Artificial intelligence (AI) is revolutionizing the modern world, and healthcare stands as one of its most transformative frontiers. As patients, professionals, and policymakers grapple with rapid technological evolution, understanding the pros and cons of AI in healthcare becomes not just beneficial but essential. This exploration delves into the intricate dimensions of AI-driven healthcare, offering a thorough analysis aimed at empowering every reader to appreciate the opportunities and challenges ahead.
Copy and paste text: Revolutionizing Healthcare: How AI in Medicine Is Enhancing Diagnosis, Treatment, and Patient Outcomes

The Evolution of AI in Healthcare
The journey of AI in healthcare is a story of ambition, innovation, and cautious optimism. Initially confined to theoretical models and basic decision-support tools, AI has now permeated nearly every aspect of healthcare delivery, from diagnostics to treatment planning. Machine learning algorithms sift through enormous datasets to find patterns invisible to the human eye, while natural language processing enables the extraction of critical insights from clinical notes. Today, AI assists radiologists in detecting tumors, predicts patient deterioration before visible symptoms appear, and even supports robotic surgeries that combine mechanical precision with human oversight. However, as exciting as these advancements are, they also signal the importance of examining both the transformative potential and inherent limitations of AI in healthcare settings.
Understanding the Pros and Cons of AI in Healthcare
Healthcare stakeholders must recognize the multifaceted nature of AI’s integration. While AI offers immense potential for improving outcomes, reducing costs, and personalizing patient care, it also introduces new ethical dilemmas, regulatory complexities, and technical challenges. A nuanced understanding of the pros and cons of AI in healthcare ensures a balanced approach to embracing its benefits without ignoring its pitfalls. Effective integration requires vigilance against algorithmic bias, overreliance on technology, and data security risks, among other concerns. This balanced perspective forms the cornerstone for sustainable and patient-centered AI adoption.
The Pros of AI in Healthcare: Transformative Opportunities
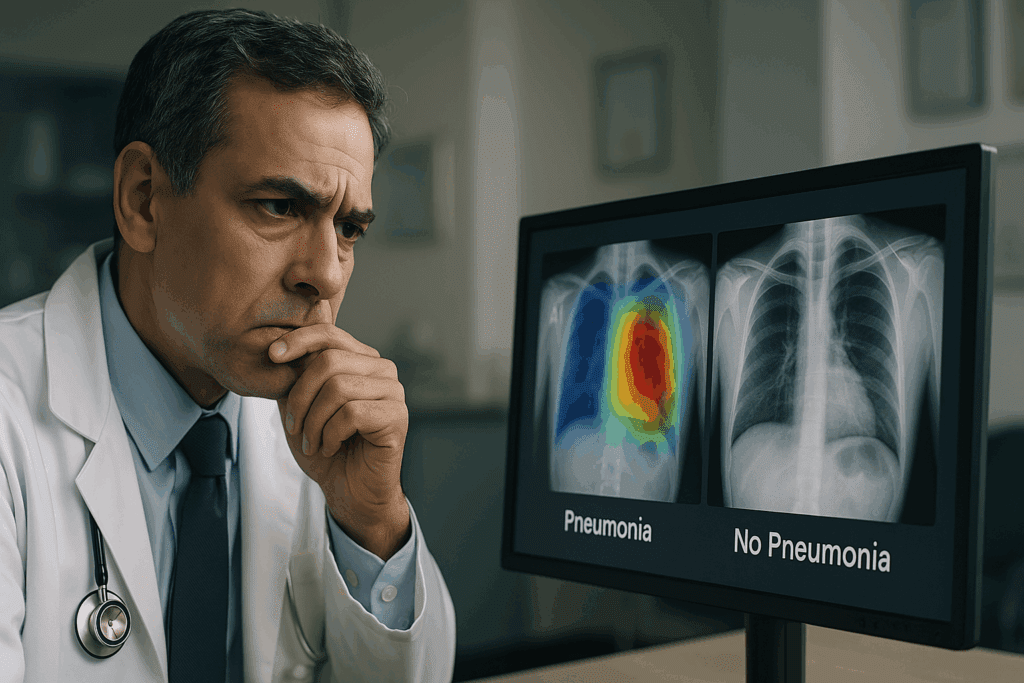
Perhaps the most celebrated benefit of AI in healthcare is its ability to enhance diagnostic accuracy. Tools like AI-powered imaging analysis can detect diseases such as cancer at earlier stages than traditional methods, potentially saving countless lives. Furthermore, AI facilitates personalized medicine by analyzing genetic, environmental, and lifestyle factors to recommend tailored treatments. Predictive analytics powered by AI identify high-risk patients, enabling preemptive interventions that can prevent hospitalizations and complications.
Operational efficiencies also rise dramatically with AI adoption. Automated administrative tasks, from patient scheduling to billing, free healthcare providers to focus more on patient care. Virtual health assistants offer 24/7 support, triaging minor ailments and providing medication reminders, thereby enhancing patient engagement and adherence to care plans. These improvements not only elevate the quality of healthcare delivery but also contribute to reduced healthcare costs, benefitting patients and providers alike.
Moreover, AI fosters medical research by accelerating data analysis and uncovering novel therapeutic targets. Researchers can now sift through massive datasets to identify trends and correlations in record time, propelling advancements in drug discovery and epidemiology. In critical care environments, real-time AI monitoring systems alert clinicians to early signs of sepsis or cardiac arrest, facilitating timely interventions that significantly improve patient outcomes.
Unveiling the Disadvantages of AI in Healthcare: A Necessary Caution
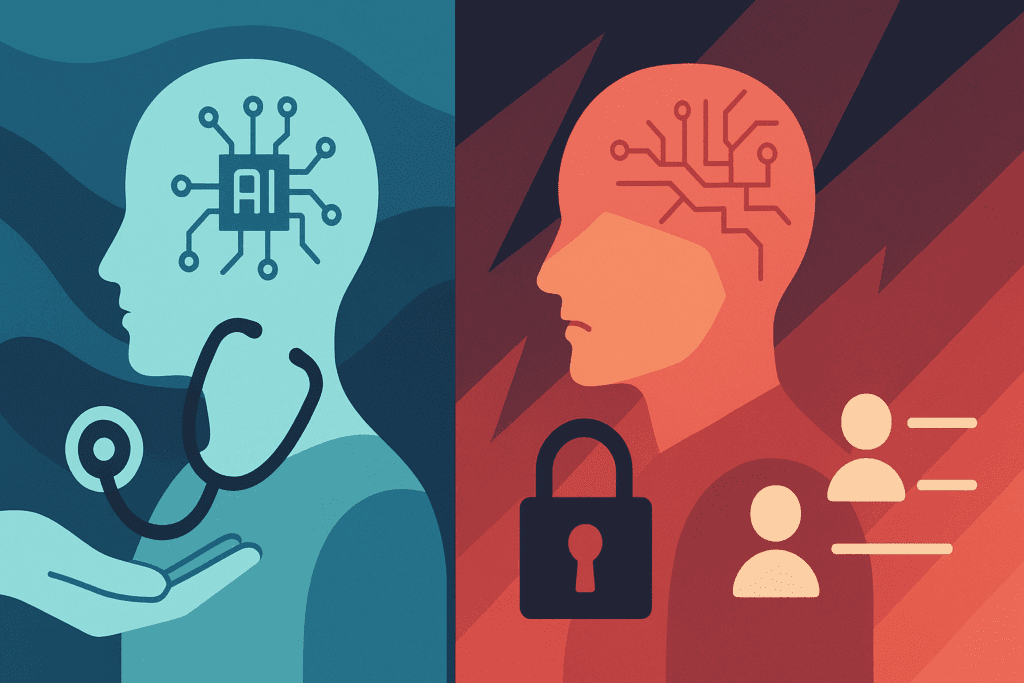
Despite its myriad benefits, it is crucial to acknowledge the disadvantages of AI in healthcare. One prominent concern is the risk of algorithmic bias, where AI systems inadvertently perpetuate existing disparities in healthcare access and outcomes. When algorithms are trained on incomplete or non-representative datasets, they may produce erroneous or inequitable recommendations that exacerbate health inequities.
Data privacy and security pose another major challenge. The massive volumes of sensitive health data required to train AI systems present attractive targets for cyberattacks. Breaches can lead to devastating consequences for patients, including identity theft, financial loss, and loss of trust in healthcare institutions. Regulatory frameworks often lag behind technological innovation, leaving gaps in legal protections and ethical guidelines.
Additionally, overreliance on AI can diminish critical thinking among healthcare providers. If clinicians begin to defer too heavily to AI-generated recommendations without exercising professional judgment, diagnostic errors and inappropriate treatments may result. Moreover, the “black box” nature of some AI systems—where even developers cannot fully explain how an algorithm arrived at a particular decision—complicates accountability and undermines trust.
The Pros and Cons of AI in Healthcare: Ethical Considerations and Moral Dilemmas
Ethical considerations permeate every discussion about the pros and cons of AI in healthcare. Issues such as informed consent, patient autonomy, and transparency become even more complex when AI is involved. Patients must understand how their data is used, and healthcare providers must ensure that AI-driven decisions are explainable and justifiable.
One pressing ethical concern is the tension between innovation and safety. While rapid AI deployment promises quicker solutions, it may also introduce unforeseen risks if not thoroughly validated. Rigorous clinical trials and peer-reviewed evaluations are necessary to safeguard patient welfare. Another ethical quandary revolves around data ownership. Patients may unknowingly surrender rights to their personal health information when consenting to data collection, raising questions about who ultimately benefits from AI innovations derived from their data.
Ensuring equitable access to AI-enhanced healthcare is equally vital. Without deliberate policies aimed at democratizing AI benefits, wealthier institutions and populations may disproportionately enjoy AI’s advantages, leaving underserved communities further behind. Bridging this digital divide is imperative to achieving a just and inclusive healthcare future.
How the Disadvantages of AI in Healthcare Impact Clinical Practice
Clinical practice is deeply affected by the disadvantages of AI in healthcare. For example, the integration of AI diagnostic tools can sometimes create conflicts between machine-generated outputs and clinician intuition. When discrepancies arise, determining the most accurate course of action can be challenging, especially if the clinician lacks a deep understanding of the AI system’s workings.
Moreover, the potential for “automation bias” looms large. Studies show that when human operators interact with highly automated systems, they may become complacent, placing undue trust in machine outputs even in the face of contrary evidence. In healthcare, such blind trust can have catastrophic consequences, underscoring the need for robust training programs that teach clinicians how to critically evaluate AI recommendations.
The financial burden associated with AI integration is another concern. Procuring, maintaining, and updating AI systems demand substantial investments that not all healthcare facilities can afford. Smaller practices and rural hospitals risk being left behind, widening the gap in care quality between different regions and socioeconomic groups. Strategic planning and equitable funding initiatives are required to ensure that AI serves as a bridge rather than a barrier to healthcare access.
The Pros and Cons of AI in Healthcare Research and Development
In the realm of medical research and development, the pros and cons of AI in healthcare manifest vividly. On the positive side, AI accelerates discovery timelines by automating data analysis, hypothesis generation, and even experimental design. AI-driven platforms have already identified promising drug candidates and novel disease biomarkers at unprecedented speeds, invigorating the pipeline for new therapies.
Yet, challenges abound. The reliance on historical data to train AI models can inadvertently bias research findings toward existing paradigms, stifling innovation rather than fostering it. Furthermore, AI-generated hypotheses may lack the nuanced contextual understanding that human researchers bring to the table, potentially leading to spurious conclusions if not rigorously vetted.
Intellectual property rights also become contentious. When AI algorithms contribute significantly to research outputs, determining authorship, patent ownership, and profit-sharing arrangements becomes complex. Clear regulatory frameworks and ethical guidelines must evolve alongside AI technology to prevent exploitation and promote fairness in research collaborations.
Patient Perspectives on the Pros and Cons of AI in Healthcare
Patients’ perceptions of AI in healthcare are shaped by personal experiences, media narratives, and broader societal attitudes toward technology. Many patients express optimism about AI’s potential to improve diagnostic accuracy, streamline care delivery, and offer more personalized treatment options. Access to telemedicine services, AI chatbots for preliminary consultations, and remote monitoring tools enhance convenience and empower patients to take a more active role in managing their health.
However, concerns about data privacy, loss of human touch, and the potential for dehumanization in care persist. For some, the idea of an AI system making life-altering decisions without direct human involvement feels unsettling, even alienating. Building trust requires transparent communication about AI’s capabilities, limitations, and the safeguards in place to protect patients’ rights and wellbeing.
Educational initiatives that demystify AI and highlight its collaborative role alongside healthcare providers can help bridge the trust gap. Encouraging patients to ask questions, seek second opinions, and engage critically with AI-driven recommendations reinforces autonomy and informed consent, ensuring that technological progress enhances rather than erodes patient-centered care.
Addressing the Disadvantages of AI in Healthcare Through Regulation and Policy
Effective regulation and policy development are pivotal in mitigating the disadvantages of AI in healthcare. Policymakers must craft robust legal frameworks that ensure data privacy, mandate transparency, and establish accountability for AI-driven decisions. Regulatory bodies such as the FDA have begun issuing guidelines for AI-based medical devices, but comprehensive, globally harmonized standards are still evolving.
Risk-based regulatory approaches—where the level of oversight corresponds to the potential harm posed by a given AI application—offer a pragmatic pathway forward. High-risk applications like diagnostic tools or autonomous surgical robots require stringent validation and monitoring, while lower-risk applications such as administrative task automation can undergo streamlined reviews.
Ethical oversight committees comprising diverse stakeholders, including patients, clinicians, ethicists, and technologists, can provide critical perspectives during AI system development and deployment. Encouraging cross-disciplinary collaboration ensures that AI solutions are not only technically sound but also ethically responsible and socially beneficial.
Future Outlook: Navigating the Pros and Cons of AI in Healthcare
As we look to the future, the pros and cons of AI in healthcare will continue to evolve. Emerging technologies such as explainable AI (XAI) aim to address transparency concerns by making AI decision-making processes more understandable to humans. Advances in federated learning—where AI models are trained across decentralized devices without transferring sensitive data—hold promise for enhancing data privacy while preserving AI’s analytical capabilities.
Moreover, interdisciplinary education programs that teach healthcare providers about AI’s strengths, limitations, and ethical dimensions will foster a workforce that is better equipped to leverage AI responsibly. Patient advocacy will play an increasingly prominent role, ensuring that technological innovation remains aligned with the needs and values of those it ultimately serves.
Global collaboration will be essential. Sharing best practices, harmonizing regulatory standards, and fostering inclusive innovation ecosystems can help mitigate disparities and promote equitable access to AI-enhanced healthcare worldwide. Balancing optimism with vigilance, innovation with ethics, and efficiency with empathy will be the guiding principles for a future where AI truly augments human healthcare.
Frequently Asked Questions: Exploring the Pros and Cons of AI in Healthcare
Q1. How is AI impacting rural healthcare access and outcomes?
AI is making significant strides in bridging the healthcare gap in rural and underserved communities. With limited access to specialists in these areas, AI-powered telemedicine platforms offer remote diagnostics and virtual consultations, reducing the need for patients to travel long distances. Furthermore, AI tools can help local practitioners by providing decision support systems that assist in identifying critical conditions such as strokes or sepsis early. While these advances contribute to better outcomes, challenges such as unreliable internet infrastructure and low digital literacy still hinder widespread implementation. Thus, to fully capitalize on AI’s benefits in rural settings, investments in technological infrastructure and targeted education initiatives are essential.
Q2. What are the psychological effects of integrating AI into patient care?
The psychological dimension of AI in healthcare is complex and often underexplored. Some patients may experience increased anxiety or discomfort knowing that algorithms, rather than solely human physicians, contribute to decision-making. Conversely, others may feel reassured by the precision and data-backed insights that AI provides. It’s also important to consider the emotional disconnect that might arise from reduced face-to-face interaction. Addressing these concerns requires careful system design that promotes transparency, empathy, and human oversight to maintain patient trust and emotional well-being.
Q3. Can AI help reduce clinician burnout?
One of the understated advantages in the ongoing debate around the pros and cons of AI in healthcare is its potential to reduce clinician burnout. By automating repetitive tasks such as documentation, scheduling, and administrative paperwork, AI allows healthcare professionals to dedicate more time to patient care and complex decision-making. Furthermore, AI-driven voice recognition software and ambient documentation tools are reducing the cognitive load during patient encounters. However, if not implemented thoughtfully, AI systems can introduce new stressors, such as interface complexity or workflow disruption. Therefore, usability and seamless integration into existing systems are key to ensuring AI supports rather than strains medical professionals.
Q4. How do AI systems handle rare diseases with limited data?
The performance of AI in recognizing rare diseases is inherently constrained by data scarcity, which poses a challenge to achieving diagnostic accuracy. Unlike common conditions that benefit from large training datasets, rare diseases may be underrepresented, leading to lower predictive accuracy. To address this, researchers are exploring synthetic data generation and transfer learning, where AI systems leverage related datasets to fill informational gaps. Collaboration between institutions to pool rare disease data can also enhance AI’s capabilities in this area. These approaches aim to mitigate one of the hidden disadvantages of AI in healthcare: the potential oversight of less common, yet critical, diagnoses.
Q5. What role does AI play in preventive medicine?
AI is emerging as a powerful ally in the shift from reactive to preventive healthcare. By analyzing large datasets from wearable devices, electronic health records, and even social determinants of health, AI can identify at-risk individuals before symptoms manifest. For example, predictive models can flag patients likely to develop chronic conditions such as diabetes or hypertension, prompting early interventions. This proactive approach reduces the long-term burden on healthcare systems and improves patient quality of life. However, the effectiveness of preventive AI hinges on ethical data collection, continuous model refinement, and patient compliance with recommendations.
Q6. Addressing Ethical Complexity: A Core Concern Within the Pros and Cons of AI in Healthcare
The ethical landscape is central to understanding the pros and cons of AI in healthcare. Key concerns include data ownership, algorithmic transparency, and consent for AI usage. Informed consent becomes particularly murky when patients are unaware of how AI influences clinical decisions or how their data is processed. Furthermore, opaque algorithms—often described as “black boxes”—challenge the principle of explainability, which is foundational in medical ethics. Institutions must establish transparent practices, offer explainable AI outputs, and empower patients with knowledge and choices to preserve autonomy and trust.
Q7. What training is required for clinicians to effectively use AI systems?
To ensure effective AI adoption, healthcare providers must undergo multidisciplinary training that extends beyond basic technical skills. Clinicians should learn how to interpret AI outputs, assess the reliability of predictions, and understand the underlying logic behind algorithmic decisions. Equally important is training in the ethical and legal implications of AI-assisted care. Simulation-based modules, continuous education programs, and interdisciplinary collaborations can cultivate the necessary skills. This comprehensive training not only improves safety but also addresses one of the subtle disadvantages of AI in healthcare: the risk of deskilling professionals who overly rely on technology.
Q8. Exploring Patient Trust in Light of the Pros and Cons of AI in Healthcare
Patient trust is both a facilitator and a barrier when it comes to the broader acceptance of AI in clinical environments. On the one hand, AI tools that deliver consistent, accurate diagnoses can reinforce confidence in the healthcare system. On the other, perceived impersonality or fears of data misuse can erode trust, especially among vulnerable populations. Strategies to foster trust include co-designing AI tools with patient input, offering transparent explanations, and maintaining human oversight in critical decisions. These actions bridge the gap between technological advancement and the relational nature of care.
Q9. How are startups and emerging technologies influencing the future of AI in healthcare?
Startups are pushing the envelope by introducing innovative AI applications, from mobile diagnostic tools to AI-powered mental health platforms. These agile companies often target specific niches that larger institutions may overlook, such as early screening tools for vision or speech disorders. By focusing on accessibility and user-friendly interfaces, startups contribute to democratizing AI benefits. However, the rapid pace of development can sometimes outstrip regulatory readiness, introducing risks related to safety and efficacy. Collaboration between innovators, regulators, and medical institutions is essential to harmonize progress with responsibility.
Q10. What global disparities exist in AI healthcare adoption?
Global adoption of AI in healthcare is uneven, with high-income countries benefiting from greater infrastructure, funding, and expertise. In contrast, many low- and middle-income nations face barriers including limited internet access, inadequate data ecosystems, and insufficient regulatory frameworks. These disparities risk exacerbating existing global health inequities. Initiatives that promote open-source AI tools, multilingual datasets, and capacity-building programs can help bridge the gap. Global partnerships and knowledge-sharing platforms are critical to ensuring that the advantages of AI do not remain confined to technologically advanced regions.
Reflecting on the Critical Pros and Cons of AI in Healthcare: A Call to Thoughtful Engagement
The critical pros and cons of AI in healthcare underscore the complexity of integrating transformative technologies into a field as deeply personal and consequential as medicine. AI offers unprecedented opportunities to enhance diagnostic accuracy, personalize treatment, and streamline healthcare delivery. Yet, it also introduces new ethical challenges, amplifies existing inequalities, and raises fundamental questions about trust, autonomy, and the nature of care.
To navigate this terrain successfully, stakeholders must engage thoughtfully, balancing enthusiasm for innovation with a steadfast commitment to ethical responsibility. Patients, providers, researchers, policymakers, and technologists must collaborate to ensure that AI development and deployment uphold the highest standards of quality, equity, and humanity.
Ultimately, the future of AI in healthcare depends not solely on technological advancements but on the collective choices we make about how to harness these tools in service of a healthier, more just, and more compassionate world.
Further Reading
Balancing The Pros And Cons Of AI In Healthcare


