The Rise of Robotic Precision in Modern Surgery
In the vast expanse of medical innovation, few advancements have reshaped the clinical landscape as profoundly as surgical robotics. Initially viewed as futuristic or experimental, robots used in surgery are now considered indispensable in many modern operating rooms. The emergence of these sophisticated systems has redefined the boundaries of what is surgically possible, enabling procedures that are more precise, less invasive, and increasingly tailored to the individual patient. From cardiac interventions to intricate neurosurgical operations, the applications of robotic technologies are not only expanding—they are transforming our understanding of surgical care.
You may also like: Advancements in Healthcare Technology: How Emerging Innovations Are Transforming Patient Care
The evolution of surgical robots has been driven by a convergence of engineering ingenuity, computer science, and clinical necessity. As patient outcomes continue to improve with robotic-assisted interventions, hospitals and research institutions worldwide are investing heavily in developing, refining, and adopting these technologies. For patients, this evolution means quicker recoveries, reduced complication rates, and greater access to cutting-edge treatment options. But to appreciate the full impact of robotic surgery, it is essential to explore both the history and the ongoing revolution these technologies represent.
Understanding the Different Types of Surgical Robots
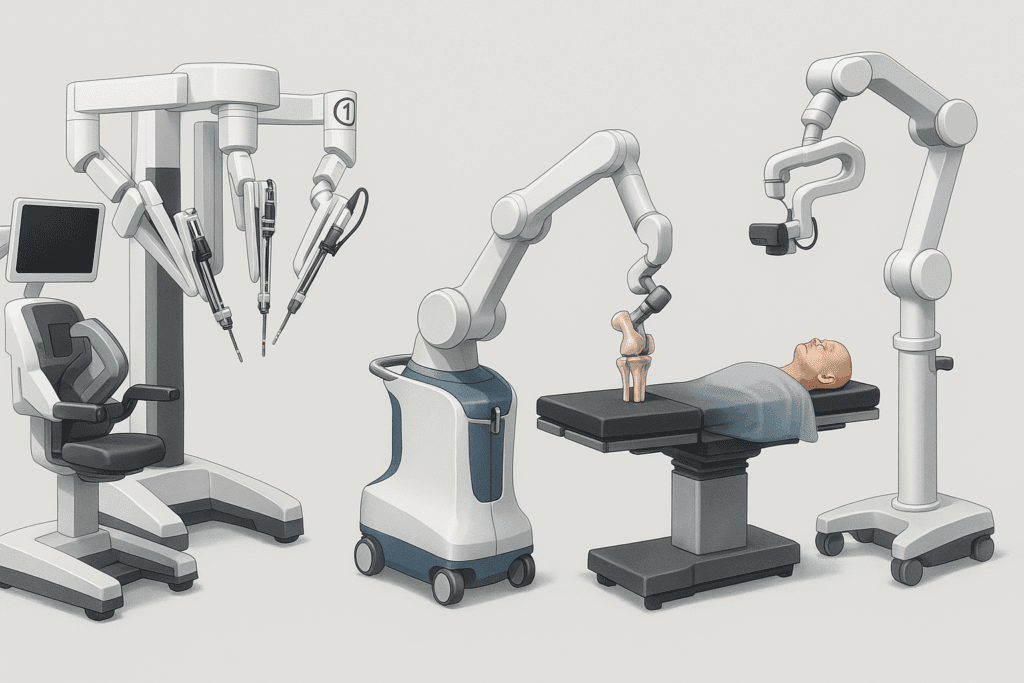
As the field of robotic surgery expands, so too does the taxonomy of machines that define it. Understanding the various types of surgical robots is critical not only for healthcare professionals but also for patients seeking to make informed decisions about their care. The most prominent systems fall into several distinct categories, each designed with specific capabilities tailored to particular types of procedures.
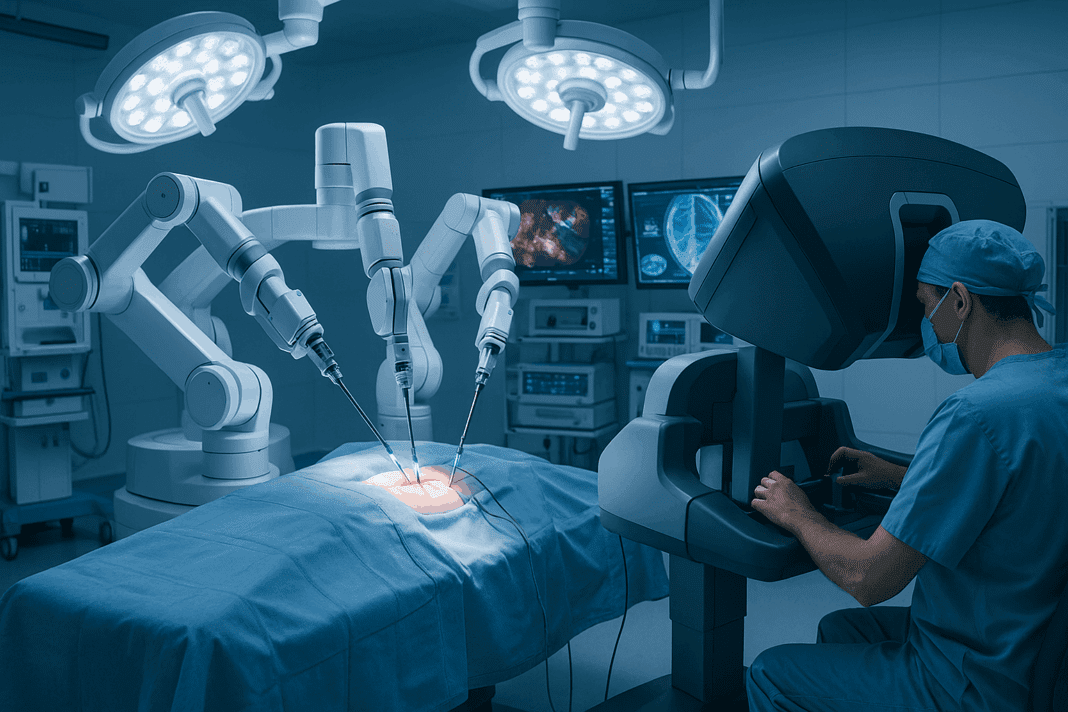
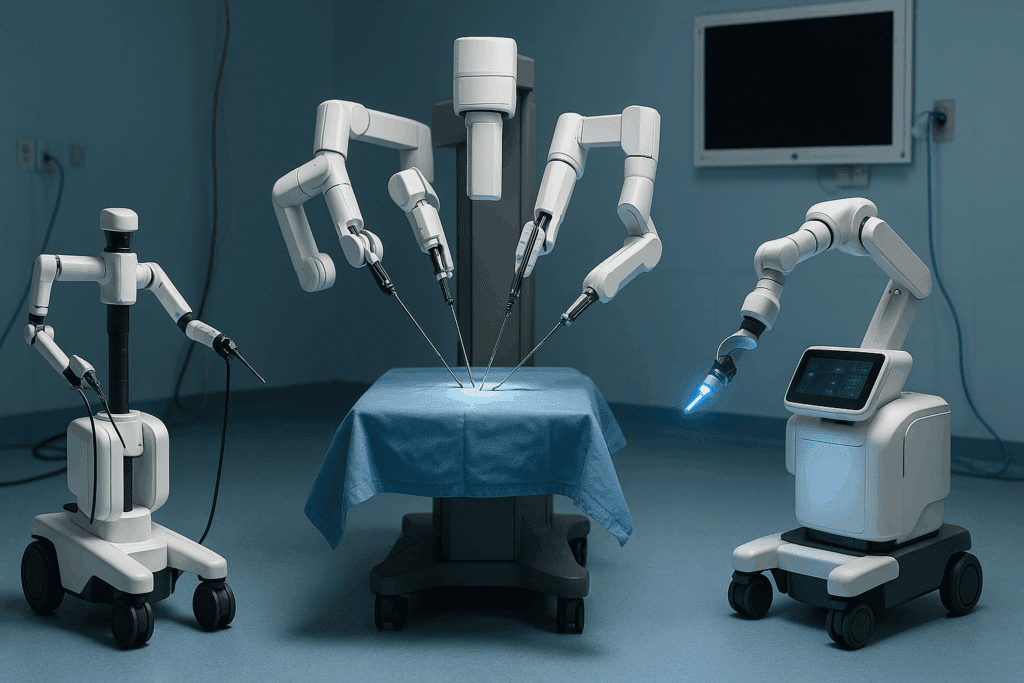
One of the most widely recognized types of surgical robots is the robotic-assisted laparoscopic system. These machines, such as the da Vinci Surgical System, use articulated arms controlled remotely by a surgeon seated at a console. The robotic arms replicate the surgeon’s hand movements with exceptional precision, enabling minimally invasive surgeries through tiny incisions. This system has become synonymous with robotic surgery examples in urology, gynecology, and general surgery.
Another class of robots used in surgery includes orthopedic robotic platforms like the MAKO system. These devices are specifically engineered to assist in joint replacement procedures, such as knee or hip arthroplasty. By integrating preoperative imaging with intraoperative navigation, they allow for millimeter-level accuracy in bone alignment and implant positioning. In neurosurgery, robotic systems like ROSA and NeuroMate facilitate stereotactic procedures, offering unparalleled precision in brain surgery. These systems are particularly valuable in complex cranial operations, where even the slightest deviation can have significant consequences.
The diversity in the types of surgical robots illustrates the growing specificity and adaptability of these technologies. As researchers and manufacturers continue to refine their designs, the future promises even more specialized machines tailored to niche medical needs, potentially revolutionizing everything from spinal surgery to organ transplantation.
Surgery Robot Names That Are Leading the Industry
A deeper look into the most impactful systems reveals a list of surgery robot names that have become synonymous with excellence in modern medicine. These names are not just branding tools; they represent comprehensive platforms designed to meet the rigorous demands of advanced surgical care. Among the most widely known is the da Vinci Surgical System, developed by Intuitive Surgical. This system has become the gold standard in robotic-assisted minimally invasive procedures and has been adopted by thousands of hospitals worldwide.
Another prominent entry is the MAKO Robotic-Arm Assisted Surgery System, which has revolutionized orthopedic surgery. Its advanced planning software allows surgeons to create detailed surgical blueprints tailored to each patient’s anatomy. This personalized approach significantly enhances procedural accuracy and postoperative outcomes. Also noteworthy is ROSA, developed by Zimmer Biomet, which is used in both neurosurgical and orthopedic applications. Its versatility and precision have made it a valuable tool in complex brain surgeries as well as total knee replacements.
The ExcelsiusGPS system, created by Globus Medical, has emerged as a frontrunner in robotic spine surgery. Its integration of real-time imaging and robotic guidance provides unparalleled control in spinal instrumentation, which is essential for reducing surgical complications and improving alignment accuracy. Other surgical robots names gaining attention include CyberKnife for robotic radiosurgery and Monarch for robotic bronchoscopy. Each of these systems brings unique capabilities to specific areas of medicine, further underscoring the multifaceted role of robotics in healthcare.
As hospitals and clinics seek to enhance their surgical offerings, the recognition of trusted surgery robot names becomes a key factor in procurement decisions. These names carry weight not only because of their technological prowess but also due to their established records of safety, efficacy, and improved patient outcomes.
Real-World Robotic Surgery Examples and Their Clinical Impact
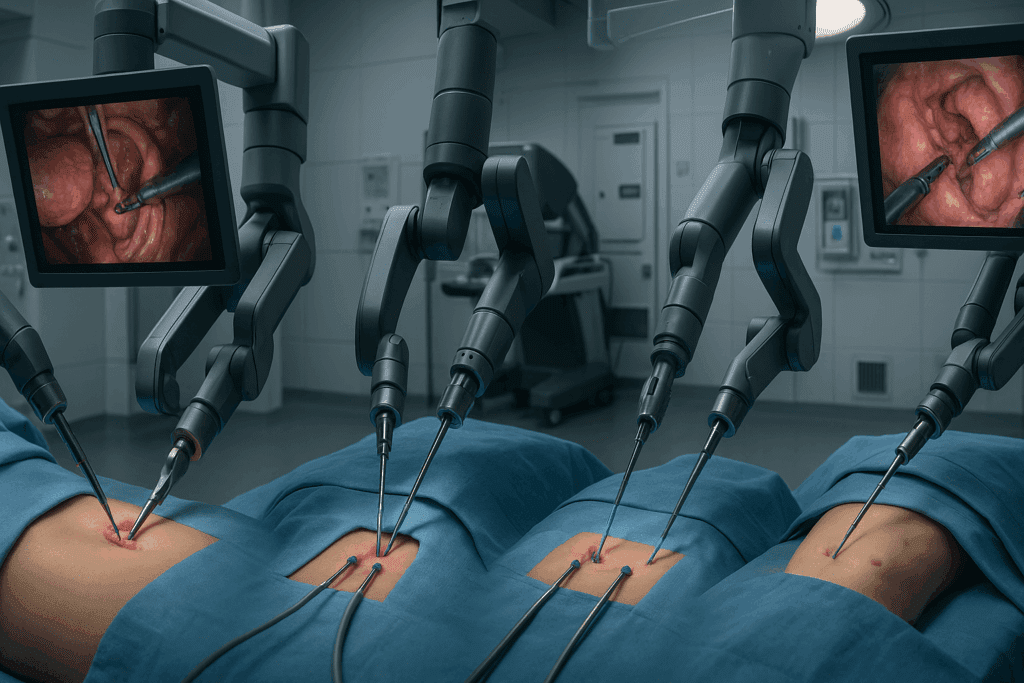
To fully appreciate the capabilities of robots used in surgery, it is essential to examine real-world scenarios where these technologies have significantly altered the course of treatment. One of the most common robotic surgery examples is prostatectomy, particularly the removal of the prostate gland in patients with prostate cancer. Traditional open surgery for this condition often involved large incisions and lengthy recovery times. With robotic assistance, surgeons can perform the procedure through small ports, resulting in less blood loss, quicker recovery, and improved preservation of urinary and sexual function.
Cardiothoracic surgery has also seen tremendous benefits from robotic interventions. In mitral valve repair, for example, robotic systems allow for the precise manipulation of delicate cardiac tissues, something that would be nearly impossible with traditional instruments. This has led to fewer postoperative complications and shorter hospital stays. Similarly, robotic hysterectomies have become a preferred approach for many gynecologists due to the enhanced visualization and control offered by robotic platforms.
Another compelling application involves colorectal surgeries, particularly for rectal cancer. Navigating the narrow confines of the pelvic cavity is notoriously challenging, but robotic systems offer the dexterity needed to operate effectively in these tight spaces. Pediatric surgery has also embraced robotics, with systems adapted for smaller anatomical structures and the unique needs of children. Across all these specialties, the consistent theme is the transformative impact of robotic precision on patient care.
By examining these robotic surgery examples, it becomes evident that these technologies are not simply upgrades to existing tools. Rather, they represent a paradigm shift in surgical philosophy—one that prioritizes precision, minimizes trauma, and embraces individualized care.
The Engineering Behind Robots Used in Surgery
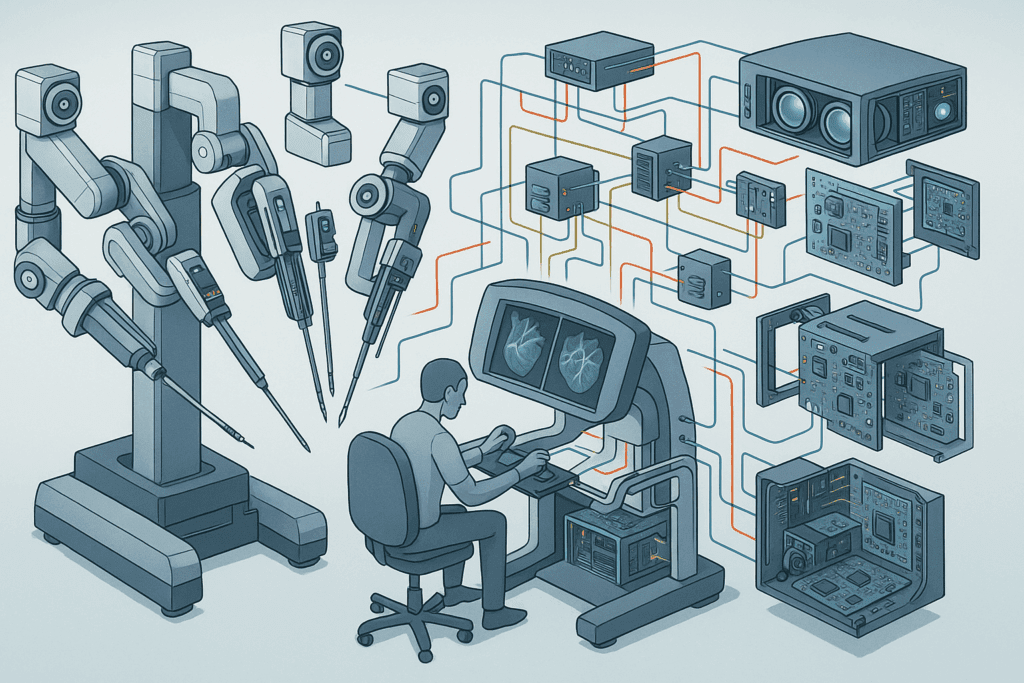
The marvels of modern surgical robots are not just feats of medicine but also engineering masterpieces. Behind every robotic arm lies a symphony of technologies that converge to create seamless interaction between human operators and machine assistance. The core of this interaction is the surgeon’s console, a sophisticated interface that translates human movements into micro-movements performed by robotic arms. These movements are not only highly accurate but also free from tremors, a critical advantage in delicate procedures.
Robotic systems rely on a combination of actuators, sensors, and advanced software algorithms to execute commands with near-perfect fidelity. Haptic feedback, for example, allows the surgeon to “feel” tissue resistance, even though they are not physically touching the patient. This tactile feedback is crucial for distinguishing between different tissue types and ensuring safe dissection. Furthermore, the integration of 3D high-definition cameras provides magnified, immersive views of the surgical field, enhancing the surgeon’s spatial awareness and decision-making.
What sets these machines apart from traditional surgical tools is their adaptability. Engineers have designed these robots to be modular, allowing for upgrades and customization based on specific procedural needs. Innovations in artificial intelligence are also beginning to play a role, enabling robots to suggest optimal cutting paths, alert surgeons to potential complications, and even execute basic tasks autonomously under supervision. As machine learning algorithms continue to improve, we may soon see robots that can learn from every procedure, continuously refining their techniques to improve future outcomes.
This intricate interplay of mechanical engineering, software development, and biomedical innovation ensures that robots used in surgery are not static machines but evolving partners in patient care.
Surgical Robots Names You Should Know in Academic and Clinical Research
While the commercial landscape of surgical robots is dominated by a few major players, academic and clinical research institutions are continually developing new systems that push the boundaries of what is possible. These emerging surgical robots names may not yet be household terms, but they are shaping the future of robotic medicine in significant ways.
One such innovation is the Versius Surgical Robotic System, developed by CMR Surgical in the UK. Designed to be more compact and mobile than traditional systems, Versius aims to democratize access to robotic surgery by making it feasible for smaller hospitals and ambulatory surgery centers. Its modular design allows for flexible configuration around the patient, making it adaptable to various surgical environments.
Another promising development comes from the REVO-I system by Meere Company, a South Korean manufacturer. This platform mirrors many of the capabilities of established systems but at a reduced cost, addressing the growing need for affordability in robotic surgery. Meanwhile, in the academic sphere, the Smart Tissue Autonomous Robot (STAR) developed by researchers at Johns Hopkins University has garnered attention for its ability to perform soft-tissue surgery with minimal human intervention. In controlled trials, STAR has outperformed human surgeons in tasks like intestinal anastomosis, suggesting a future where AI-driven systems may play a central role.
The emergence of these surgical robots names signals a shift toward greater accessibility, affordability, and autonomy in robotic surgery. As research continues to validate their efficacy and safety, these systems may soon become integral components of mainstream surgical practice.
Ethical and Economic Implications of Robotic Surgery
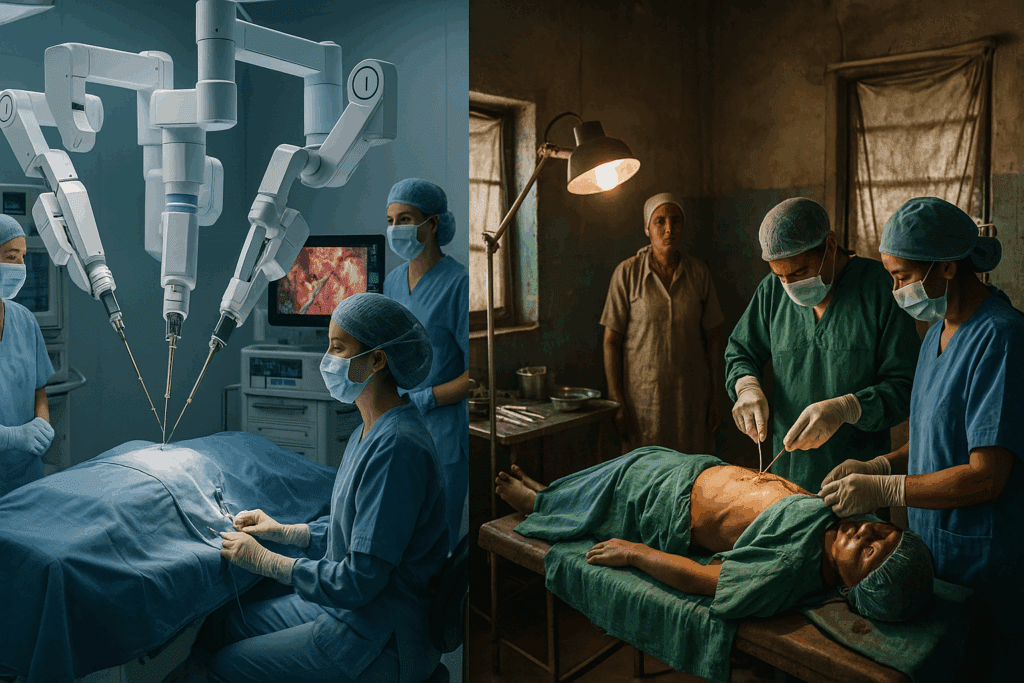
As with any groundbreaking medical technology, the widespread adoption of surgical robots brings with it a host of ethical and economic considerations. One major concern is cost. Robotic surgical systems are expensive, with initial investments ranging from $1 million to $2.5 million, not including maintenance, training, and disposable instruments. While these costs may be justified by improved outcomes and reduced hospital stays, they can also limit access, particularly in underfunded healthcare systems.
There is also the question of equity. If only large, well-funded hospitals can afford these technologies, patients in rural or underserved areas may be left behind. Efforts to develop more affordable robots used in surgery, like the REVO-I and Versius systems, are critical steps toward bridging this gap. Ethical considerations also extend to informed consent. Patients must be made fully aware of the benefits and limitations of robotic procedures, including the fact that, in some cases, robots may be operated by surgeons who are still early in their training with the technology.
Furthermore, as automation and AI become more integrated into surgical platforms, questions of accountability arise. Who is responsible if a semi-autonomous robot makes a critical error? Current regulatory frameworks are still catching up with these realities, making it essential for stakeholders to engage in proactive dialogue. The ultimate goal should be to ensure that advancements in robotic surgery are aligned with principles of justice, transparency, and patient-centered care.
Frequently Asked Questions: Exploring Robotic Surgery Innovations
1. What role do robots play in training future surgeons?
Robots used in surgery have become more than just tools in the operating room—they’re now essential platforms for surgical education and training. Advanced simulation environments that replicate real robotic systems allow residents to practice complex procedures without patient risk. These simulators incorporate surgical robots names like da Vinci or Versius, providing hands-on experience with interface navigation, instrument control, and camera handling. This kind of training is vital in ensuring that new surgeons not only understand the mechanics but also the decision-making processes involved in robotic-assisted procedures. Moreover, many institutions are developing curriculum-integrated modules where surgical residents progressively transition from simulators to supervised operations using actual surgery robot names recognized in clinical practice.
2. How do robotic systems address surgical fatigue and precision?
One of the lesser-discussed yet critical advantages of robotic surgery lies in its ability to reduce surgeon fatigue, which directly affects precision and outcomes. Traditional surgery often requires prolonged static postures, repetitive motions, and intense focus, leading to muscle strain and cognitive overload. Robotic systems alleviate this by allowing surgeons to operate from an ergonomic console, reducing physical burden. This improvement in operator comfort enhances concentration and enables finer motor control. With many types of surgical robots incorporating intuitive motion scaling and tremor filtration, even delicate micro-suturing can be executed with consistent accuracy, minimizing error from human fatigue.
3. Are robotic surgeries more cost-effective in the long run?
While the initial investment in robots used in surgery is significant, including infrastructure and ongoing maintenance, the long-term economics often favor robotic intervention. Reduced postoperative complications, shorter hospital stays, and quicker return-to-work timelines contribute to overall healthcare cost savings. Many types of surgical robots, despite their high price tags, improve operating room efficiency through shorter procedure times and fewer readmissions. As newer surgical robots names enter the market and competition drives down costs, the economic argument for robotics becomes increasingly compelling. Additionally, hospitals investing in advanced robotic platforms often see an uptick in patient referrals, further offsetting costs through increased volume.
4. How are robotics impacting global access to advanced surgical care?
Access to robotic surgery remains uneven across the globe, largely due to disparities in healthcare infrastructure and funding. However, emerging technologies are beginning to bridge this gap. Portable and modular systems, which represent new entries in the catalog of surgical robots names, are being designed specifically for low-resource environments. Moreover, cloud-based telepresence platforms allow expert surgeons to guide or supervise procedures remotely, bringing top-tier expertise to underserved regions. As types of surgical robots become more compact and cost-efficient, their deployment in rural and international health settings becomes more feasible, promoting equitable access to high-quality care.
5. What psychological benefits do patients experience from robotic procedures?
Patients undergoing robotic procedures often report reduced anxiety related to surgical outcomes, particularly when they understand that robots used in surgery offer greater precision and minimal invasiveness. The smaller incisions and faster recovery periods commonly associated with robotic interventions contribute to a perception of reduced trauma and lower risk. Knowing that leading surgery robot names are associated with some of the world’s top hospitals can also provide psychological reassurance. Additionally, being presented with robotic surgery examples during preoperative consultations can enhance patient trust and improve compliance with postoperative care instructions. The perception of cutting-edge technology often translates into greater confidence in the healthcare provider.
6. Can robotic systems improve outcomes in rare or complex cases?
Absolutely. In complex or rare surgical cases, robotic platforms offer advantages that go beyond conventional capabilities. High-definition 3D imaging, paired with multi-articulated instruments, allows surgeons to navigate anatomical variations with heightened awareness. Many types of surgical robots also incorporate real-time data integration, enabling intraoperative decision-making that is both precise and adaptive. These features are particularly beneficial in rare tumor resections or anatomical anomalies where traditional tools may fall short. As newer surgical robots names emerge with AI-enhanced capabilities, we can expect even greater customization of approaches for atypical and high-risk cases.
7. What advancements are shaping the next generation of robotic surgery?
Innovation in robotic surgery is accelerating rapidly, with several transformative technologies on the horizon. AI-driven analytics are beginning to assist in real-time surgical decision-making, providing predictive modeling based on accumulated procedural data. Emerging types of surgical robots now include haptic-enabled platforms that provide force feedback, allowing surgeons to “feel” virtual textures or resistance, enhancing situational awareness. Additionally, some surgery robot names are incorporating augmented reality overlays that project anatomical landmarks directly onto the surgeon’s view. These advancements not only refine surgical precision but also expand the scope of procedures that can be performed robotically.
8. How do regulatory bodies evaluate robotic surgical systems?
Before robotic systems are introduced to clinical practice, they must undergo rigorous assessment by regulatory authorities such as the FDA in the United States or the European Medicines Agency. These evaluations include scrutiny of device safety, efficacy, and compatibility with existing surgical protocols. Surgical robots names entering the market are typically subject to preclinical testing, simulation trials, and multi-phase human studies. Post-market surveillance also ensures continued compliance and identifies any long-term issues. As more robotic surgery examples demonstrate positive outcomes in peer-reviewed literature, regulatory bodies have become more open to accelerating approval timelines for platforms that show strong promise.
9. Are there risks of overreliance on robotic systems in surgery?
As robotic systems grow more sophisticated, there is a valid concern about potential overreliance. While robots used in surgery offer immense benefits, they are not infallible and require human oversight to ensure safety. Surgeons must remain well-trained in both robotic and traditional techniques to respond effectively to unexpected scenarios, including system malfunctions. There is also the psychological risk of surgeon deskilling if too much dependence is placed on automation. Integrating robotic surgery examples into comprehensive surgical education helps strike a balance, ensuring that human expertise complements technological precision.
10. What ethical concerns surround the use of robotic surgery in clinical trials?
Clinical trials involving robotic surgery introduce ethical complexities that differ from traditional surgical studies. Informed consent must include not only the nature of the procedure but also details about the specific robotic system being used. With many types of surgical robots still considered investigational, patients must understand the potential risks and limitations. Trials involving newly introduced surgery robot names should also ensure equitable access and avoid socioeconomic bias in participant selection. Additionally, outcomes must be transparently reported, including failures, to uphold scientific integrity and inform future innovation responsibly.
Conclusion: The Next Frontier of Robotic Medicine and Its Lasting Impact on Healthcare
The trajectory of robotic surgery is not merely a trend but a transformational movement that is redefining the way healthcare is delivered. From the well-established systems bearing familiar surgery robot names to the groundbreaking innovations emerging from academic research, the landscape is rich with promise and complexity. Each advance in robotic technology brings us closer to a future where surgical care is more precise, personalized, and accessible.
By examining diverse robotic surgery examples, we see how these machines have already improved outcomes in fields ranging from urology to neurosurgery. Understanding the types of surgical robots allows clinicians and institutions to make informed choices tailored to their needs, while awareness of the robots used in surgery globally helps foster collaboration and innovation across borders. The growing list of surgical robots names in development further expands the possibilities, ensuring that the momentum of progress continues.
Yet, amid the excitement, it is crucial to remain grounded in the principles of ethical implementation and equitable access. As we stand at the threshold of a new era in medical care, the lasting impact of robotic surgery will depend not only on technological innovation but also on our collective commitment to ensuring that these tools serve all patients, everywhere. The future of robotic medicine is undeniably bright—but it is our responsibility to ensure that its light reaches everyone it can heal.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Future Of Robotic Surgery: Things To Know About
Robot Assisted Surgery: Why it’s done and Risks
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.