Reimagining Modern Medicine Through Innovation
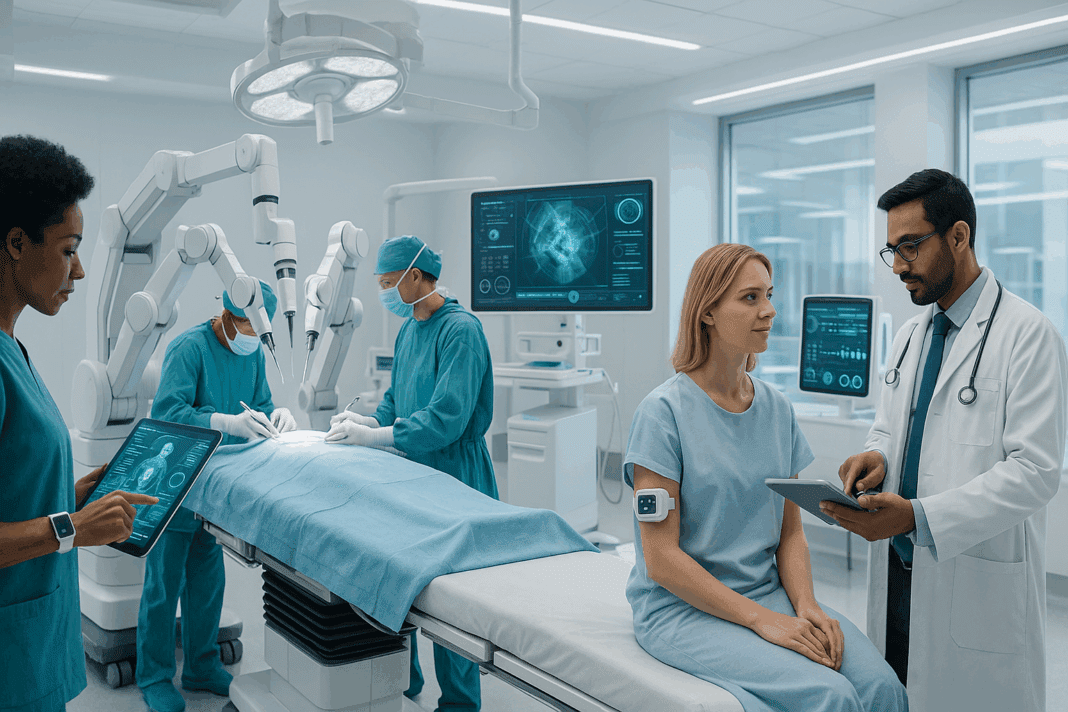
The landscape of patient care is undergoing a dramatic evolution, powered by recent medical technology that redefines the boundaries of diagnosis, treatment, and recovery. Gone are the days when clinical decisions relied solely on a physician’s intuition and standard laboratory tests. Today, we inhabit a world where artificial intelligence can detect disease at its earliest stages, wearable devices provide real-time monitoring of vital signs, and minimally invasive surgical robots carry out procedures with microscopic precision. This convergence of medical science and technological innovation not only enhances the accuracy of diagnoses and the effectiveness of treatments, but it also fosters a more personalized and patient-centered approach to healthcare. As we stand at the forefront of this digital revolution, it is vital to understand how these changes are reshaping the practice of medicine and transforming lives in profound and meaningful ways.
You may also like: Advancements in Healthcare Technology: How Emerging Innovations Are Transforming Patient Care

Understanding the Current Landscape of Technological Integration in Healthcare
The integration of new medical tech into clinical practice is no longer a theoretical aspiration; it is a tangible reality influencing every facet of patient care. Hospitals and clinics across the globe are increasingly adopting electronic health records (EHRs), telemedicine platforms, and advanced imaging modalities that provide a more cohesive, data-driven view of a patient’s health status. The recent wave of digitization has also enabled the development of predictive analytics tools, allowing clinicians to forecast health trends and intervene proactively. This digital ecosystem creates a seamless flow of information, empowering care providers to make faster, more informed decisions.
In parallel, patient engagement is seeing a transformation. Individuals are more informed and involved in their own care journeys, aided by technologies that deliver accessible information, reminders, and health tracking capabilities. This democratization of data fosters transparency and shared decision-making, elevating the quality of care while also improving patient satisfaction. With these advancements, the conversation is no longer just about improving medical outcomes—it’s about reshaping the entire healthcare experience.
The Role of Artificial Intelligence in Diagnostic Precision
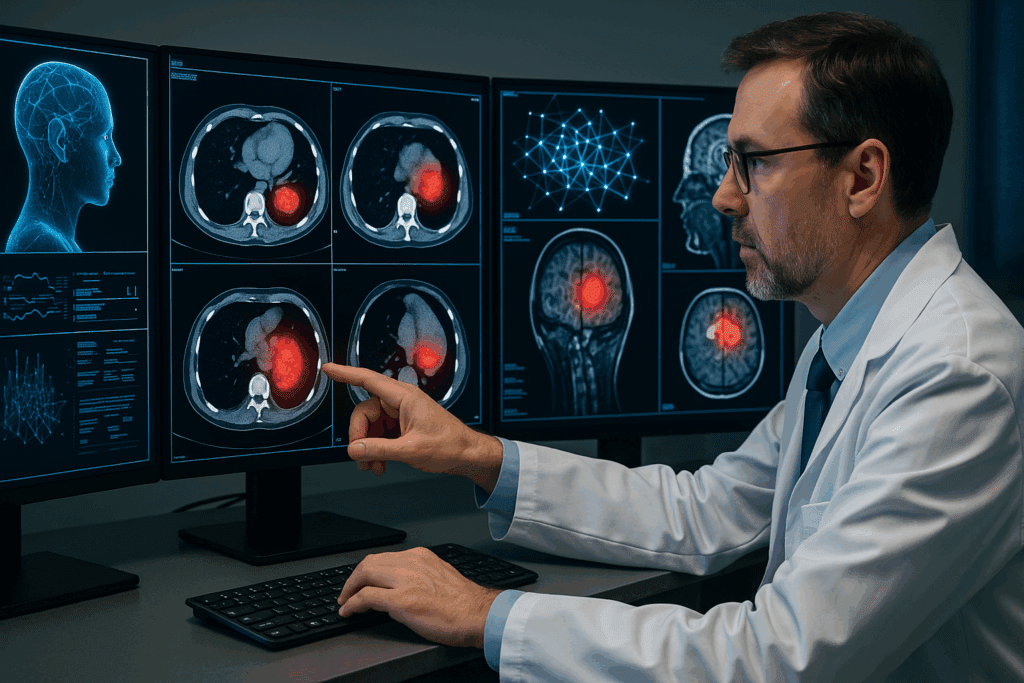
Artificial intelligence (AI) is arguably the most transformative force in recent medical technology. By processing vast datasets at speeds unattainable by human minds, AI systems can recognize complex patterns, identify anomalies, and suggest potential diagnoses with remarkable accuracy. In radiology, for instance, deep learning algorithms now assist in the interpretation of medical images, flagging abnormalities that might otherwise go unnoticed. This has proven particularly valuable in the early detection of cancers, where timely intervention is critical to survival.
Beyond image analysis, AI is also making significant strides in pathology, genomics, and even primary care. Chatbot-driven interfaces are being employed for preliminary assessments, triaging patients efficiently before they meet with a physician. Meanwhile, AI-driven genetic screening tools can predict disease susceptibility, enabling preemptive lifestyle adjustments or therapeutic interventions. As these systems continue to learn and evolve, they are poised to become indispensable partners in the diagnostic process.
Wearable Technology and the Rise of Personalized Monitoring
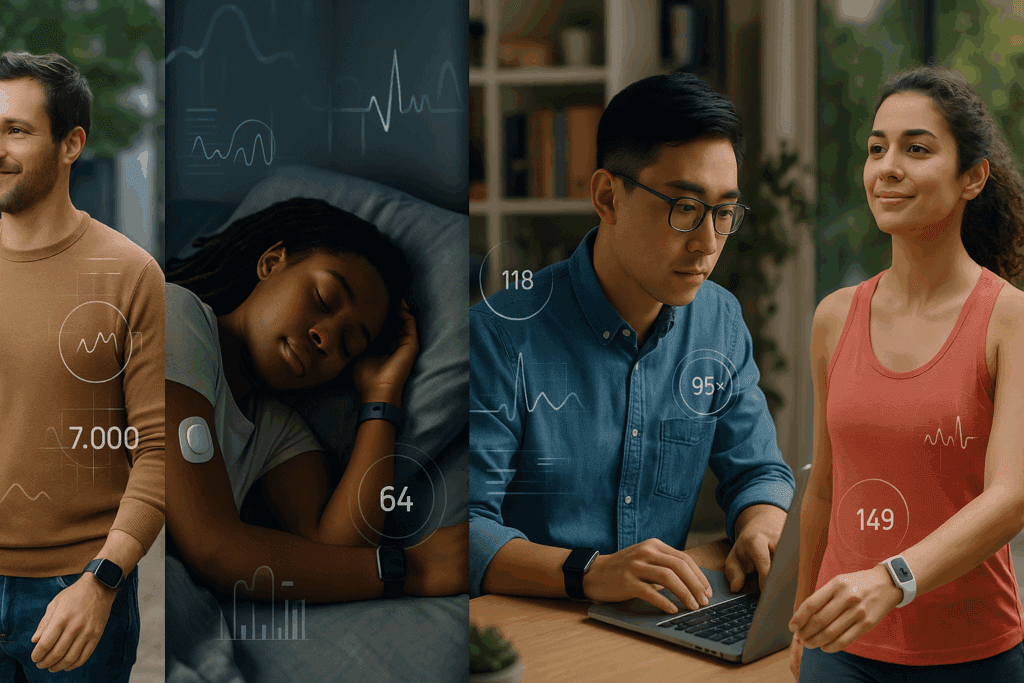
Wearable devices represent a quintessential example of new medical tech that has migrated from the consumer wellness market into the clinical realm. What began as fitness trackers has evolved into a sophisticated suite of wearable biosensors capable of continuously monitoring heart rate, blood oxygen levels, sleep quality, glucose levels, and even cardiac rhythms. For patients with chronic conditions such as diabetes, heart failure, or hypertension, these devices offer a lifeline—providing real-time data that can prompt early interventions and avert complications.
This technological evolution is a cornerstone in what is often described as the “quantified self” movement, where individuals leverage data to better understand and manage their health. It also enables more tailored and responsive care models. Physicians can now monitor their patients remotely and make informed decisions without requiring in-person visits. In a broader sense, wearable technologies are democratizing access to continuous care, empowering patients to take control of their health and participate actively in managing their well-being.
Robotics and Minimally Invasive Surgical Innovations
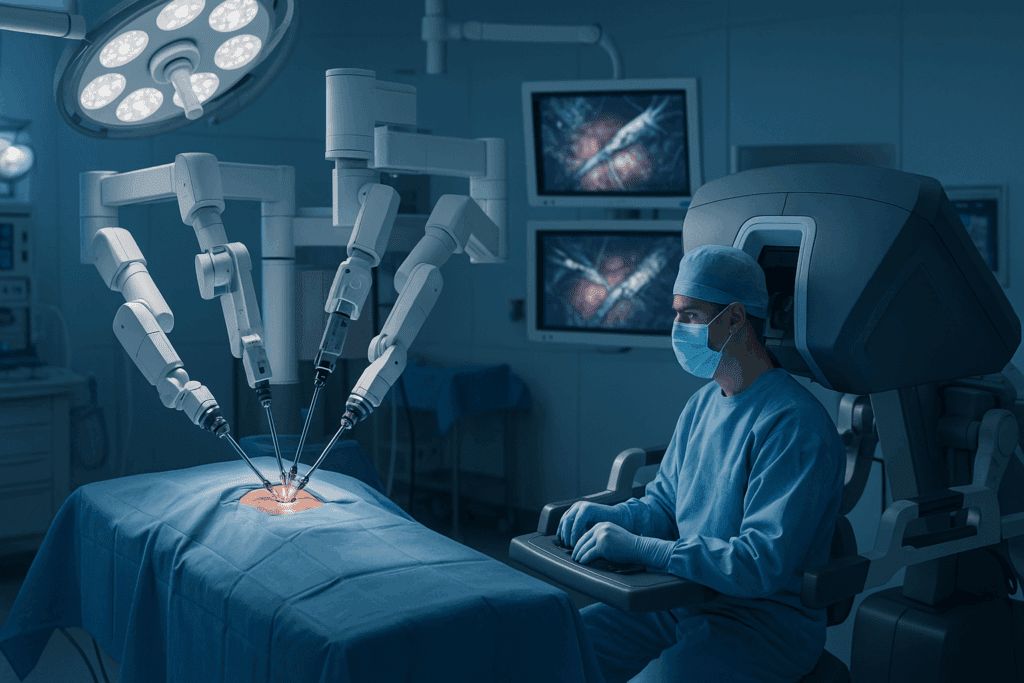
In the surgical theater, robotics has emerged as one of the most impactful advancements in recent medical technology. Robotic-assisted surgeries enable unparalleled precision, smaller incisions, reduced blood loss, and quicker recovery times. Systems such as the da Vinci Surgical System have become increasingly prevalent in urological, gynecological, and gastrointestinal procedures, allowing for enhanced maneuverability and visualization in confined anatomical spaces.
What makes this new medical tech particularly revolutionary is its ability to amplify human skill rather than replace it. Surgeons remain in control, guiding robotic instruments with dexterity and receiving real-time feedback. Meanwhile, enhanced imaging and haptic technology allow for a level of detail and control that far surpasses traditional techniques. As robotic systems become more sophisticated and affordable, their application is expected to expand beyond large hospitals to include outpatient centers and rural clinics, addressing longstanding disparities in access to advanced surgical care.
Telemedicine: Expanding Access and Reducing Barriers to Care
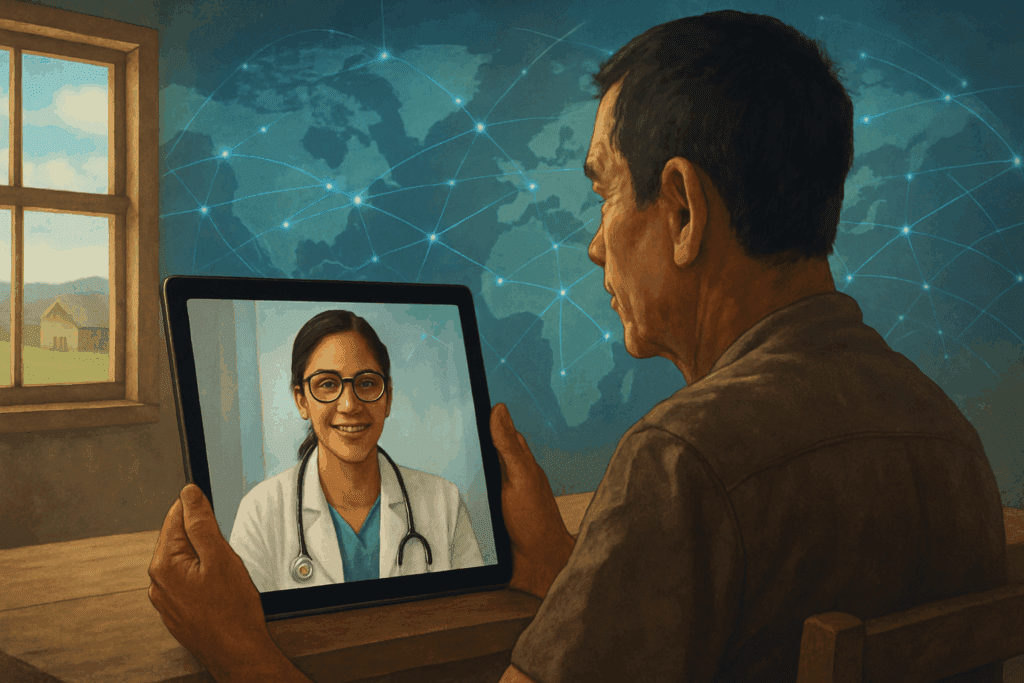
The COVID-19 pandemic catalyzed a surge in telemedicine adoption, but its benefits have proven too significant to abandon. Telehealth platforms offer a convenient and effective alternative to in-person visits, especially for patients in remote or underserved areas. This model of care is not only more accessible, but also cost-effective and efficient, minimizing wait times and reducing strain on healthcare facilities.
More importantly, telemedicine fosters a new kind of continuity in patient-provider relationships. Regular virtual check-ins enable timely management of chronic diseases, post-operative follow-ups, and mental health support. Combined with secure data transmission and integrated health records, virtual consultations can be as informative and personalized as face-to-face encounters. As the new market of health care technology continues to expand, telemedicine will undoubtedly remain a central pillar in delivering equitable, scalable, and patient-centric care.
Precision Medicine and Genomics: Targeted Therapies for Individual Patients
One of the most promising outcomes of recent medical technology is the rise of precision medicine—an approach that tailors medical treatment to the individual characteristics of each patient. At its core, precision medicine harnesses data from genetic profiles, lifestyle habits, and environmental exposures to customize care. This paradigm shift enables more effective interventions with fewer side effects, as treatments are designed to target specific molecular mechanisms.
Genomics plays a foundational role in this model. Advances in sequencing technologies have made it possible to identify mutations that predispose individuals to certain conditions, guiding both prevention and treatment. In oncology, for example, targeted therapies based on tumor genetics have revolutionized the management of cancers such as melanoma, lung, and breast cancer. This shift represents a movement away from one-size-fits-all medicine and toward a future where therapy is as unique as the patient receiving it.
The Ethical and Regulatory Dimensions of Medical Innovation
As with any rapid technological advancement, the integration of new medical tech raises critical ethical and regulatory questions. Issues of data privacy, consent, and algorithmic bias demand careful consideration. The collection and analysis of personal health data—whether from EHRs, wearable devices, or genomic sequencing—must be handled with the utmost responsibility. Regulatory frameworks must evolve in tandem with technology to ensure that patient rights are protected without stifling innovation.
Additionally, questions around equitable access must remain front and center. While urban hospitals may have the resources to implement cutting-edge tools, rural or low-income communities often lack the infrastructure or funding to benefit from these advancements. Addressing these disparities will require coordinated efforts among policymakers, technology developers, and healthcare providers to create scalable and inclusive solutions that serve all segments of the population.
What’s the New Market of Health Care Technology and Who’s Leading It?
The new market of health care technology is characterized by rapid innovation, increasing investment, and a competitive ecosystem of startups, established companies, and academic institutions. Venture capital is flowing into digital health, artificial intelligence, and biotechnology at unprecedented rates, signaling strong confidence in the future of tech-driven care. Companies such as Apple, Google, and Amazon are actively expanding their footprint in healthcare, offering platforms and devices that merge consumer tech with clinical utility.
Simultaneously, biotech firms are developing advanced diagnostic tools, gene-editing technologies, and regenerative medicine therapies that hold the potential to revolutionize treatment paradigms. Startups specializing in remote monitoring, AI diagnostics, and patient engagement platforms are gaining traction, often partnering with healthcare systems to pilot and scale their innovations. As this ecosystem matures, it is creating fertile ground for interdisciplinary collaboration and shaping the trajectory of medicine for decades to come.
Challenges and Considerations in Implementing Emerging Technologies
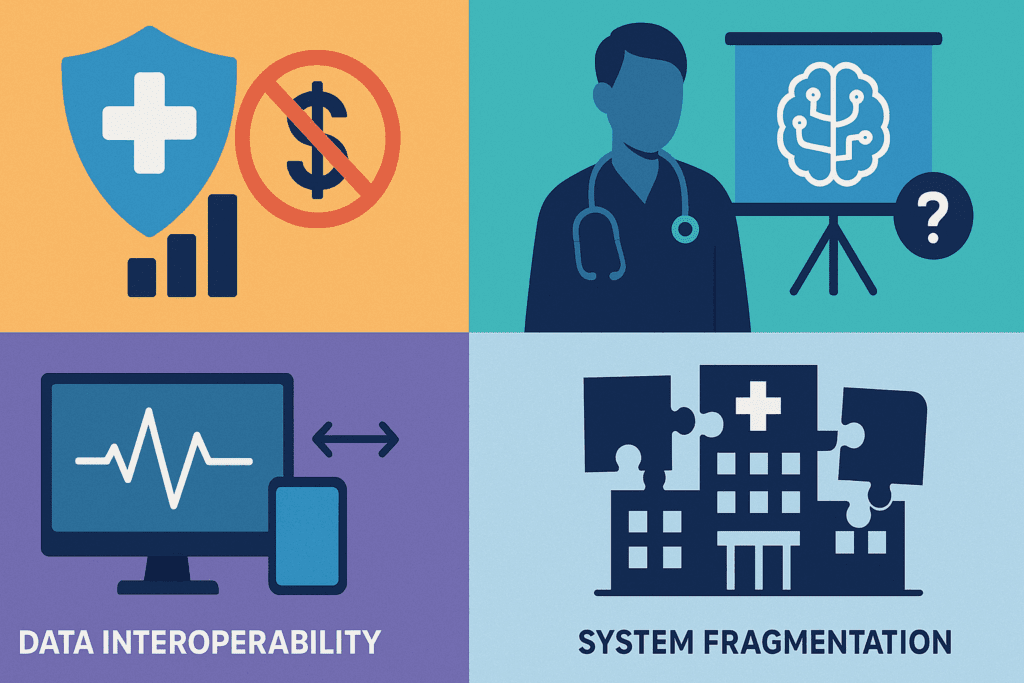
Despite the enthusiasm surrounding recent medical technology, implementation is not without challenges. Financial constraints, workforce training, interoperability issues, and resistance to change all pose significant barriers. Health systems must invest not only in infrastructure but also in education and change management to ensure successful adoption. Providers need training to interpret AI outputs, manage wearable data, and navigate telehealth platforms effectively.
Moreover, ensuring interoperability—the seamless exchange of information across disparate systems—remains a major hurdle. Fragmented data silos can lead to redundancy, miscommunication, and suboptimal outcomes. Collaborative efforts to standardize platforms and promote data sharing are essential to unlocking the full potential of new medical tech. By addressing these challenges head-on, the healthcare industry can pave the way for a smoother, more integrated digital transformation.
A Glimpse Into the Future: Predictive and Preventive Healthcare
Looking ahead, the most profound impact of emerging technology may lie not in treating illness but in preventing it altogether. Predictive analytics, powered by machine learning and big data, can identify at-risk individuals before symptoms arise. Such systems can draw upon a wide range of inputs—genetic data, lifestyle patterns, environmental exposures, and social determinants of health—to generate risk scores and recommend preventive actions.
This shift from reactive to proactive care represents a fundamental transformation in the philosophy of medicine. Rather than waiting for disease to manifest, clinicians and patients alike can intervene early, reducing both the human and economic toll of chronic conditions. Combined with behavioral nudges, remote monitoring, and personalized health coaching, predictive systems offer a path toward truly preventive healthcare—one that is empowered, informed, and deeply human.
Frequently Asked Questions: Exploring the Expanding Role of Technology in Modern Healthcare
1. What are some lesser-known benefits of integrating new medical tech into routine clinical workflows?
While most discussions around new medical tech emphasize improvements in diagnosis and treatment, one overlooked benefit is the enhancement of interdisciplinary collaboration. For example, integrated data platforms allow primary care physicians, specialists, and pharmacists to work from a single, comprehensive health record. This unified access fosters more cohesive care planning and reduces medical errors caused by fragmented communication. Moreover, some institutions are using machine learning to optimize hospital logistics, including operating room schedules and bed assignments, improving operational efficiency without compromising patient care. As new medical tech becomes increasingly embedded in daily practice, it can quietly but significantly streamline the behind-the-scenes processes that sustain effective healthcare delivery.
2. How is recent medical technology changing the doctor-patient relationship beyond digital appointments?
Recent medical technology is redefining the doctor-patient dynamic by emphasizing shared decision-making and empowering patients through data transparency. Tools such as patient portals, home monitoring devices, and AI-generated summaries provide individuals with a clearer understanding of their condition and treatment options. As a result, consultations are becoming more collaborative, with patients playing a more active role in their care plans. Additionally, virtual second-opinion platforms and AI symptom checkers allow patients to seek guidance from a variety of sources before committing to a treatment path. This shift toward informed engagement nurtures trust and mutual respect in the medical relationship, marking a meaningful evolution in patient-centered care.
3. What’s the new market of health care technology doing to promote preventive medicine?
What’s the new market of health care technology is increasingly focused on predictive and preventive approaches that identify risks before symptoms arise. Innovations like AI-driven risk models, mobile health applications, and genomic screening tools are designed to anticipate chronic conditions such as heart disease or diabetes. This proactive model enables earlier lifestyle interventions and reduces the need for aggressive treatments later on. Insurance providers are beginning to incentivize the use of wearable devices that track physical activity, heart rate, and sleep, rewarding patients for maintaining healthier habits. As the market continues to evolve, prevention is becoming not only a clinical goal but also a financially strategic imperative for providers and patients alike.
4. Are there any psychological implications associated with the widespread use of wearable health tech?
The rise of wearable technology introduces nuanced psychological effects that are not often discussed. While many users feel empowered by constant health tracking, others experience anxiety from data overload or become fixated on minor fluctuations in their metrics. This phenomenon, known as the “quantified self” paradox, can create a dependency on validation through numbers rather than subjective well-being. Healthcare professionals must now be prepared to guide patients through interpreting their data constructively. As wearable devices become a standard part of recent medical technology, balancing self-awareness with psychological resilience will be essential for promoting healthy relationships with these tools.
5. How are hospitals and clinics adapting their infrastructure to support new medical tech?
To accommodate new medical tech, healthcare facilities are undergoing architectural and IT transformations. This includes reconfiguring spaces to support telemedicine consults, upgrading servers for real-time data processing, and implementing cybersecurity measures to protect patient information. Cloud-based systems and AI-powered analytics are also being integrated into daily workflows, requiring staff training and ongoing technical support. Additionally, hospitals are forming partnerships with tech firms to ensure seamless integration of tools such as smart beds, connected diagnostic devices, and autonomous delivery robots. These infrastructural shifts reflect a broader trend of healthcare becoming more digitized, interconnected, and responsive to patient needs.
6. How does recent medical technology influence the global accessibility of advanced care?
Recent medical technology is playing a crucial role in leveling the playing field between urban and rural healthcare environments. Portable diagnostic tools, cloud-based medical records, and mobile health units are extending quality care to regions previously lacking access. In developing countries, smartphone-based ultrasound devices and low-cost telemedicine platforms are bridging gaps in maternal care and chronic disease management. Multilingual AI interfaces are also emerging to break down language barriers, allowing providers to serve diverse populations effectively. This democratization of healthcare through technology is one of the most promising trends in global public health, illustrating the far-reaching impact of innovation beyond high-tech hospital settings.
7. What challenges arise when scaling recent medical technology in smaller practices or community clinics?
Small practices and community health centers often face unique barriers to adopting recent medical technology, primarily due to limited budgets and technical expertise. Unlike large hospital systems, these facilities may struggle with the upfront costs of devices, software licensing, and staff training. Moreover, interoperability challenges can be more pronounced when integrating new tools with legacy systems. There is also a learning curve associated with interpreting AI-generated insights, which may require hiring or consulting with specialized personnel. However, many tech companies are beginning to develop scaled-down, affordable versions of their products specifically tailored for smaller providers, signaling a shift toward more inclusive innovation.
8. How are health tech startups influencing what’s the new market of health care technology?
Health tech startups are acting as catalysts within what’s the new market of health care technology by introducing nimble, user-focused solutions that often outpace legacy systems. These startups typically concentrate on niche problems—such as medication adherence, remote patient engagement, or AI triage—and offer agile platforms that can be rapidly tested and iterated. Their presence stimulates competition and encourages established companies to adopt more patient-friendly and interoperable designs. Additionally, partnerships between startups and academic institutions are leading to breakthroughs in areas like digital therapeutics and mental health applications. These new entrants are not just responding to the market; they are actively shaping its trajectory.
9. What ethical dilemmas are emerging alongside advances in new medical tech?
As new medical tech becomes more sophisticated, ethical concerns around consent, data ownership, and algorithmic transparency are intensifying. For instance, patients may unknowingly agree to share sensitive health data through third-party apps without fully understanding the implications. Additionally, predictive models used in diagnostics can inherit biases from training data, leading to skewed outcomes for marginalized populations. There are also questions about how much autonomy should be granted to AI in decision-making, particularly in life-or-death scenarios. Healthcare institutions must establish robust governance policies that prioritize patient rights while ensuring the responsible use of technology. Ethics committees and independent audits are becoming increasingly important in maintaining public trust.
10. What’s next for recent medical technology in terms of long-term societal impact?
The long-term impact of recent medical technology extends beyond clinical outcomes to influence workforce dynamics, healthcare economics, and public health strategy. Automation may reshape job roles within hospitals, shifting the demand toward tech-savvy professionals and reducing reliance on administrative labor. Economically, value-based care models will likely accelerate as insurers use technology to reward prevention over intervention. On a societal level, data-driven insights could guide urban planning, nutrition policy, and epidemic response, creating a more holistic approach to wellness. While the benefits are vast, these changes will require careful planning to avoid unintended consequences such as over-reliance on machines or widening digital divides. Ultimately, the societal influence of medical tech will be shaped by how thoughtfully we manage its integration.
Conclusion: Navigating the Future of Care Through Innovation and Integrity
The journey into the new market of health care technology is not merely a technological transition—it is a redefinition of what it means to care for another human being. From AI-powered diagnostics to genomics-driven treatment plans, recent medical technology is reshaping the contours of clinical practice, making it more precise, personalized, and proactive. These advancements are not abstract concepts but real tools transforming patient outcomes and enriching the lives of both caregivers and recipients.
As we embrace the promise of new medical tech, we must do so with a commitment to the principles of EEAT—Experience, Expertise, Authoritativeness, and Trustworthiness. The ethical stewardship of innovation, the promotion of equitable access, and the cultivation of informed, collaborative care will define the next era in medicine. By staying grounded in these values, we can ensure that the future of healthcare is not only technologically advanced but also profoundly humane.
In the years to come, the healthcare field will continue to witness extraordinary shifts fueled by innovation. The fusion of science, compassion, and technology offers a blueprint for a system that is not only more efficient and effective but also more empathetic and inclusive. The future of medicine is being written now, and it is our collective responsibility to shape it with vision, integrity, and purpose.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Exploring New Medical Devices for Improved Patient Care
Transformative Frontiers: A Comprehensive Review of Emerging Technologies in Modern Healthcare
Transformative Frontiers: A Comprehensive Review of Emerging Technologies in Modern Healthcare
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.