responsible for promoting vasodilation. Moreover, chronic consumption of processed foods can lead to systemic inflammation, compounding the effects of vasoconstriction on long-term blood pressure. Therefore, dietary interventions can be pivotal in addressing whether vasoconstriction increases blood pressure through chronic vascular damage.
4. Can a constricted artery develop without the presence of atherosclerosis?
While atherosclerosis is a leading cause of arterial narrowing, not all cases of constricted arteries are due to plaque buildup. Functional vasoconstriction, often mediated by hormonal imbalances or nervous system dysregulation, can produce transient but clinically significant narrowing. Conditions such as Raynaud’s phenomenon or coronary artery spasm illustrate how arteries can constrict without structural blockage. These functional constrictions can still restrict blood flow and elevate blood pressure episodically. Thus, the presence of a constricted artery does not always indicate atherosclerosis, but it does necessitate investigation into its underlying cause, especially when trying to determine whether vasoconstriction increases blood pressure on a recurrent basis.
5. What role does sleep quality play in modulating vasoconstriction and cardiovascular health?
Sleep deprivation or poor sleep quality can elevate sympathetic nervous system activity, contributing to increased vasoconstriction and, consequently, elevated blood pressure. Interrupted sleep disrupts hormonal balance, increasing cortisol and reducing melatonin—both of which can affect vascular tone. Repeated cycles of poor sleep can desensitize baroreceptors responsible for blood pressure regulation, exacerbating the impact of vasoconstriction on cardiovascular health. Over time, this contributes to a cycle where a constricted artery becomes more likely, especially in individuals with underlying sleep apnea. These findings suggest that consistent, high-quality sleep is an underrated yet crucial factor in moderating whether vasoconstriction increases blood pressure over the long term.
6. Is there a gender difference in how vasoconstriction affects blood pressure regulation?
Yes, gender differences exist in the physiological response to vasoconstriction, which in turn affects blood pressure regulation. Estrogen, for instance, promotes nitric oxide production and vasodilation, offering some protection against excessive vasoconstriction in premenopausal women. Postmenopausal women, however, experience a decline in this protective effect, leading to a higher incidence of hypertension and vascular stiffness. In men, testosterone has a more complex relationship with vascular tone, sometimes promoting vasoconstriction, particularly under conditions of stress or inflammation. These sex-specific variations are essential for understanding who may be more vulnerable to the effects of a constricted artery and the degree to which vasoconstriction increases blood pressure across life stages.
7. Are athletes or physically active individuals at lower risk of problems associated with vasoconstriction?
Regular physical activity is strongly associated with improved endothelial function and reduced vascular resistance. In athletes, the cardiovascular system becomes more efficient at regulating blood flow, often resulting in lower resting blood pressure and reduced sensitivity to vasoconstrictive triggers. Exercise increases nitric oxide production, which counters the narrowing effects on arteries and supports optimal vascular tone. However, overtraining without sufficient recovery can paradoxically increase sympathetic activity and provoke vasoconstriction in some cases. This highlights the importance of balanced training regimens and cardiovascular monitoring, even in populations generally less susceptible to the risks of a constricted artery or the concern of whether vasoconstriction increases blood pressure.
8. How does high-altitude living or travel impact vasoconstriction and arterial pressure?
At high altitudes, the body adapts to reduced oxygen levels through multiple mechanisms, one of which is increased vasoconstriction in certain vascular beds, particularly the pulmonary circulation. This physiological adjustment can raise pulmonary arterial pressure and potentially affect systemic blood pressure as well. For some individuals, especially those with pre-existing cardiovascular conditions, altitude-induced vasoconstriction may exacerbate symptoms or unmask underlying hypertension. It becomes particularly important to monitor individuals with a history of a constricted artery when traveling to or living in high-altitude regions. These conditions underscore the environmental dimensions of the broader question: does vasoconstriction increase blood pressure, and under what circumstances does it become clinically relevant?
9. Can vasoconstriction and blood pressure be influenced by pharmaceutical drug interactions?
Yes, several medications can either amplify or suppress vasoconstrictive effects, thereby influencing blood pressure regulation. Decongestants containing pseudoephedrine, for example, can constrict arteries and raise blood pressure, especially in individuals sensitive to sympathetic stimulation. Conversely, certain antidepressants or anti-anxiety medications may blunt sympathetic activity and reduce vasoconstrictive episodes. Drug interactions—such as combining blood pressure medications with vasoconstrictive agents—can lead to unpredictable outcomes, especially in patients with complex health profiles. Recognizing how pharmaceutical interventions affect whether vasoconstriction increases blood pressure is a key element in personalized cardiovascular care.
10. What are the long-term psychological impacts of living with undiagnosed vasoconstriction-related hypertension?
Living with undiagnosed hypertension caused by persistent vasoconstriction can take a psychological toll, often leading to anxiety, chronic fatigue, and reduced quality of life. Individuals may experience unexplained symptoms like headaches, dizziness, or palpitations without a clear diagnosis, which can increase psychological distress. Over time, the lack of clarity surrounding a constricted artery or elevated blood pressure may erode trust in medical evaluations and contribute to healthcare avoidance. Early diagnosis and a clear understanding of how vasoconstriction increases blood pressure are critical not just for physical health, but also for psychological well-being. Integrative care models that address both mental and cardiovascular health can improve outcomes and restore patient confidence in long-term disease management.
Key Takeaways on Vasoconstriction, Constricted Arteries, and Blood Pressure Management
A nuanced understanding of how vasoconstriction affects blood pressure is essential for managing both individual and public health. The narrowing of blood vessels—whether due to acute stress, hormonal regulation, or pathological conditions—plays a central role in determining vascular resistance and cardiovascular risk. While the answer to the question “does vasoconstriction increase blood pressure” is generally affirmative, the underlying mechanisms and individual variations provide critical context for clinical decision-making.
Equally important is recognizing that a constricted artery may indicate broader systemic issues, including atherosclerosis, endothelial dysfunction, and chronic inflammation. Addressing these root causes through a combination of pharmacological, lifestyle, and public health strategies offers a comprehensive path toward better cardiovascular outcomes. By continuing to explore the intricate relationship between vascular tone and blood pressure, healthcare professionals can empower patients to take proactive steps in preserving their vascular health and preventing life-threatening complications.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.