High blood pressure, also known as hypertension, has long been considered a condition predominantly affecting older adults. However, in recent years, an increasing number of young people in their twenties have found themselves facing a diagnosis that was once deemed uncommon for their age group. The question that echoes across clinics and online health forums is clear: why do I have high blood pressure in my 20s? The answer is complex, multifaceted, and rooted in a convergence of lifestyle habits, genetic predispositions, environmental factors, and often, silent warning signs that go unnoticed until the condition has progressed.
For those who are 24 with high blood pressure or experiencing hypertension at 21, the concern is not merely about numbers on a blood pressure cuff. It speaks to a broader issue surrounding the evolving nature of cardiovascular health in younger demographics. This article delves deeply into the underlying causes, emerging patterns, and implications of high blood pressure in early adulthood, offering evidence-based insight and practical strategies for both prevention and management.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Redefining the Age of Onset: What Age Does High Blood Pressure Start?
The traditional understanding that hypertension is a disease of aging is rapidly shifting. While age remains a significant risk factor, an increasing body of research has revealed that high blood pressure at 22 or hypertension at 24 is not as rare as previously thought. Epidemiological data from major public health studies have shown a steady climb in early-onset hypertension cases, with a pronounced spike in the 20 to 29 age group.
This shift in age of onset can be attributed to multiple converging factors, including the rising rates of obesity, sedentary behavior, and poor dietary habits among younger populations. In fact, lifestyle choices in adolescence and early adulthood often lay the groundwork for cardiovascular issues that manifest in one’s twenties. For young men, high blood pressure in 20s male individuals is particularly concerning, as early hypertension is linked with a significantly higher lifetime risk of cardiovascular disease, stroke, and kidney complications.
The prevalence of hypertension at 27 or 30 reflects more than just a numerical anomaly—it underscores the urgency of re-evaluating health norms and expectations for younger adults. More importantly, it highlights the need for routine screening and awareness campaigns targeted specifically at young populations who may otherwise dismiss early symptoms or fail to seek preventative care.
Why Do I Have High Blood Pressure in My 20s? The Hidden Contributors
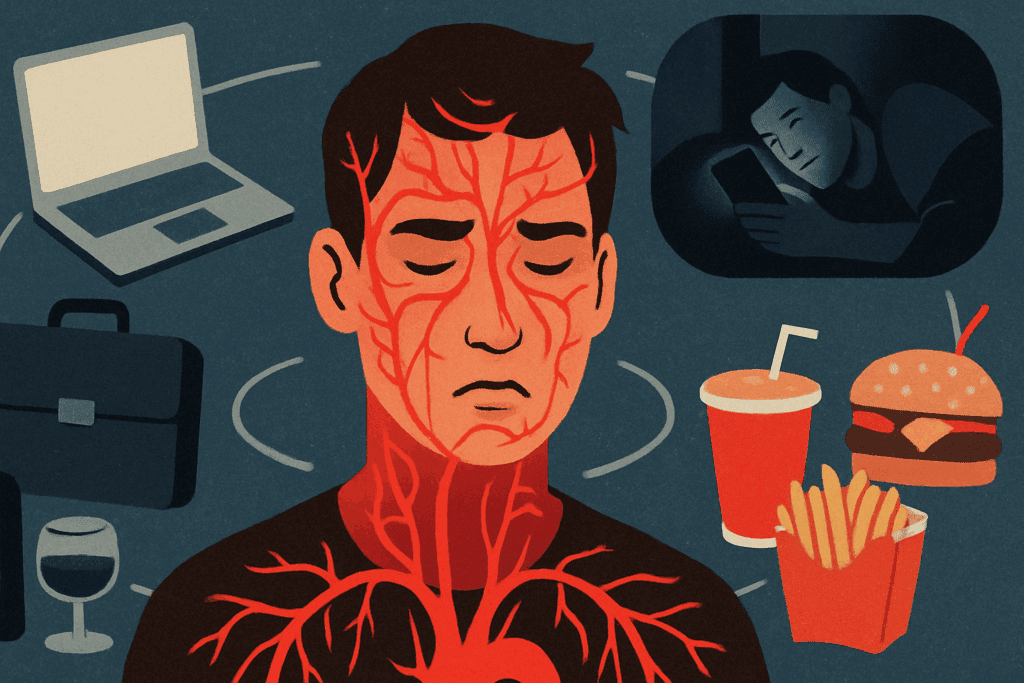
Unraveling the question of why do I have high blood pressure in my 20s requires a nuanced understanding of contributing risk factors that are often overlooked in conventional diagnostics. One of the most prominent culprits is chronic stress. Whether it’s due to academic pressure, career instability, social expectations, or financial stress, chronic activation of the sympathetic nervous system can lead to elevated blood pressure.
Additionally, dietary patterns among young adults often lack the essential nutrients needed for vascular health. High sodium intake, low potassium consumption, and a general deficiency in magnesium and calcium can all contribute to increased vascular resistance. These dietary gaps, combined with high consumption of processed foods, sugar-laden beverages, and alcohol, form a potent recipe for hypertension in young adults.
Another critical but frequently neglected aspect is sleep quality. Sleep deprivation, irregular sleep patterns, and sleep disorders like obstructive sleep apnea have all been independently associated with elevated blood pressure levels. For those experiencing high blood pressure at 25 or younger, exploring sleep hygiene and underlying sleep conditions is an important part of the diagnostic process.
Genetics and Hypertension in Men: An Unavoidable Intersection
While lifestyle plays a pivotal role, the genetic component of high blood pressure cannot be dismissed. Studies have consistently shown that individuals with a family history of hypertension are more likely to develop the condition at a younger age. This genetic predisposition is even more pronounced among males, with hypertension in men emerging earlier and more aggressively than in women.
When a 20 with high blood pressure patient walks into a clinic, clinicians are increasingly encouraged to assess family history with rigor. The presence of inherited metabolic conditions, renal disorders, and abnormalities in blood vessel elasticity can all be part of a genetic predisposition that manifests as early-onset hypertension.
Hormonal factors also contribute to sex-specific risk profiles. Men are often found to have higher baseline blood pressure readings compared to women of the same age, particularly in their twenties and thirties. Coupled with higher rates of smoking and alcohol use, these factors help explain the disproportionate prevalence of hypertension at 30 and similar ages among male patients.
Can You Feel Your Blood Pressure Rise? The Subtlety of Symptoms
One of the most deceptive aspects of high blood pressure is its silent progression. Often called the “silent killer,” hypertension rarely presents with overt symptoms until damage has already occurred to major organs. However, some individuals report subtle cues—feelings of pulsating in the head, mild headaches, dizziness, or palpitations—that may occur during spikes in blood pressure. So, can you feel your blood pressure rise? In some cases, yes, but these sensations are neither universal nor consistent.
This lack of early warning signs means that many people remain unaware of their condition. For those who are 24 with high blood pressure, this absence of symptoms can be dangerously misleading. It often leads to late diagnoses, at which point vascular and organ damage may already be underway. Regular monitoring, especially for individuals with known risk factors, is essential for early detection and management.
Environmental and Sociocultural Influences on Early Hypertension
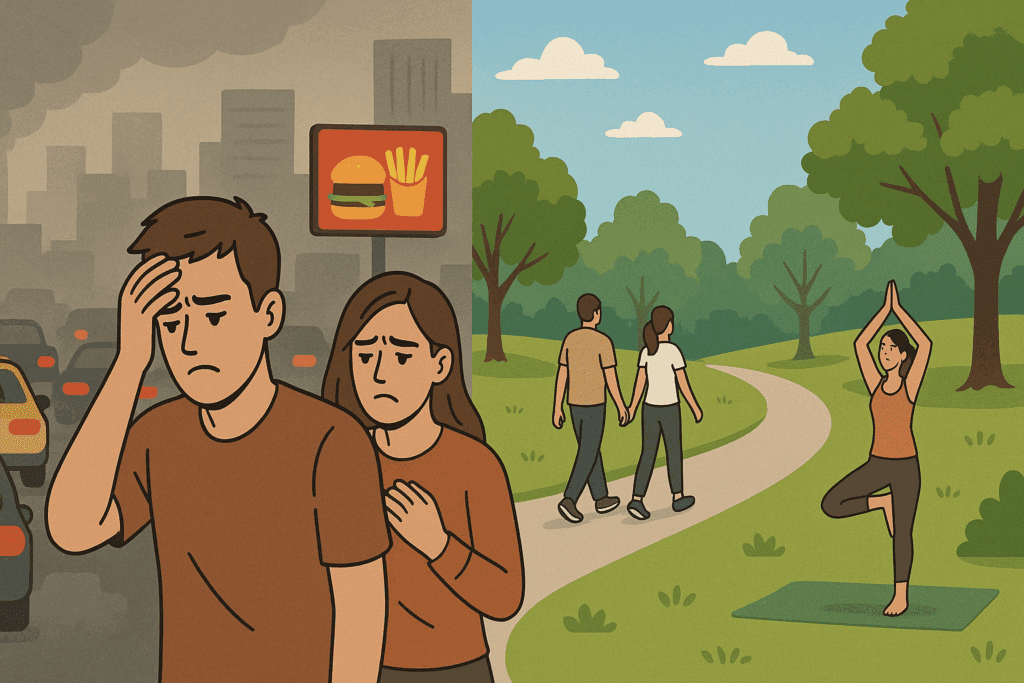
The context in which one lives plays a significant role in cardiovascular risk. Urban environments, with their fast-paced lifestyles, high pollution levels, and limited access to green spaces, contribute to increased stress and reduced opportunities for physical activity. Young adults who live in densely populated cities often experience higher rates of hypertension, partly due to these environmental stressors.
Moreover, cultural norms around diet and activity can either protect against or contribute to the development of high blood pressure. In many cultures, traditional diets rich in fruits, vegetables, and whole grains have been replaced by Western-style eating patterns high in sodium and unhealthy fats. These changes disproportionately affect younger generations, who are more likely to consume convenience foods and skip regular meals.
The issue of high blood pressure at 22 or similar ages cannot be fully understood without considering these broader sociocultural influences. Socioeconomic status, access to healthcare, education, and even neighborhood safety can all shape health outcomes in profound ways. These factors collectively influence why some individuals develop hypertension at 24 while others maintain normal readings well into middle age.
Understanding What Causes High Blood Pressure and Swelling in Young Adults
In some cases, young adults experience not just elevated blood pressure, but also symptoms like swelling in the legs, ankles, or hands. Understanding what causes high blood pressure and swelling is essential for proper diagnosis, as these signs can indicate underlying renal or cardiovascular issues that require medical intervention.
Swelling, or edema, may be linked to poor kidney function, which impairs the body’s ability to regulate fluid and electrolyte balance. High blood pressure can damage the small blood vessels in the kidneys, reducing their efficiency and leading to fluid retention. In such cases, swelling serves as a warning sign that hypertension may be affecting internal organ systems.
Heart failure, although rare in younger adults, is another possible cause. When the heart cannot pump blood effectively, fluid backs up in the body, leading to peripheral swelling. While this is more common in older adults, it should not be ruled out in those with early-onset hypertension, especially if the individual also has a history of congenital heart issues or substance use that could strain cardiac function.
Early Detection and Intervention: The Lifesaving Importance of Awareness
Timely identification of hypertension in young adults is paramount. The earlier the condition is diagnosed and managed, the better the long-term prognosis. Unfortunately, many individuals with high blood pressure in their 20s do not receive regular health checkups. They may dismiss early warning signs or avoid healthcare settings due to cost, lack of insurance, or a general underestimation of their risk.
Routine screenings should be encouraged starting in adolescence, particularly for individuals with a family history of hypertension or other risk factors. Medical professionals are now advocating for blood pressure checks at annual physicals, even in otherwise healthy individuals as young as 18. The data increasingly supports this shift in practice, given the rising incidence of hypertension at 21 or similar ages.
Moreover, the introduction of digital health tools such as home blood pressure monitors and smartphone apps has made it easier than ever to track readings over time. These tools empower young adults to take charge of their health, identify patterns, and share real-time data with their healthcare providers.
Reversing the Trend: Lifestyle Modifications That Matter
Although genetics and environmental factors play critical roles, lifestyle modification remains the most powerful tool for managing and even reversing early hypertension. Regular physical activity—particularly aerobic exercise like walking, running, swimming, or cycling—has been shown to significantly lower blood pressure by improving vascular flexibility and cardiac efficiency.
Diet is equally influential. The DASH (Dietary Approaches to Stop Hypertension) diet, rich in fruits, vegetables, lean proteins, and low-fat dairy, has proven benefits for lowering blood pressure. Reducing sodium intake and avoiding processed foods are particularly important for young adults who are 24 with high blood pressure or experiencing hypertension at 27.
Mind-body interventions such as meditation, deep breathing, and yoga can also be effective, especially for those whose high blood pressure is exacerbated by chronic stress. Sleep hygiene, alcohol moderation, and smoking cessation further enhance the effectiveness of these lifestyle changes. While these measures may not eliminate the need for medication in all cases, they can often reduce dosages or delay the need for pharmacological intervention.
Pharmacological Treatment: When Lifestyle Changes Aren’t Enough
In some cases, lifestyle changes alone are not sufficient to bring blood pressure within a healthy range. This is particularly true for those with a strong genetic predisposition or underlying medical conditions. Pharmacological treatments—including ACE inhibitors, beta blockers, calcium channel blockers, and diuretics—may be necessary to prevent long-term damage.
Treatment decisions must be individualized, taking into account age, comorbid conditions, and the severity of hypertension. Young adults may also have concerns about the long-term use of medication, including potential side effects and impacts on fertility, libido, or mental health. These concerns should be openly discussed with healthcare providers to create a treatment plan that is both effective and sustainable.
Importantly, taking medication for high blood pressure at 25 or 30 does not signify failure. Rather, it is a proactive step in preserving heart health and preventing complications such as stroke, heart attack, and kidney disease. Regular follow-ups and lab tests ensure that the medication continues to work effectively and without causing harm.
Looking Forward: Public Health Implications of Early-Onset Hypertension
The increasing prevalence of high blood pressure in young adults has wide-reaching implications for public health systems. Left unaddressed, this trend could contribute to an epidemic of early cardiovascular disease, placing unprecedented strain on healthcare resources. Policies aimed at promoting heart health must now include strategies tailored to the needs and behaviors of young adults.
Health education in schools, targeted social media campaigns, and community-based health screenings are all promising avenues for reaching this demographic. Moreover, integrating blood pressure monitoring into routine healthcare visits for college students and young professionals could significantly improve early detection rates.
Employers also have a role to play. Workplace wellness programs that encourage physical activity, provide nutritious meal options, and promote mental health can have a meaningful impact on reducing the incidence of hypertension in men and women in their twenties. Through a multi-pronged approach, the tide of early-onset hypertension can be turned.
The Long View: Managing Hypertension at 30 and Beyond
For those who have been diagnosed with hypertension at 30, the journey ahead is one of vigilance and resilience. While the condition is chronic, it is also manageable with the right combination of lifestyle, medication, and monitoring. The key lies in consistency—maintaining healthy habits over time, staying informed about new treatment options, and fostering a collaborative relationship with healthcare providers.
The emotional toll of a chronic diagnosis at a young age should not be underestimated. It is normal to experience frustration, anxiety, or even denial. Support networks—whether through family, friends, or peer groups—can provide invaluable encouragement and motivation. Mental health care, when integrated into the overall management plan, enhances both psychological and cardiovascular outcomes.
Frequently Asked Questions: Early-Onset Hypertension in Your 20s
1. Can stress-related conditions explain why I have high blood pressure in my 20s, even if I’m healthy otherwise?
Yes, chronic stress is increasingly being recognized as a major contributor to early-onset hypertension. Even if you have no visible risk factors, sustained psychological pressure from academic demands, work-life imbalance, or financial insecurity can lead to continuous sympathetic nervous system activation. This can cause temporary spikes in blood pressure that become chronic over time. Individuals who are 20 with high blood pressure or experiencing hypertension at 24 may be unaware that their elevated levels are due to unaddressed stress. Practicing mindfulness, incorporating structured relaxation techniques, and seeking psychological support can be just as essential as diet or exercise in managing blood pressure.
2. If I’m 24 with high blood pressure, could my use of energy drinks or supplements be a factor?
Absolutely. Many energy drinks contain high doses of caffeine and stimulants like guarana, which can lead to temporary increases in blood pressure. When used frequently, these spikes can accumulate and lead to chronic hypertension. This is especially relevant for those experiencing high blood pressure at 22 or high blood pressure at 25, as stimulant tolerance and dependency may develop over time. Additionally, workout supplements containing pre-workout formulas can cause vasoconstriction, further elevating blood pressure. It’s important for young adults to review their intake of these substances if they’ve been diagnosed with hypertension at 21 or later.
3. Can you feel your blood pressure rise, or is it always symptomless?
While high blood pressure is often asymptomatic, some individuals do report subtle sensations during blood pressure spikes. These can include lightheadedness, a throbbing sensation in the head, or facial flushing. However, these signs are not definitive and can easily be misattributed to other conditions like anxiety or dehydration. Individuals with high blood pressure in 20s male populations often mistake these sensations for stress or fatigue. If you suspect you can feel your blood pressure rise, consistent at-home monitoring with a validated cuff is recommended to confirm patterns and verify symptoms.
4. What causes hypertension in young adults who maintain a healthy lifestyle and weight?
Genetic predisposition plays a significant role in early-onset hypertension. Even those with optimal body weight, regular physical activity, and healthy diets may still face elevated readings due to inherited vascular traits, hormone imbalances, or kidney-related issues. For example, secondary hypertension—caused by underlying conditions such as hyperaldosteronism or polycystic kidney disease—often first emerges in individuals experiencing hypertension at 27 or younger. For young adults who are 24 with high blood pressure and no identifiable lifestyle risk, a thorough diagnostic workup is essential to rule out these conditions. Family history and subtle metabolic markers often provide important clues.
5. How is high blood pressure in 20s male populations influenced by alcohol and recreational drug use?
Men in their twenties often face societal norms that promote alcohol consumption and experimentation with recreational drugs, both of which can influence blood pressure. Chronic alcohol use leads to endothelial dysfunction, a process that impairs the blood vessels’ ability to dilate properly, raising baseline blood pressure. Similarly, drugs like cocaine, MDMA, and even cannabis in some users can increase heart rate and vascular resistance. This is particularly concerning for those facing hypertension at 30 or slightly younger, as early vascular damage may go unnoticed. Reducing or abstaining from these substances is a critical part of hypertension prevention in men.
6. Is there a link between what causes high blood pressure and swelling in the legs or hands in young people?
Yes, when high blood pressure begins affecting kidney function or heart performance, fluid regulation in the body can be compromised. This may lead to peripheral swelling, known as edema, which is particularly noticeable in the lower extremities. Young adults who experience both hypertension at 24 and swelling should be evaluated for signs of early renal insufficiency or cardiac dysfunction. It’s also important to investigate whether medications, such as NSAIDs or hormonal contraceptives, may be contributing. What causes high blood pressure and swelling in young adults is rarely one single issue—it’s often a combination of vascular, renal, and pharmacologic influences.
7. How early should routine screening begin if I’m concerned about developing high blood pressure at 22 or earlier?
The ideal time to begin routine screening is late adolescence, especially if you have a family history of hypertension or cardiovascular disease. Annual check-ups that include blood pressure measurements can help establish a personal baseline. This is crucial because what age does high blood pressure start is increasingly skewing younger, particularly in industrialized nations. If you’re already 20 with high blood pressure, your monitoring frequency should increase to every three to six months, depending on your provider’s guidance. Early screening allows for timely intervention before permanent vascular changes or organ stress occur.
8. Are mental health disorders like anxiety and depression linked to high blood pressure at 25 or younger?
Yes, research increasingly shows that untreated anxiety and depression are linked to dysregulation of the autonomic nervous system, leading to sustained elevations in blood pressure. This connection is particularly strong in individuals navigating life transitions, such as college, employment, or early independence, which may coincide with diagnoses of hypertension at 21 or 24. Mental health disorders can also impair sleep, appetite, and self-care behaviors—all of which are risk factors. For those 24 with high blood pressure and underlying anxiety, integrated care involving both mental health and primary care providers is often the most effective strategy.
9. Why is high blood pressure at 25 more concerning than developing it later in life?
Developing hypertension at 25 means that your cardiovascular system may be under sustained pressure for several decades longer than someone who develops it in their 50s. This extended exposure increases the risk of long-term complications such as left ventricular hypertrophy, chronic kidney disease, and stroke. Furthermore, hypertension in men diagnosed in their 20s is associated with a faster progression to end-organ damage compared to women. Early detection and intervention are key to preventing these outcomes. Even modest lifestyle changes can significantly alter the trajectory of someone with hypertension at 27, making early adulthood a crucial intervention window.
10. What new technologies or innovations are helping young adults manage hypertension more effectively?
Digital health has transformed the way young people can track and manage their cardiovascular health. Smartwatches and fitness trackers now offer continuous heart rate monitoring, and some devices even include blood pressure tracking features, though these are still being refined for accuracy. Mobile apps allow for trend tracking, medication reminders, and sharing data directly with healthcare providers. These tools are particularly useful for those wondering why do I have high blood pressure in my 20s when lifestyle appears healthy—trends may reveal hidden contributors like stress or sleep disruption. Wearable tech empowers individuals with hypertension at 30 or earlier to take a more active role in daily management and long-term prevention.
Conclusion: Understanding the Rise of Hypertension in Young Adults and How to Take Control
The question of why do I have high blood pressure in my 20s reflects a broader shift in the landscape of cardiovascular health. With more young adults being diagnosed at 21, 24, 27, and 30, early-onset hypertension is no longer an anomaly—it is a pressing public health concern. Understanding what causes hypertension in young adults, whether it’s genetic, environmental, or behavioral, is the first step in managing and preventing this condition.
From recognizing the silent nature of symptoms to understanding how lifestyle and environment intersect with physiology, this article has explored the many dimensions of high blood pressure in young adults. Whether you are a 20 with high blood pressure individual wondering what comes next, or a 25-year-old looking to reverse the early signs of cardiovascular strain, knowledge is your most powerful ally.
Taking control starts with awareness, but it doesn’t end there. Consistent monitoring, meaningful lifestyle changes, and evidence-based medical care can transform a diagnosis into a manageable part of a long, healthy life. In a world where hypertension at 30 is becoming more common, informed action is not just advisable—it is essential.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Causes of High Blood Pressure in Young Adults
Can I Get Hypertension in My 20s?
Risk Factors Associated With Hypertension in Young Adults: A Systematic Review


