Can Aspirin Raise Blood Pressure? Aspirin has long held a prominent place in the world of cardiovascular medicine. Often hailed as a preventative measure against heart attacks and strokes, it is commonly recommended for individuals with certain cardiovascular risk factors. However, for all its benefits, aspirin is not without its risks. One of the more nuanced questions surrounding this common medication is whether it can raise blood pressure. Given that hypertension itself is a leading cause of cardiovascular disease, understanding this potential interaction is not only important—it is essential. This article examines the relationship between aspirin use and blood pressure, exploring the scientific evidence, clinical implications, and what patients should know when weighing the pros and cons of aspirin therapy.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Understanding Aspirin’s Role in Cardiovascular Health
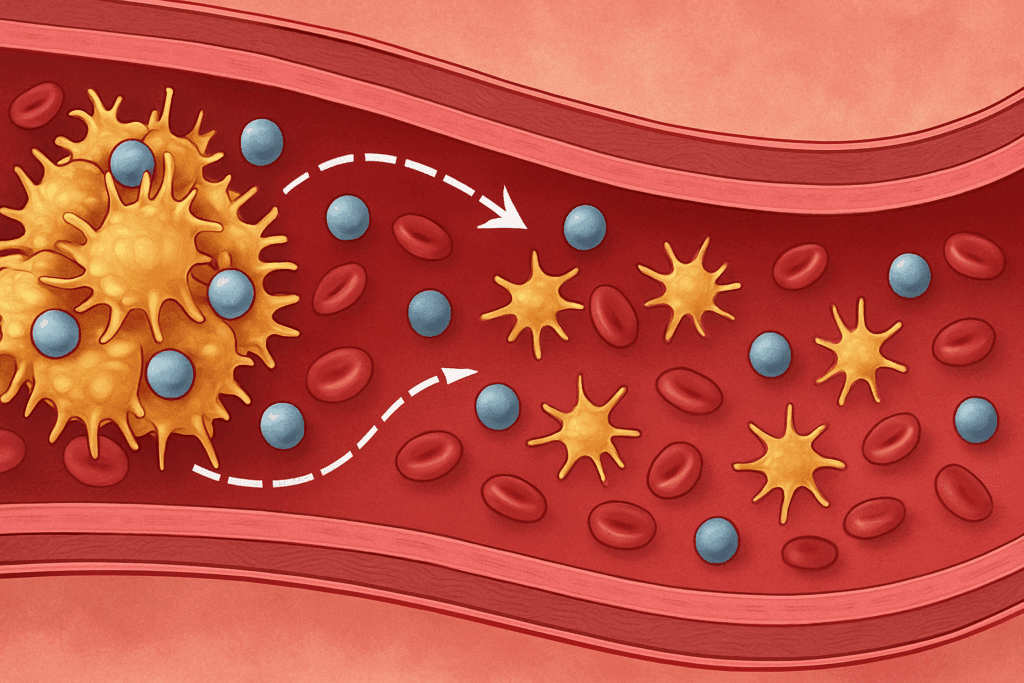
Aspirin, or acetylsalicylic acid, is widely used for its antiplatelet properties, which help prevent the formation of blood clots. By inhibiting cyclooxygenase (COX) enzymes, aspirin reduces the production of thromboxane A2, a molecule that promotes platelet aggregation. This mechanism makes it a cornerstone in secondary prevention strategies for individuals who have experienced myocardial infarction, stroke, or other forms of vascular disease. In some cases, low-dose aspirin is also prescribed for primary prevention, particularly in patients with elevated cardiovascular risk profiles.
Beyond its clot-preventing effects, aspirin also possesses anti-inflammatory properties, which have implications for a range of chronic diseases. However, these benefits come with caveats, particularly for individuals with hypertension. While aspirin has been a trusted agent for decades, emerging research has prompted healthcare providers to revisit its risk-benefit profile, especially in patients with coexisting conditions such as high blood pressure.
The Pharmacological Interaction Between Aspirin and Blood Pressure
To understand whether aspirin can raise blood pressure, it is important to explore how it interacts with the vascular system. Some studies suggest that aspirin may have a neutral or even slightly beneficial effect on blood pressure, particularly when taken at night. This observation is thought to be related to its ability to reduce platelet activity and inflammation, both of which play a role in endothelial function and vascular tone.
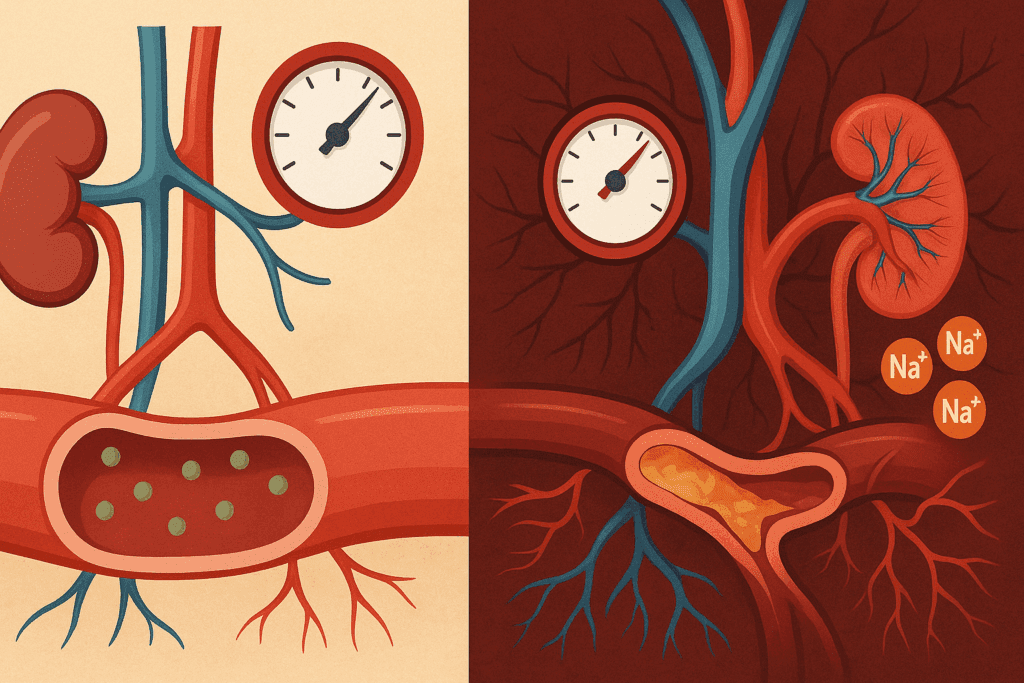
On the other hand, some findings indicate that aspirin may increase blood pressure in certain populations, particularly when taken in conjunction with other nonsteroidal anti-inflammatory drugs (NSAIDs). Unlike aspirin, which irreversibly inhibits COX enzymes, other NSAIDs often have reversible effects and can lead to sodium retention, decreased renal perfusion, and vasoconstriction—all of which can elevate blood pressure. The question then becomes: does aspirin raise blood pressure in a clinically meaningful way, or are these changes negligible for most users?
Clinical Evidence: Does Aspirin Raise Blood Pressure in Real-World Settings?
The clinical data on aspirin and blood pressure are mixed, reflecting the complexity of individual physiology and coexisting risk factors. A number of studies have attempted to determine whether aspirin has a direct hypertensive effect, and the findings vary based on patient demographics, dosage, timing of administration, and concurrent medication use.
In a notable trial involving hypertensive patients, evening administration of low-dose aspirin was associated with a modest reduction in systolic blood pressure compared to morning use. This supports the hypothesis that circadian rhythms influence aspirin’s cardiovascular effects. Conversely, other trials have not found statistically significant differences in blood pressure readings with aspirin use, suggesting that its impact may be minimal or context-dependent.
Despite these nuances, clinicians continue to evaluate whether aspirin can raise blood pressure in patients already at risk for cardiovascular complications. For individuals with well-controlled hypertension, low-dose aspirin is generally considered safe, though monitoring remains essential. The potential for aspirin to raise blood pressure appears to be more theoretical than consistently observed in clinical practice, but it warrants consideration in vulnerable populations.
Can Aspirin Raise Blood Pressure in Older Adults?
Older adults often face a higher burden of comorbid conditions, including hypertension, kidney dysfunction, and vascular rigidity. These factors may influence how aspirin affects their blood pressure. Several studies have explored the use of aspirin in geriatric populations, particularly those with existing cardiovascular disease or multiple risk factors.
In this demographic, the question of whether aspirin can raise blood pressure becomes particularly relevant. The presence of age-related changes in renal function, increased sensitivity to sodium retention, and polypharmacy can amplify the effects of even small changes in medication. While most older adults tolerate low-dose aspirin well, clinicians remain cautious about its use in those with labile blood pressure or fragile cardiovascular systems.
Research has not conclusively demonstrated that aspirin consistently raises blood pressure in older adults, but it highlights the importance of individualized care. Physicians often weigh the antithrombotic benefits of aspirin against its potential risks, including gastrointestinal bleeding and possible hypertensive effects. In some cases, alternative strategies such as statins or lifestyle modifications may be prioritized over routine aspirin use.
Will Aspirin Raise Blood Pressure When Used with Other Medications?
Drug interactions represent a key variable in determining whether aspirin might raise blood pressure. Many individuals who are prescribed aspirin are also taking antihypertensive medications, statins, or other cardiovascular agents. The interaction between these drugs can modulate aspirin’s effects on vascular tone and blood pressure regulation.
For example, when aspirin is combined with certain diuretics or ACE inhibitors, there may be a reduction in the efficacy of the blood pressure-lowering agents. This is more likely to occur with higher doses of aspirin, but even low doses can sometimes interfere with renal perfusion. Additionally, the simultaneous use of other NSAIDs like ibuprofen or naproxen may compound this effect, leading to increases in blood pressure that might not be attributed to aspirin alone.
It is important to note that while aspirin can interact with other drugs, it does not always raise blood pressure in a clinically significant way. However, for patients on complex medication regimens, regular monitoring and medication reconciliation are crucial. Pharmacists and physicians should collaborate to assess the full spectrum of drug interactions and ensure that any increase in blood pressure is promptly identified and managed.
Individual Variability and Risk Factors to Consider
One of the reasons the question “does aspirin raise blood pressure” does not have a universal answer is because of the wide variability in individual responses. Factors such as genetic predisposition, baseline blood pressure, metabolic profile, and lifestyle habits can all influence how aspirin affects the cardiovascular system.
For instance, individuals with salt-sensitive hypertension may be more prone to blood pressure fluctuations due to the renal effects of aspirin and similar medications. Likewise, those with a history of kidney disease, congestive heart failure, or autonomic dysfunction may exhibit different hemodynamic responses compared to the general population.
Gender, age, and even the presence of metabolic syndrome can also shape how aspirin influences blood pressure regulation. Understanding these variables is essential for clinicians when evaluating whether aspirin is appropriate for a given patient. While population-level studies provide valuable insights, individual-level assessments are often necessary to determine the best course of action.
Safe Use Guidelines for Patients Taking Aspirin
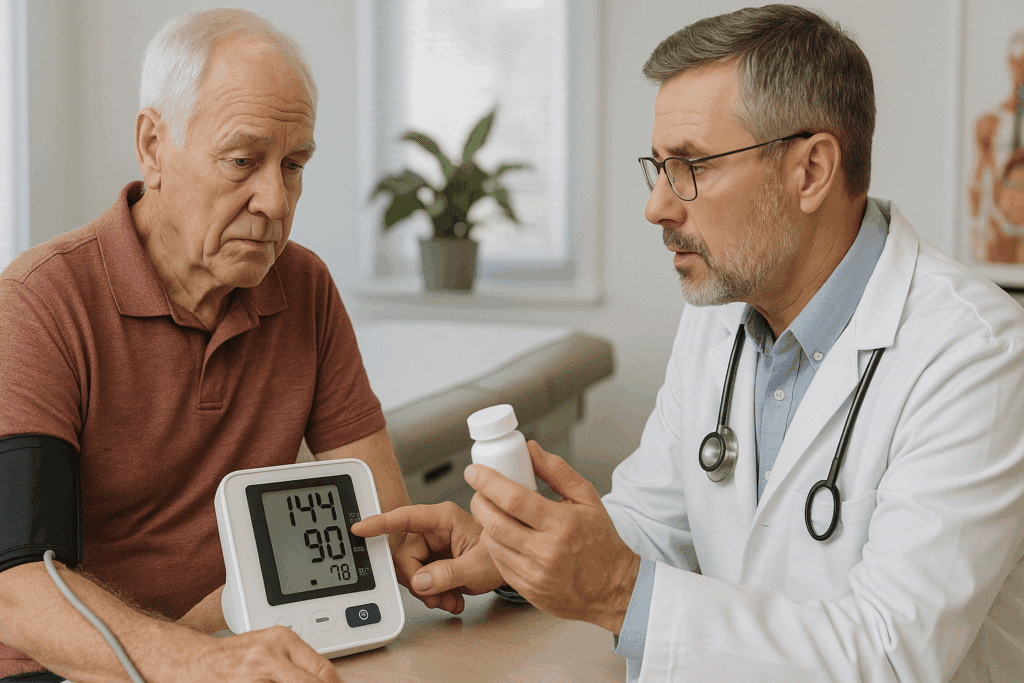
Given the complexities surrounding aspirin use and its potential effects on blood pressure, patients should adhere to a set of safety guidelines when incorporating aspirin into their treatment regimen. First and foremost, aspirin should never be started without the recommendation of a qualified healthcare provider. Despite its over-the-counter availability, aspirin is a powerful drug that can have serious side effects if misused.
Patients should regularly monitor their blood pressure, especially during the initial weeks of starting aspirin therapy. If any significant elevations are noted, they should consult their physician immediately. It is also wise to inform all healthcare providers, including dentists and pharmacists, about aspirin use to prevent complications during medical or surgical procedures.
Lifestyle factors should not be neglected. A heart-healthy diet, regular physical activity, stress management, and adequate sleep all contribute to optimal cardiovascular health and can help mitigate any minor fluctuations in blood pressure that might occur with aspirin use. In some cases, clinicians may recommend taking aspirin at night to align with the body’s circadian rhythms, potentially enhancing its benefits while minimizing any adverse effects.
Evaluating Alternatives: Is Aspirin Always the Best Option?
While aspirin remains a valuable tool in cardiovascular medicine, it is not always the best or only option. As more data emerge about its risks and benefits, especially in primary prevention, alternatives are increasingly being considered. Statins, for instance, offer robust protection against cardiovascular events by lowering cholesterol and exerting anti-inflammatory effects. Unlike aspirin, statins do not carry a significant risk of gastrointestinal bleeding or blood pressure elevation.
Other antiplatelet agents such as clopidogrel may be preferred in patients with aspirin intolerance or those at higher risk for gastrointestinal complications. Meanwhile, non-pharmacologic approaches such as the Mediterranean diet, smoking cessation, and routine physical activity provide foundational support for heart health without the risks associated with medications.
When weighing these options, clinicians must consider the patient’s overall risk profile, preferences, and tolerance for potential side effects. The decision to use aspirin should be based on a comprehensive assessment, not just a one-size-fits-all guideline. Shared decision-making between doctor and patient remains the gold standard in cardiovascular care.
The Role of Timing: Does It Matter When You Take Aspirin?
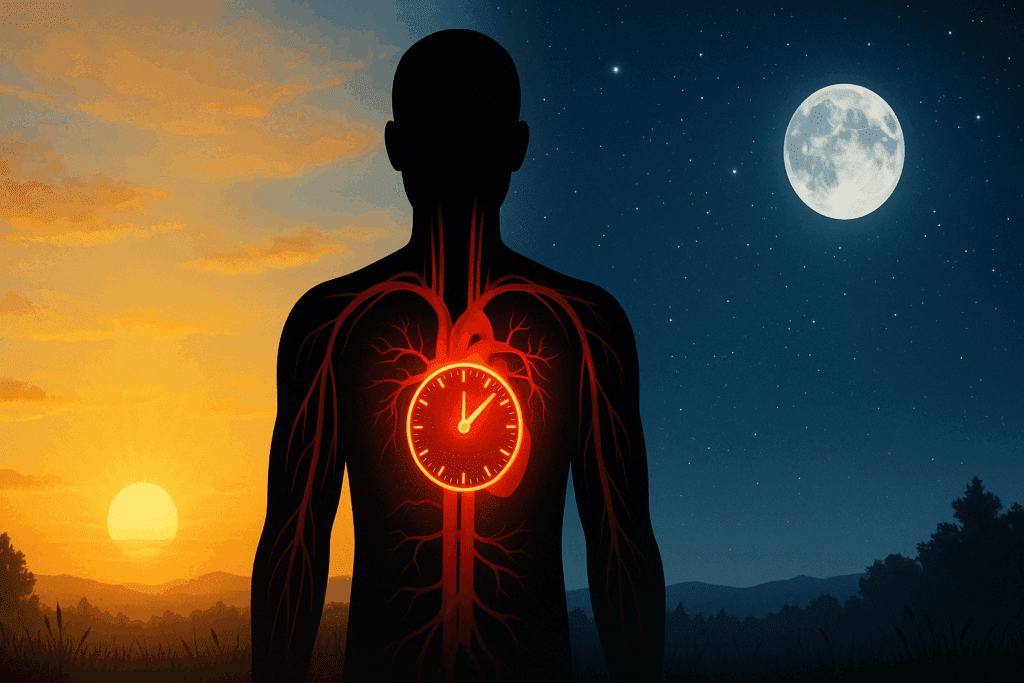
A growing body of research suggests that the timing of aspirin administration can influence its effects on blood pressure. Some studies indicate that taking aspirin in the evening may enhance its ability to reduce blood pressure, particularly in individuals with nocturnal hypertension or non-dipping blood pressure patterns. This phenomenon is tied to the body’s circadian rhythms, which affect blood pressure regulation and platelet activity.
Evening dosing may also minimize the risk of gastrointestinal side effects, as the stomach is generally less active during nighttime hours. However, more research is needed to determine the optimal timing for different patient populations. Until then, consistency remains key—patients should take aspirin at the same time each day unless instructed otherwise by their physician.
This growing interest in chronotherapy, or time-based medication administration, reflects the evolving understanding of how drug effects can be optimized by aligning with the body’s natural rhythms. For those wondering, “can aspirin raise blood pressure depending on when it’s taken?”—the answer appears to be yes, but in a way that may actually be beneficial when timed appropriately.
Frequently Asked Questions (FAQ): Aspirin and Blood Pressure
1. How does aspirin affect blood pressure differently in people with metabolic syndrome?
Individuals with metabolic syndrome often have a complex interplay of insulin resistance, inflammation, and endothelial dysfunction, all of which can amplify cardiovascular risks. In these cases, even low-dose aspirin may interact unpredictably with vascular tone. Research indicates that in people with metabolic syndrome, the question “does aspirin raise blood pressure” becomes more nuanced due to their heightened inflammatory state. While aspirin may reduce systemic inflammation, which could benefit blood pressure, metabolic irregularities may blunt these effects or even lead to unintended pressure fluctuations. It’s essential for individuals with metabolic syndrome to undergo frequent blood pressure monitoring if aspirin is part of their therapeutic regimen.
2. Can nighttime dosing of aspirin improve blood pressure outcomes more effectively than morning dosing?
There is growing interest in the concept of chronotherapy, which explores how the timing of medication impacts its effectiveness. Some studies suggest that taking aspirin at night may optimize its antiplatelet effects and reduce the risk of morning cardiovascular events, which are more common due to early-day blood pressure spikes. This has led researchers to ask: not just does aspirin raise blood pressure, but when might its administration minimize any adverse impact? Nighttime dosing may better align with circadian patterns in blood pressure and platelet activity, possibly offering a modest benefit in hypertensive control. However, this approach is not universally effective and should be guided by a physician familiar with the patient’s overall health status.
3. Will aspirin raise blood pressure more significantly in patients with existing kidney disease?
Patients with chronic kidney disease are more susceptible to shifts in fluid and electrolyte balance, which can make them more vulnerable to blood pressure changes. When used inappropriately or at higher doses, aspirin can impair renal perfusion and sodium excretion, potentially leading to elevated blood pressure. In clinical settings, nephrologists often approach aspirin use cautiously in this population. Thus, when exploring whether aspirin will raise blood pressure in those with kidney impairment, the answer leans toward caution, especially when combined with other nephrotoxic agents. A thorough evaluation of kidney function is warranted before initiating regular aspirin therapy in such individuals.
4. Are there gender differences in how aspirin affects blood pressure?
Emerging evidence suggests that hormonal variations, especially estrogen in premenopausal women, may influence how aspirin interacts with vascular systems. Some studies have observed that men and women may respond differently to the anti-inflammatory and antiplatelet effects of aspirin, which raises the question: can aspirin raise blood pressure differently across sexes? Estrogen is known to have vasodilatory effects, and its presence may modulate how aspirin affects vascular reactivity. While more research is needed, preliminary findings indicate that female hormonal cycles could potentially mediate aspirin’s influence on blood pressure dynamics. Personalized treatment plans that consider gender-specific responses are increasingly advocated in cardiovascular care.
5. How does aspirin use impact blood pressure during periods of high stress or anxiety?
Stress and anxiety are known to elevate blood pressure through sympathetic nervous system activation and cortisol release. In such heightened states, even medications with generally neutral effects might contribute to adverse cardiovascular responses. Patients often wonder, during emotionally taxing times, does aspirin raise blood pressure more than it would under normal conditions? While no definitive link has been established, stress-induced changes in blood flow and hormone levels could theoretically exaggerate aspirin’s hemodynamic influence. Managing psychological stress alongside medication use is critical, and physicians may suggest incorporating mindfulness, therapy, or relaxation techniques to support cardiovascular stability.
6. Can the long-term use of aspirin subtly increase blood pressure over time?
Long-term medication use often raises questions about cumulative physiological effects. While aspirin is not typically associated with sustained hypertensive trends, some researchers continue to explore whether extended use—particularly at higher doses—may affect renal function or vascular integrity in ways that gradually influence blood pressure. Asking whether aspirin can raise blood pressure over time may lead to individualized insights, especially for aging populations or those with borderline hypertension. Routine blood pressure monitoring and periodic re-evaluation of the necessity for aspirin therapy help ensure that any long-term risks are identified early. Patients on prolonged aspirin regimens should also receive regular kidney function assessments.
7. Are there specific populations for whom aspirin use is more likely to raise blood pressure?
Yes, individuals with salt-sensitive hypertension, autonomic dysfunction, or polypharmacy-induced interactions are at higher risk. For these patients, the question “will aspirin raise blood pressure” becomes more than academic; it represents a practical clinical concern. In salt-sensitive individuals, any medication that alters sodium retention or renal function can shift blood pressure upward. Similarly, older adults managing multiple medications may encounter compounded effects that disrupt vascular homeostasis. Identifying these high-risk groups allows for a more tailored approach and emphasizes the need for individualized medical supervision.
8. How do lifestyle habits influence the extent to which aspirin affects blood pressure?
Diet, hydration, physical activity, and sleep patterns all play a crucial role in determining cardiovascular response to medications, including aspirin. A sedentary lifestyle, excessive sodium intake, or dehydration can increase the likelihood that aspirin will affect blood pressure, especially when combined with other risk factors. So, when patients ask, “can aspirin raise blood pressure if my lifestyle is unhealthy?”—the answer is a cautious yes. Improving overall health habits can not only reduce cardiovascular risk but also buffer against medication-related fluctuations. Healthcare providers should encourage a holistic strategy that integrates pharmacological and lifestyle-based interventions.
9. Is there a connection between aspirin-induced gastrointestinal effects and changes in blood pressure?
While the primary focus of aspirin use is often on its cardiovascular and clot-preventing actions, its gastrointestinal side effects should not be overlooked. Chronic gastrointestinal bleeding can lead to anemia, which may initially lower blood pressure due to reduced blood volume. However, compensatory mechanisms—such as vasoconstriction and increased cardiac output—may later result in blood pressure instability. Therefore, in rare cases, the question “does aspirin raise blood pressure” could be indirectly answered through a cascade of secondary effects related to GI health. Patients experiencing persistent gastrointestinal discomfort should consult a physician to adjust dosage or explore alternative therapies.
10. What innovations in cardiovascular medicine might reduce the need for aspirin in the future?
The medical field is rapidly evolving, with emerging therapies offering alternatives to traditional aspirin use. Precision medicine, pharmacogenomics, and novel antiplatelet agents tailored to individual risk profiles are becoming more prominent. As these innovations advance, fewer patients may rely on aspirin, particularly if other agents offer equal protection with fewer risks. In this context, the inquiry “will aspirin raise blood pressure” may become less central, replaced by more personalized risk assessments and targeted interventions. Advances in wearable technology and remote patient monitoring also promise to provide real-time feedback on blood pressure and medication efficacy, further reducing reliance on broad-spectrum treatments like aspirin.
Conclusion: What Patients Should Know About Aspirin and Blood Pressure
As research continues to evolve, the relationship between aspirin and blood pressure remains a topic of active investigation. For most patients, particularly those using low-dose aspirin under medical supervision, the risk of significant blood pressure elevation appears to be low. However, the question of “does aspirin raise blood pressure” cannot be answered with a simple yes or no. Individual physiology, timing, dosage, and the presence of other medications all play a role in determining the net effect.
Heart patients considering aspirin therapy should engage in open dialogue with their healthcare providers to assess the benefits and potential risks. Regular blood pressure monitoring, lifestyle modifications, and careful attention to medication interactions are all essential components of a safe and effective cardiovascular strategy. Ultimately, while aspirin is a powerful ally in heart health, it must be used thoughtfully and intentionally, especially for those with or at risk for hypertension.
In summary, while aspirin does not typically raise blood pressure in a clinically significant way, it can interact with other factors in ways that merit close attention. The keyword phrases “does aspirin raise blood pressure,” “can aspirin raise blood pressure,” and “will aspirin raise blood pressure” are not just queries—they represent important clinical considerations that every patient and provider should thoughtfully explore before beginning or continuing aspirin therapy.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Is Taking Aspirin Good for Your Heart?