For individuals managing chronic kidney disease (CKD), nutrition becomes more than just a matter of taste or routine; it becomes a crucial component of therapy. As kidney function declines, the body struggles to eliminate excess waste and fluids, making a specialized diet not only helpful but often essential. That’s where a carefully structured renal diet menu plan comes in. This article explores what a doctor-recommended 7 day meal plan for kidney disease entails, how to approach each day with purpose, and what a renal diet menu should truly look like to support better kidney health. From balancing nutrients to crafting satisfying, flavorful meals, we dive deep into the world of kidney-friendly nutrition, anchored in medical accuracy and tailored guidance.
You may also like: Is the Keto Diet Safe or Dangerous? What Experts Say About the Risks, Benefits, and Basics of the Ketogenic Diet
Understanding the Importance of a Renal Diet for CKD Management
The kidneys are vital organs tasked with filtering the blood, excreting waste through urine, and maintaining electrolyte and fluid balance. When they begin to fail, as in CKD, waste products such as urea and creatinine can accumulate in the body. This can lead to symptoms like fatigue, nausea, swelling, and high blood pressure. By adhering to a renal diet meal plan, patients can significantly reduce the workload on their kidneys, alleviating symptoms and slowing disease progression.
A kidney disease diet plan is not a one-size-fits-all approach. Nutrient restrictions vary depending on the stage of kidney disease, presence of comorbidities such as diabetes or hypertension, and individual lab results. However, in general, a renal diet emphasizes reduced sodium, potassium, and phosphorus intake, along with controlled protein consumption. This dietary framework helps manage symptoms while preserving remaining kidney function. Thus, the best diet for kidney disease is personalized yet grounded in scientifically established principles of renal nutrition.
What Is a Kidney Diet and How Does It Work?
When patients ask, “What is a kidney diet?” they’re often surprised to learn it is not just about avoiding salt. The kidney diet menu plan is multifaceted, targeting several nutrients that are normally excreted by healthy kidneys. Key among these are sodium, potassium, phosphorus, and protein. Each plays a different role in the body, but all must be balanced carefully when kidney function is impaired.
For example, excess sodium can increase blood pressure and fluid retention, contributing to swelling and further kidney damage. Potassium, while essential for muscle and nerve function, can accumulate dangerously in CKD, leading to cardiac issues. Phosphorus is another mineral that tends to build up in advanced kidney disease, causing bone weakness and vascular calcification. Protein, while necessary for tissue repair and immune function, produces waste that overburdens the kidneys. A renal diet aims to strike a delicate balance, allowing patients to receive necessary nutrients without further compromising renal health.

Components of a Successful Renal Diet Menu Plan
Building a renal diet menu plan requires thoughtful consideration of nutrient content, meal timing, and patient preferences. A successful plan includes renal diet breakfast, lunch, and dinner options that are low in sodium, moderate in protein, and carefully portioned for potassium and phosphorus. The meals should be satisfying and easy to prepare, enabling patients to adhere to dietary guidelines consistently.
Beyond macronutrients and minerals, hydration also plays a role. Some patients with advanced CKD or on dialysis may need to restrict fluid intake, while others may benefit from increased hydration to help flush waste. Therefore, each kidney diet menu plan must be reviewed regularly by a registered dietitian or nephrologist to adapt to the patient’s changing needs.
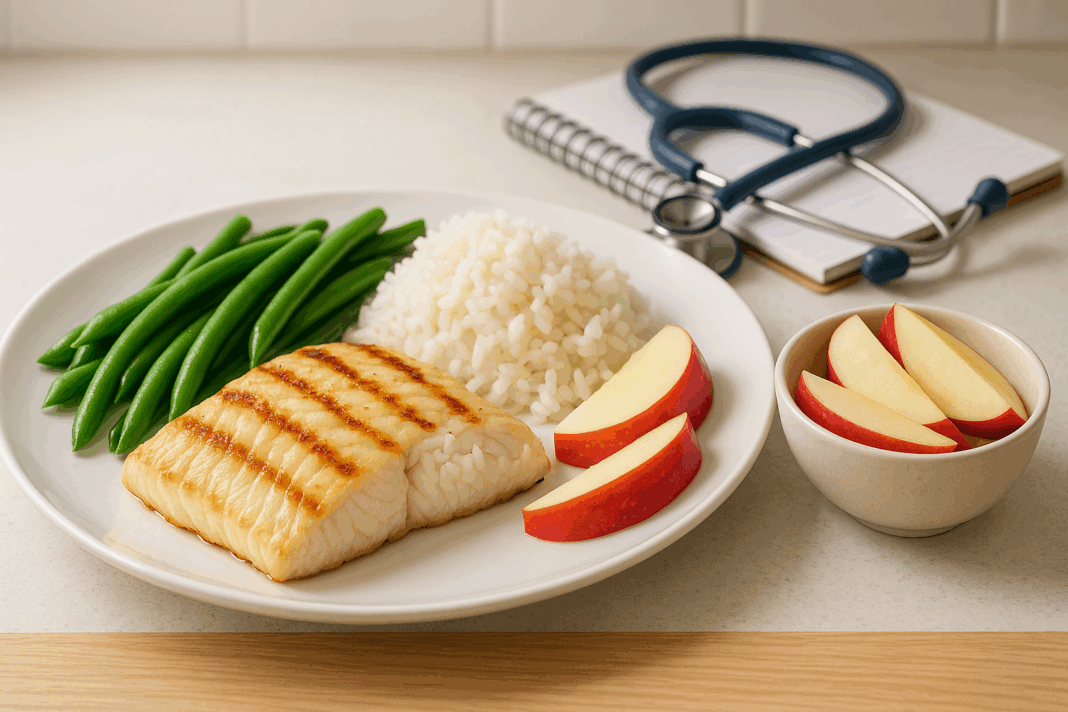
What Makes a Meal Kidney-Friendly? Practical Applications
Renal diet meals are more than just bland, restrictive dishes. With proper planning, they can be flavorful, diverse, and enjoyable. A kidney-friendly meal typically includes a small portion of high-quality protein, such as egg whites, skinless poultry, or fish. Vegetables are chosen carefully, favoring low-potassium options like cauliflower, zucchini, and bell peppers. Grains such as white rice, pasta, and refined breads are often preferred over whole grains due to their lower phosphorus content.
To keep sodium in check, herbs and spices like rosemary, thyme, garlic powder (not salt), and lemon juice are excellent alternatives to salt. Cooking methods also matter; steaming, grilling, or baking foods without added salt preserves flavor while reducing unnecessary additives. Dairy, nuts, and processed foods should be consumed in limited quantities or avoided altogether, depending on lab results. These practical strategies transform the renal diet from a limitation into an empowering tool for kidney health.
Tailoring a Renal Diet Menu for Potassium Control
Potassium control is often one of the most critical elements in a kidney disease diet plan. While many fruits and vegetables are naturally high in potassium, careful selection can enable patients to enjoy variety without risk. A 7 day meal plan for low potassium diet emphasizes produce like apples, grapes, cabbage, and green beans, while avoiding bananas, oranges, potatoes, and tomatoes.
Cooking techniques can also reduce potassium content. For instance, double boiling high-potassium vegetables—boiling them in water, draining the water, and then boiling again—can leach out significant amounts of potassium. While this does reduce some of the nutrient density, it allows patients to safely enjoy a wider variety of foods. Regular monitoring of potassium levels through blood tests is essential, and dietary adjustments should be made accordingly under medical supervision.
In contrast, some patients may struggle with low potassium levels due to medications or dialysis. In such cases, a 7 day meal plan for high potassium diet may be recommended. This plan can include nutrient-dense foods like sweet potatoes, spinach, avocados, and bananas, but only when prescribed by a healthcare provider.
Planning a Full Week: 7 Day Meal Plan for Kidney Disease
Designing a 7 day meal plan for kidney disease requires more than plugging foods into a calendar. It involves structuring meals that offer variety, balance, and practical convenience. Each day should include a renal diet breakfast, lunch, and dinner, along with appropriate snacks when needed. The renal diet menus should avoid redundancy to minimize taste fatigue, a common challenge in long-term dietary adherence.
For example, a Monday breakfast might include scrambled egg whites with white toast and a serving of blueberries, followed by a lunch of grilled chicken salad with lettuce, cucumbers, and a vinaigrette dressing. Dinner could feature baked tilapia, white rice, and steamed green beans. Over the week, protein sources can be rotated among lean poultry, fish, and plant-based options like tofu. Grains and vegetables can also be varied within potassium and phosphorus limits. A renal diet menu that offers daily change while meeting nutritional guidelines helps foster long-term success.
Best Diet for Renal Disease: Evidence-Based Approaches
The best diet for renal disease is grounded in evidence-based nutrition science and individualized patient care. Numerous studies have demonstrated the benefits of low-protein diets supplemented with keto analogs, as well as plant-dominant diets with proper monitoring. While some patients benefit from vegetarian kidney diet menu plans, others require more animal-based proteins due to specific nutritional needs.
Medical nutrition therapy (MNT) delivered by a registered renal dietitian is a cornerstone of CKD management. MNT helps patients understand food labels, plan meals, and manage symptoms like swelling or nausea. Adherence to a kidney diet menu plan has been associated with improved lab values, delayed dialysis initiation, and better quality of life. These findings underscore the value of well-structured renal diet meals as more than a recommendation—they become a form of medical treatment in themselves.

Avoiding Common Pitfalls in Renal Diet Planning
Despite good intentions, many patients unknowingly consume foods that can worsen kidney function. Common pitfalls include relying on “healthy” options like whole grains, dairy, or nuts that are often high in phosphorus and potassium. Without proper guidance, patients may also overlook hidden sodium in condiments, canned goods, or restaurant foods. Learning to read nutrition labels and prepare meals at home helps avoid these risks.
Another challenge is protein quality and quantity. Patients may consume too much protein, thinking it’s needed for strength, or too little, leading to muscle loss. The ideal renal diet meal plan carefully calibrates protein intake to match the patient’s stage of CKD. It’s also important to manage fluid intake and avoid dehydration or fluid overload. A successful kidney disease diet plan is one that adapts as the disease progresses, supported by frequent consultation with a healthcare provider.
The Role of Breakfast, Lunch, and Dinner in a Renal Diet
A well-balanced day begins with a thoughtful renal diet breakfast. Skipping breakfast can lead to energy crashes and poor food choices later in the day. A suitable morning meal might include cream of wheat, low-sodium toast with jam, and apple slices. This combination provides energy without overwhelming the kidneys.
Lunch and dinner should aim to balance protein, carbohydrates, and low-potassium vegetables. A kidney diet menu plan might include lunch options like turkey sandwiches with iceberg lettuce and a side of unsalted crackers, while dinner could feature pasta with garlic-infused olive oil and sautéed zucchini. Ensuring that all three meals align with dietary restrictions helps maintain energy levels and reduce metabolic stress. Snacks, when permitted, should be nutrient-dense yet kidney-friendly, such as unsalted popcorn or fresh berries.
Finding the Best Foods for Kidney Health
Determining the best food for kidney health depends on the stage of CKD, individual lab values, and personal taste preferences. However, general recommendations include low-potassium fruits like apples and grapes, low-sodium grains like white rice and pasta, and lean protein sources such as egg whites or chicken breast. Certain herbs and spices also offer flavor without adding phosphorus or sodium, making them excellent additions to the renal diet menus.
Limiting or avoiding phosphorus-rich foods is especially important, as phosphorus can accumulate in the bloodstream and lead to bone and cardiovascular complications. This includes avoiding cola beverages, packaged meats, and most dairy products. Instead, plant-based alternatives with lower phosphorus absorption rates, like rice milk (phosphate-free) and certain tofu products, can be safely included. These choices reflect how the best diet for renal disease is built on informed, strategic decisions about every ingredient.
How to Customize a Kidney Diet Menu Plan for Individual Needs
No two patients with CKD are exactly alike. Therefore, the kidney diet menu must be customized to align with individual health status, lifestyle, and cultural preferences. A vegetarian might lean more on tofu and rice-based dishes, while another patient may benefit from fish and white poultry. Likewise, someone with diabetes must consider carbohydrate content alongside potassium and phosphorus restrictions.
The key is adaptability. A renal diet menu plan that is overly rigid can cause frustration, leading to dietary noncompliance. Collaborating with a renal dietitian helps strike the right balance between restriction and enjoyment. Patients should also learn how to swap ingredients based on seasonal availability or personal preference while staying within dietary boundaries. Such flexibility is essential to creating a sustainable and effective kidney disease diet plan.
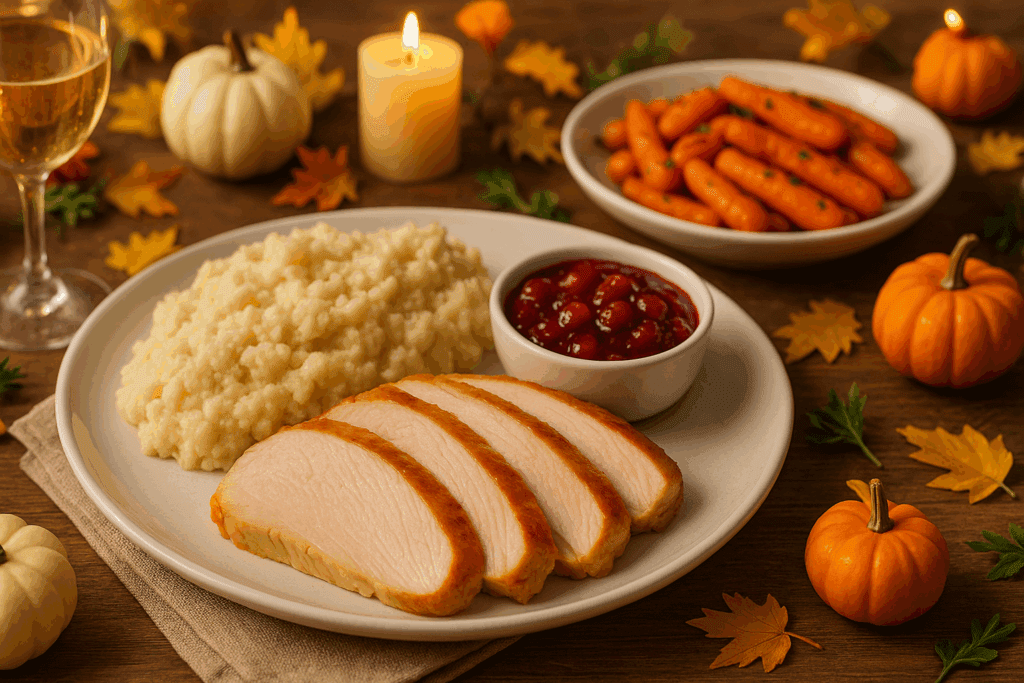
Rethinking Traditional Meals with a Renal-Friendly Twist
Cultural and family traditions are an important part of eating, but many traditional dishes may not align with the goals of a renal diet. Fortunately, it’s possible to adapt recipes without sacrificing flavor. For example, a traditional meatloaf can be prepared with ground turkey instead of beef and seasoned with onion powder and herbs rather than salt. Mashed potatoes, often high in potassium, can be replaced with mashed cauliflower.
Even holiday meals can be made renal-friendly with a little planning. Turkey without skin, cranberry sauce made from fresh berries with minimal sugar, and stuffing with white bread and celery can create a satisfying meal that supports diet for kidney health. These adaptations allow patients to remain socially connected while still prioritizing their health.
The Importance of Education and Ongoing Support
Sticking to a renal diet menu requires more than access to the right foods—it requires knowledge, motivation, and support. Patients who understand the “why” behind their restrictions are more likely to adhere to them. Educational sessions, printed meal guides, and support groups all contribute to better long-term outcomes. Empowering patients to make informed decisions transforms passive dietary compliance into active self-management.
Regular follow-ups with a nephrologist and renal dietitian help ensure that the renal diet meal plan remains aligned with current health needs. Adjustments may be required due to changes in lab values, medication, or lifestyle. By treating dietary planning as a dynamic, ongoing process, patients are better equipped to manage their CKD.
Frequently Asked Questions: A Doctor-Recommended 7 Day Meal Plan for Kidney Disease
1. Can a renal diet menu plan improve mental clarity and reduce fatigue in people with kidney disease? Yes, following a structured renal diet menu plan can have noticeable effects on cognitive clarity and energy levels in individuals with CKD. When waste products like urea and creatinine accumulate due to poor filtration, they can affect neurological function and contribute to a persistent mental fog. A targeted renal diet meal plan helps regulate electrolyte imbalances, stabilizes blood sugar, and reduces inflammation—factors that directly influence mood, concentration, and stamina. Patients often report feeling more alert and less sluggish after consistently following a 7 day meal plan for kidney disease. Additionally, including brain-supportive ingredients that fit the kidney diet menu plan, such as omega-3-rich fish (in moderation) or berries, further supports mental performance.
2. How does a 7 day meal plan for low potassium diet help prevent emergency complications in advanced CKD? Managing potassium through a 7 day meal plan for low potassium diet is essential for patients at risk of hyperkalemia, a potentially life-threatening condition. Excess potassium can lead to irregular heart rhythms, muscle weakness, and in severe cases, cardiac arrest. A proactive kidney disease diet plan limits high-potassium foods while ensuring adequate nutrition through carefully selected alternatives like green beans, apples, and rice. It also supports medication efficiency, as certain phosphate binders and diuretics interact with dietary minerals. Customizing a renal diet menu with proper potassium control offers a preventive layer that reduces emergency hospital visits and maintains cardiovascular safety in daily life.
3. What are some social challenges people face when adhering to a kidney diet menu in group settings or cultural traditions? Following a kidney diet menu plan during social events or cultural meals can be challenging due to traditional ingredients that may be high in salt, potassium, or phosphorus. Social stigma or peer pressure may lead individuals to compromise their renal diet menus, risking setbacks in their CKD management. Planning ahead by bringing renal diet meals to gatherings, or communicating dietary needs with hosts, can help maintain both health and inclusion. Creative adaptations of traditional dishes—such as using cauliflower mash instead of high-potassium mashed potatoes—can allow individuals to enjoy meals without deviation from their renal diet meal plan. Support groups or forums tailored to CKD patients can offer valuable strategies for navigating these social complexities.
4. Are there emerging technologies or apps that can assist with tracking a renal diet breakfast lunch dinner routine? Yes, there are several digital tools now designed to help patients stay consistent with their renal diet breakfast lunch dinner schedules. These tools often include barcode scanning for grocery items, potassium and phosphorus tracking, and customized renal diet menu alerts based on lab values. Mobile apps like MyNetDiary and RenalTracker allow users to log their 7 day meal plan for kidney disease and receive real-time feedback on nutrient levels. Some also sync with lab portals, helping users adjust their kidney diet menu as their bloodwork changes. Integrating technology with a CKD diet plan can empower patients to take more control over their health while maintaining dietary precision.
5. Can patients combine a kidney diet menu plan with intermittent fasting or time-restricted eating? Yes, but with caution and professional guidance. Intermittent fasting may offer metabolic benefits, but those with kidney disease must approach it differently than the general population. Skipping meals may lead to excessive protein intake in fewer sittings, which can burden the kidneys even within a renal diet meal plan. For patients who wish to explore fasting, a modified approach—such as a 10-hour eating window with evenly spaced renal diet meals—might be safer. Coordination with a renal dietitian is essential to ensure that nutrient needs are still met and that the kidney diet menu remains balanced throughout the restricted time frame.
6. How can caregivers support someone managing a renal diet menu plan without overwhelming them? Caregivers play a pivotal role in supporting adherence to a renal diet menu without becoming overbearing. Instead of micromanaging meals, caregivers can assist by preparing shopping lists based on a CKD diet plan, pre-portioning meals for the week, or helping with label reading during grocery trips. Encouraging autonomy in meal choices within the renal diet breakfast lunch dinner framework fosters dignity and long-term compliance. It’s also helpful for caregivers to learn basic renal nutrition concepts so they can offer support without imposing. Emotional encouragement, especially during times of diet fatigue, is as vital as logistical support in helping maintain a healthy 7 day meal plan for kidney disease.
7. Is the best diet for kidney disease different for individuals on dialysis compared to those in earlier CKD stages? Absolutely. The best diet for kidney disease shifts significantly once a patient begins dialysis. While pre-dialysis patients often follow a low-protein renal diet menu plan, those on dialysis typically require higher protein intake to compensate for losses during treatment. Phosphorus and potassium control remain critical, but fluid and sodium restrictions may intensify. A dialysis-specific kidney diet menu plan may also include protein supplements and carefully timed meals to align with treatment sessions. Therefore, it is crucial to reassess renal diet meals regularly with a healthcare provider to reflect the evolving needs at different CKD stages.
8. What role do herbal and alternative therapies play in a kidney disease diet plan? Although alternative therapies can complement conventional treatment, they must be approached cautiously in the context of a kidney disease diet plan. Some herbs and supplements, like licorice root or high-dose turmeric, can interfere with blood pressure, electrolyte balance, or medication metabolism. That said, certain plant-based ingredients—such as ginger or cinnamon—can offer anti-inflammatory benefits and be safely included in a renal diet menu if approved by a healthcare professional. Integrating these within a kidney diet menu plan should always be supervised by a nephrologist or dietitian to avoid toxicity. Importantly, herbal preparations must not replace the foundational role of a structured CKD diet plan and renal diet menu plan.
9. How can patients avoid palate fatigue when following a strict renal diet menus regimen? Renal diet fatigue is common, especially when options seem limited. Combatting this involves rotating herbs and spices, exploring international low-potassium recipes, and trying new cooking techniques like air-frying or pressure cooking. Seasonal meal adjustments within the renal diet menu plan keep it fresh and psychologically rewarding. Using visual variety—colorful produce within safe limits, for example—enhances appetite and satisfaction. Incorporating a new dish every week into a 7 day meal plan for kidney disease helps prevent monotony while still aligning with dietary goals. The goal is to make the best diet for renal disease both effective and enjoyable for the long term.
10. What strategies help ensure a diet plan for kidney failure is sustainable during periods of illness or appetite loss? Periods of illness or appetite loss can make it difficult to maintain a consistent diet plan for kidney failure. During these times, nutrient-dense small meals or smoothies tailored to renal diet restrictions can help meet calorie and protein requirements without overwhelming the stomach. Working with a dietitian to develop contingency meals that align with the renal diet breakfast lunch dinner framework can be invaluable. Flavor enhancers like lemon juice or garlic-infused oils can stimulate appetite without increasing sodium. Finally, maintaining hydration with low-potassium clear fluids is critical—especially during fevers or gastrointestinal episodes—to preserve kidney function while following the best food for kidney health.
Conclusion: Building a Renal Diet Menu Plan That Supports Lifelong Kidney Health
A well-structured 7 day meal plan for kidney disease does more than manage symptoms—it provides a roadmap to a healthier, more stable life. By embracing a renal diet menu that includes breakfast, lunch, and dinner options tailored to each stage of CKD, patients can actively participate in their treatment. From understanding what a kidney diet entails to selecting the best food for kidney health, the journey requires knowledge, discipline, and support.
With a personalized kidney diet menu plan, patients can enjoy flavorful meals while maintaining control over sodium, potassium, phosphorus, and protein intake. Whether creating renal diet meals for low potassium needs or adapting traditional recipes for kidney-friendly options, the best diet for renal disease is one that evolves with the individual. By integrating medically sound guidance with practical, enjoyable strategies, the renal diet becomes not a burden, but a tool for empowerment and lasting wellness. Through collaboration with healthcare professionals and a commitment to learning, patients can transform dietary therapy into a powerful ally in the fight for better kidney health.
Further Reading:
Build Your 7-Day Meal Plan for Kidney Disease: Breakfast, Lunch, Dinner and Everything in Between
Diabetes and Kidney Disease: What to Eat?
7-Day Meal Plan for Kidney Disease: Foods that Make Both Your Kidneys and Taste Buds Happy