Why Potassium Control Is Crucial for Kidney Health
Managing chronic kidney disease (CKD) requires far more than medication or regular check-ups—it demands strict attention to diet, particularly to potassium intake. As kidney function declines, the body’s ability to regulate potassium diminishes, often leading to dangerous elevations in blood potassium levels. This condition, known as hyperkalemia, poses a serious risk, especially to the heart, where it may trigger arrhythmias or even cardiac arrest. A well-structured low potassium diet for kidney patients becomes essential to avoid these complications while maintaining nutritional adequacy.
Potassium plays critical roles in muscle function, nerve signaling, and cellular hydration. However, with kidney impairment, the very nutrients that typically support health can become liabilities. Therefore, identifying and consistently choosing low potassium foods for kidney patients allows for safer nourishment and helps mitigate the effects of potassium and kidney issues. Strategic dietary choices help manage symptoms, slow disease progression, and maintain a higher quality of life.
You may also like: Is the Keto Diet Safe or Dangerous? What Experts Say About the Risks, Benefits, and Basics of the Ketogenic Diet
How Potassium Affects the Body and Kidney Function
Potassium’s importance in human physiology cannot be overstated—it maintains the heart’s rhythm, ensures smooth muscle movement, and regulates nerve impulses. But when the kidneys lose efficiency in filtering potassium from the bloodstream, levels can accumulate rapidly. Potassium kidney disease scenarios often result in fatigue, numbness, muscle cramps, and potentially fatal arrhythmias if not promptly addressed. These risks make potassium regulation through diet a cornerstone of care for renal patients.
For individuals with impaired kidney function, the daily recommended potassium intake may be drastically lower than that of a healthy person. What complicates matters is that potassium is found in a wide array of otherwise healthy foods, from oranges to potatoes. Without proper knowledge, patients can unknowingly consume excessive amounts. That’s why integrating low potassium vegetables for kidney patients and learning cooking techniques that lower potassium content is so valuable.

Low Potassium Vegetables That Support Kidney Wellness
Vegetables are an essential source of vitamins, fiber, and phytonutrients. But for kidney patients, not all vegetables are equally safe. High-potassium options like spinach, sweet potatoes, and tomatoes should be minimized or carefully prepared. Fortunately, there are several low potassium vegetables for kidney patients that are not only safe but versatile and nutrient-rich.
Cabbage, green beans, cauliflower, bell peppers, zucchini, and cucumber are prime examples of vegetables with low potassium content that fit seamlessly into renal diets. These can be steamed, sautéed, or roasted with kidney-friendly herbs and healthy oils. Boiling or double-boiling can further reduce potassium levels, making previously borderline vegetables safer for occasional consumption. Including these vegetables in daily meals can provide balance, volume, and essential nutrition without contributing to potassium overload.

Navigating Protein Choices with Low Potassium Levels in Mind
Protein is vital for tissue repair, immune function, and overall metabolic health. However, many protein-rich foods, such as dairy products, legumes, and nuts, are also high in potassium, creating a nutritional dilemma for kidney patients. Still, there are effective ways to meet protein requirements using low potassium foods for renal patients.
Lean poultry, fresh fish, and egg whites are excellent low potassium sources of high-quality protein. For those seeking plant-based alternatives, tofu (in limited portions) and specially prepared low potassium diet peanut butter can be viable options. Peanut butter, when consumed in small amounts and chosen wisely from low potassium varieties, can add flavor and protein without exceeding safe potassium limits. It’s critical for patients to read labels, opt for unsalted versions, and consult their renal dietitian about appropriate serving sizes.
What to Eat for a Kidney-Friendly, Low Potassium Breakfast
Breakfast often includes foods that are high in potassium—think bananas, orange juice, or bran cereals. But with planning, a satisfying and safe low potassium breakfast is achievable. Many traditional items can be replaced with renal-friendly alternatives that maintain flavor and variety.
For example, white toast with unsalted margarine, cream of wheat with almond milk, scrambled egg whites, or low-sodium pancakes made from refined flour all align with a low potassium diet. Avoiding processed breakfast meats and juices is also essential. Low potassium breakfast strategies focus on minimizing potassium while ensuring the meal is energy-rich and balanced enough to start the day strong. Patients can also include small servings of safe fruits, such as apples or blueberries, for sweetness and antioxidants.
Kidney-Safe Fruits for Low Potassium Diets
Fruits often pose a dilemma: while they are packed with vitamins and antioxidants, many are high in potassium. For patients managing potassium and kidney issues, it’s important to know which fruits to limit and which to embrace.
Fortunately, several fruits for low potassium diets can be safely enjoyed. Apples, pears, grapes, plums, strawberries, and peaches (especially when canned in natural juice) are generally safe options. These fruits provide hydration, fiber, and natural sweetness without threatening potassium control. On the other hand, patients should avoid or limit bananas, melons, oranges, and avocados, as these tend to be potassium-rich. Serving size remains essential, as even low potassium fruits can add up if consumed in excess.
Cooking Techniques to Lower Potassium in Foods
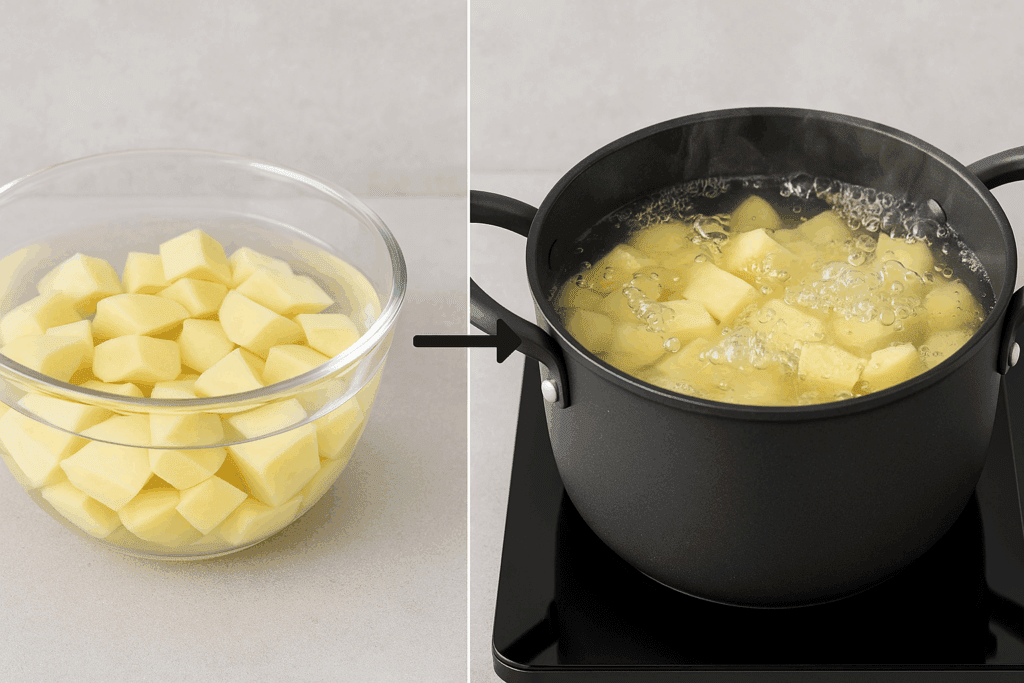
Beyond choosing the right ingredients, how food is prepared significantly affects its potassium content. Some high potassium foods can be made safer through specific preparation methods, offering more flexibility in diet.
Leaching, for example, involves soaking vegetables like potatoes or squash in water to draw out potassium before cooking. Boiling vegetables rather than steaming or baking them can also help reduce potassium levels. For patients struggling to let go of familiar favorites, these methods can provide a compromise. A potato soaked overnight and boiled may contain far less potassium than one that is simply baked. Learning these techniques empowers patients to adapt their diets without feeling deprived.

Reading Labels and Avoiding Hidden Sources of Potassium
In today’s food environment, hidden potassium sources abound, particularly in processed and convenience foods. Potassium-based additives—especially potassium chloride—are used as salt substitutes and preservatives. These are often found in low-sodium versions of canned soups, sauces, frozen meals, and even sports drinks. Despite good intentions, patients may unknowingly increase their potassium intake when opting for these items.
Reading ingredient labels carefully becomes essential. Any additive beginning with “potassium” should raise a red flag. This is especially important for patients on dialysis or those in later stages of kidney disease. Being proactive and vigilant in grocery store aisles can make a significant difference in managing potassium levels. Education around label literacy is a powerful tool in supporting patient independence and long-term dietary success.
The Role of Hydration and Lifestyle in Potassium Regulation
Diet is foundational, but managing potassium and kidney issues requires a broader lifestyle approach. Hydration is one key factor. In earlier stages of kidney disease, adequate fluid intake helps the kidneys flush excess potassium. However, fluid restrictions may apply for patients with advanced kidney failure or those on dialysis, making individualized guidance essential.
Exercise also supports overall health and can improve potassium regulation when paired with appropriate medical care. Medication adherence, routine lab work, and open communication with a nephrologist and renal dietitian create a multi-faceted care strategy. All of these elements work in tandem, but food remains the constant and most controllable variable—particularly when potassium management is a concern.
Adapting Traditional Cuisines to Low Potassium Needs
Cultural and regional food traditions often present both opportunities and challenges for those on a low potassium diet. Many global cuisines rely heavily on high-potassium staples like plantains, tomatoes, legumes, and root vegetables. Adapting these recipes without sacrificing identity or enjoyment requires creativity and collaboration with dietitians who understand both medical nutrition therapy and cultural context.
For example, a stew traditionally made with yams and tomatoes can be modified using cabbage and green beans with garlic and herbs to maintain flavor while lowering potassium content. Renal dietitians often help patients modify cherished recipes, reinforcing the idea that food can remain joyful even within dietary boundaries. Maintaining cultural continuity in meals enhances adherence and supports mental well-being.
Supporting Emotional Wellness While Managing a Kidney-Friendly Diet
The psychological and emotional toll of dietary restrictions should not be underestimated. For many patients, being told to give up favorite foods or entire food groups is not only frustrating—it can feel isolating. Anxiety around eating, social events, and fear of making mistakes may emerge. Addressing these concerns with compassion is as important as nutritional education.
Support groups, counseling, and compassionate care models that integrate emotional and behavioral support improve long-term success. Encouraging patients to focus on what they can eat rather than what they can’t, and celebrating small victories, reinforces a positive mindset. The ultimate goal is sustainability, not perfection, and patients should feel empowered, not punished, by their dietary choices.
The Future of Potassium Management in Kidney Care
Medical science continues to explore new ways to optimize nutrition for kidney patients. Advances in gut microbiome research may eventually provide solutions that influence potassium absorption or excretion. Until such breakthroughs become widely available, patients and clinicians must rely on established dietary guidelines and emerging clinical evidence.
A low potassium diet for kidney patients remains a medically sound, evidence-backed approach. When combined with lifestyle adjustments, emotional support, and regular monitoring, it enables people with kidney disease to live healthier, fuller lives. Empowering patients with knowledge, resources, and support is the foundation of successful potassium management.
Frequently Asked Questions (FAQ) on Low Potassium Foods for Kidney Patients
1. Can a low potassium diet for kidney patients support other aspects of health beyond potassium control? Yes, a well-structured low potassium diet for kidney patients can also support cardiovascular health, reduce fluid retention, and improve overall energy levels. Since many low potassium foods for kidney patients are also naturally lower in sodium and saturated fats, they contribute to healthier blood pressure and reduced strain on the heart. Moreover, by encouraging whole, unprocessed foods, this diet often increases the intake of dietary fiber, which supports digestive health. The key is ensuring the diet is still nutritionally balanced—rich in essential vitamins and moderate in protein—to prevent deficiencies that can emerge with overly restrictive eating. When managed properly, this type of renal diet not only protects against potassium and kidney issues but can also enhance total wellness.
2. How can patients make low potassium breakfasts more enjoyable and varied? Creativity plays a major role in transforming a low potassium breakfast into a satisfying and varied meal. Swapping in safe starches like white bread, refined oats, or low-potassium pancakes paired with low-fat cream cheese or jam (without potassium additives) can introduce new textures and flavors. Many people on a low potassium diet for kidney patients overlook aromatic herbs and citrus zest, which can add depth without increasing potassium content. Incorporating fruits for low potassium like berries or sliced apples can elevate taste and nutritional value. Rotating options every few days and experimenting with new kidney-safe recipes is essential to avoiding breakfast fatigue while maintaining compliance.
3. Are there new developments in food labeling that help identify low potassium foods for renal patients more easily? Yes, recent advocacy efforts have led to improved labeling regulations in some regions, making it easier to identify low potassium foods for renal patients. Some brands now highlight “renal-friendly” or “low potassium” directly on the front of packaging, particularly in frozen meals or plant-based products. Additionally, digital tools and apps have emerged that scan barcodes and provide instant potassium content feedback. For those managing potassium kidney disease, learning how to interpret not only the Nutrition Facts panel but also the ingredients list is vital. Potassium-based preservatives like potassium chloride may be hidden, so advanced literacy in label reading empowers patients to make safer choices confidently.
4. Can low potassium diet peanut butter be included daily in a kidney patient’s eating plan? While moderation is key, low potassium diet peanut butter can be incorporated several times a week if portion sizes are monitored and phosphorus content is also considered. Many patients mistakenly believe all peanut butter is off-limits, but newer formulations have emerged specifically for individuals with potassium and kidney issues. These products often use less processed peanuts, remove added salts, and are labeled as renal-friendly. A serving of about one tablespoon, paired with white toast or low potassium fruits, makes for a convenient and protein-rich snack. Still, patients should consult their renal dietitian to ensure compatibility with their individualized potassium targets.
5. Are there seasonal fruits that fit into a low potassium diet for kidney patients? Absolutely. Each season offers a variety of fruits for low potassium that can align with the needs of a kidney patient. In spring, strawberries and blueberries are excellent options; in summer, you might enjoy apples, pears, and plums; fall offers cranberries and certain types of grapes; and winter brings canned peaches (in natural juice) or frozen berries. Choosing seasonal produce not only adds freshness and variety to meals but also often makes them more affordable. These fruits, when eaten in appropriate portions, provide flavor and nutrients without overwhelming the kidneys, making them staples in many low potassium diets.
6. What role does portion control play in consuming low potassium vegetables for kidney patients? Portion control is crucial, even when selecting low potassium vegetables for kidney patients. Many vegetables considered “low potassium” only remain so if consumed within specific serving sizes. For example, half a cup of cooked green beans is typically safe, but doubling the portion could approach or exceed safe potassium levels. Patients must be mindful of how vegetables are prepared—boiling can reduce potassium, while roasting or baking retains more of the mineral. Meal planning with a dietitian helps create personalized serving guides that account for both variety and cumulative potassium intake throughout the day.
7. How do low potassium foods for kidney patients affect medication management? Dietary potassium intake can directly influence how certain medications function in patients with kidney disease. For example, some blood pressure medications, like ACE inhibitors or potassium-sparing diuretics, can raise potassium levels independently of diet. When combined with high-potassium foods, this can increase the risk of hyperkalemia. By following a low potassium diet for kidney patients, the likelihood of dangerous drug-nutrient interactions is reduced. Doctors may also adjust medication doses based on blood potassium trends, underscoring the importance of consistent dietary adherence and lab monitoring.
8. Can low potassium breakfast options support blood sugar regulation in diabetic kidney patients? Yes, selecting the right low potassium breakfast can play a significant role in managing blood glucose levels, especially in diabetic kidney patients. Opting for slow-digesting carbohydrates such as refined oats or white toast with a source of protein like egg whites or low potassium diet peanut butter can provide stable energy without large glucose spikes. Pairing these meals with fruits for low potassium, like sliced berries, adds natural sweetness and fiber. Avoiding sugary cereals, processed pastries, or potassium-enriched milk alternatives is also important. A carefully balanced breakfast supports both glycemic control and kidney function.
9. What are common mistakes patients make when transitioning to low potassium foods for renal patients? One of the most common mistakes is assuming that all fresh produce is automatically healthy without considering potassium content. Another error is relying too heavily on processed “low sodium” products, many of which substitute sodium with potassium-based preservatives. Some patients also overconsume “safe” foods, not realizing that large portions of even low potassium vegetables for kidney patients can accumulate quickly. Forgetting to re-check food labels periodically for reformulations is another pitfall. A successful transition to low potassium foods for renal patients often involves retraining shopping habits, learning to portion meals properly, and seeking professional guidance.
10. Are there potential innovations on the horizon that could make potassium management easier for kidney patients? Yes, the future holds promising developments. Research is underway into potassium-binding agents that may allow more dietary flexibility in potassium and kidney issues. Additionally, biotech companies are exploring genetically modified crops with reduced potassium content, potentially offering new low potassium vegetables for kidney patients. Personalized nutrition platforms using AI may soon deliver real-time feedback based on individual lab results, helping patients select appropriate meals daily. As food labeling laws become more transparent, renal patients will likely benefit from smarter packaging and clearer indicators. These advancements could significantly ease the burden of dietary potassium management while preserving nutritional quality and quality of life.
Conclusion: Embracing Low Potassium Nutrition for Kidney Health and Quality of Life
Successfully managing kidney disease involves many moving parts, but none are as constant or as critical as diet. A carefully planned, well-executed low potassium diet for kidney patients is not about deprivation—it’s about empowerment. Through informed choices, strategic meal planning, and a strong support network, individuals can maintain safe potassium levels and enjoy satisfying meals that support overall health.
Low potassium foods for kidney patients—from vegetables like cabbage and cauliflower to fruits for low potassium diets like apples and berries—offer both safety and variety. Building meals around these staples ensures better outcomes while maintaining joy in eating. Whether incorporating low potassium breakfast options or selecting low potassium diet peanut butter for a snack, every food decision matters.
Most importantly, understanding potassium and kidney issues doesn’t stop with a list of dos and don’ts. It’s an ongoing journey of learning, adapting, and thriving. With guidance from healthcare providers and a willingness to embrace change, kidney patients can navigate this journey with strength, knowledge, and the confidence that they are taking the right steps toward better health.
Further Reading:
Low-Potassium Diet: What to Know
Kidney Disease and Potassium: How to Create a Kidney-Friendly Diet


