Sleep is a fundamental component of human health, yet millions of individuals across the globe struggle with conditions that compromise the quality and continuity of their rest. For those experiencing chronic fatigue, frequent nighttime awakenings, or excessive daytime sleepiness, medical experts often recommend a diagnostic evaluation known as a sleep study. If you have ever wondered how does a sleep study work or what unfolds during such a clinical assessment, this guide will offer a comprehensive, medically accurate, and SEO-optimized look into every essential detail. Understanding the purpose, process, and outcomes of a sleep study can empower patients to make informed decisions and alleviate the anxiety that often accompanies medical testing.
You may also like: Essential Tips on How to Take Deep Sleep and Fight Everyday Fatigue
The Purpose and Value of Sleep Studies in Modern Medicine
Sleep studies serve as a cornerstone in the diagnosis of sleep disorders and related fatigue syndromes. They are designed to detect abnormalities in sleep architecture, respiratory patterns, neurological function, and other physiological behaviors during rest. A significant number of patients who undergo sleep studies report symptoms that suggest obstructive sleep apnea, narcolepsy, restless legs syndrome, or insomnia. The ultimate goal of a sleep study is to pinpoint the root cause of sleep disturbances and guide treatment strategies that enhance both sleep quality and overall health.
For clinicians, a sleep study offers a treasure trove of data collected over the course of one night (or occasionally multiple nights) in either a sleep laboratory or at home. These tests are indispensable tools in managing not only sleep apnea but also more elusive conditions that mimic common fatigue syndromes. Many patients who complain of being tired all the time are surprised to discover underlying problems such as periodic limb movement disorder or even rare parasomnias that would have remained undiagnosed without a formal evaluation. This reveals just how pivotal a sleep study can be in bridging the gap between symptoms and solutions.

How Does a Sleep Study Work in a Clinical Sleep Lab Setting?
When people ask how does a sleep study work, they are often envisioning a cold, impersonal room filled with machines. In reality, clinical sleep labs are typically designed to mimic a comfortable hotel room, complete with a bed, minimal noise, and climate control. The ambiance is intentionally crafted to promote natural sleep while enabling the precise monitoring of various biological signals.
Upon arrival, a registered polysomnographic technologist guides the patient through the setup process. A series of small, painless sensors are attached to the scalp, chest, legs, and face. These electrodes track vital signals such as brain waves (EEG), eye movements (EOG), muscle activity (EMG), and heart rhythm (ECG). Additional sensors monitor airflow, oxygen saturation, body movements, and snoring. The study typically begins at the patient’s usual bedtime, and data is recorded continuously throughout the night.
Despite the seemingly extensive setup, most patients adjust quickly and are able to fall asleep. The technologist remains in a separate control room, observing the patient through video monitoring and intervening only when necessary. The collected data is later analyzed by a board-certified sleep physician, who interprets the results in light of the patient’s symptoms, medical history, and test performance. This ensures that the findings are not only comprehensive but also clinically relevant.

The Home-Based Sleep Study: When and How It Works
Not all patients require the full spectrum of a laboratory sleep study. For those with a high likelihood of obstructive sleep apnea and no complicating medical conditions, a home sleep apnea test (HSAT) may be sufficient. This approach answers the same fundamental question—how does a sleep study work—but in a simplified and portable form.
A home sleep study typically involves a compact monitoring device with a nasal cannula, a chest strap, and a pulse oximeter that fits over the finger. Patients are given instructions on how to properly wear the equipment and are then able to sleep in their own bed, in their natural environment. While this method does not track brain waves or sleep stages, it excels at detecting sleep apnea and related breathing irregularities.
The convenience of HSATs cannot be overstated, especially for individuals who feel anxious in clinical environments or who have mobility limitations. However, because they offer a narrower scope of data, they are best suited for straightforward diagnostic scenarios. Complex cases involving parasomnias, suspected narcolepsy, or unexplained excessive daytime sleepiness still warrant a full in-lab evaluation.

What Can a Sleep Study Diagnose Beyond Sleep Apnea?
Though sleep apnea testing remains the most common reason for conducting a sleep study, the diagnostic potential of polysomnography extends far beyond this single condition. When evaluating what can a sleep study diagnose, one must consider a broad spectrum of sleep and neurological disorders that manifest through disturbed rest.
Restless legs syndrome (RLS), for instance, often presents with uncomfortable sensations and an uncontrollable urge to move the limbs, particularly in the evening. In many cases, RLS is associated with periodic limb movements during sleep (PLMS), which are objectively captured during a sleep study. These movements can significantly fragment sleep and contribute to daytime fatigue.
Another condition, narcolepsy, is characterized by sudden sleep attacks, vivid hallucinations, and cataplexy. Diagnosis typically involves both an overnight sleep study and a follow-up multiple sleep latency test (MSLT) conducted the next day. Parasomnias—which include sleepwalking, night terrors, and REM behavior disorder—also require in-lab testing to differentiate them from seizures or other nocturnal disturbances. In essence, a sleep study serves as a diagnostic gateway to understanding a multitude of sleep-related issues.
Interpreting the Results: What Happens After a Sleep Study Test?
Once the sleep study test is complete, the data is meticulously analyzed by a qualified sleep specialist. This post-evaluation process is as critical as the test itself. The recorded parameters are broken down into various metrics, such as sleep efficiency, apnea-hypopnea index (AHI), oxygen desaturation index (ODI), and arousal index. These metrics help quantify the severity and type of sleep disturbance.
For example, a high AHI indicates frequent interruptions in breathing, confirming a diagnosis of obstructive or central sleep apnea. Low oxygen saturation levels can reveal the extent to which sleep apnea affects blood oxygenation. Fragmented sleep architecture, characterized by a high arousal index or decreased time in restorative sleep stages (like REM or deep sleep), may suggest insomnia or another underlying issue.
The sleep specialist reviews these metrics in tandem with the patient’s symptoms and medical background. Based on this analysis, a tailored treatment plan is developed. This may involve the use of CPAP therapy for apnea, cognitive behavioral therapy for insomnia, or pharmacological interventions for conditions like narcolepsy. The goal is not just to treat the symptoms but to address the root causes of sleep disruption in a scientifically sound manner.
Sleep Apnea Testing: A Closer Look at the Diagnostic Process
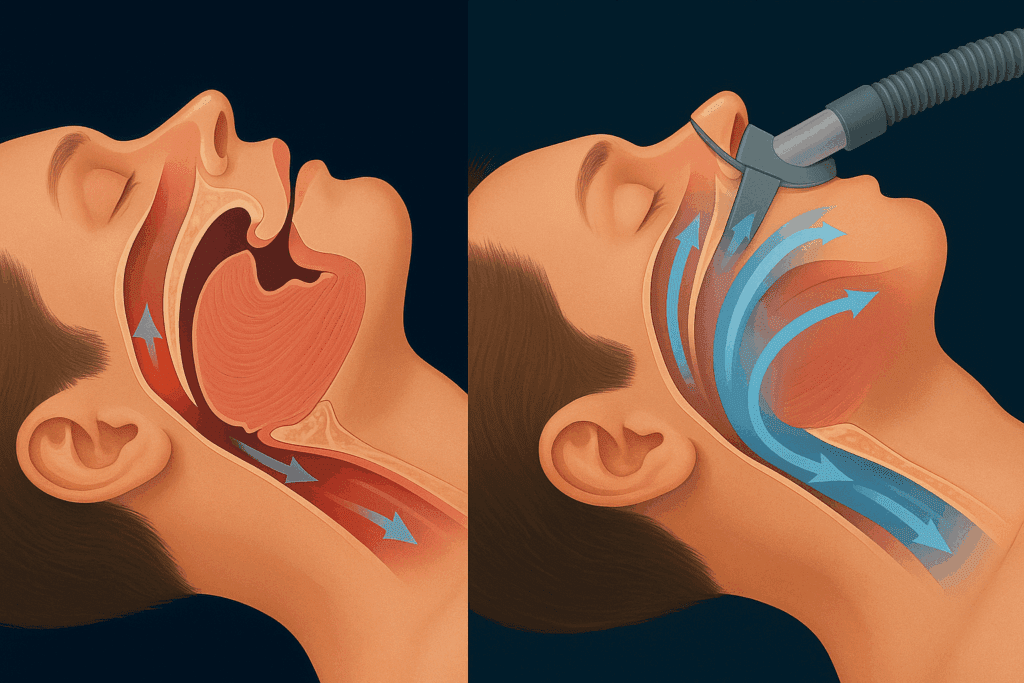
Among all the conditions diagnosed through sleep studies, sleep apnea remains the most prevalent and widely recognized. Sleep apnea testing involves monitoring for repeated episodes of breathing cessation (apneas) or shallow breathing (hypopneas) that lead to oxygen drops and micro-arousals from sleep. These disturbances often go unnoticed by the sleeper but have profound consequences on cardiovascular health and daytime function.
Sleep apnea testing, whether conducted at home or in a lab, focuses on identifying the frequency and severity of these episodes. Patients with an apnea-hypopnea index above five are generally considered to have sleep apnea, with classifications ranging from mild to severe. In addition to nighttime data, patients are also evaluated based on daytime symptoms such as fatigue, concentration problems, and mood disturbances.
It is worth noting that untreated sleep apnea is associated with an increased risk of hypertension, stroke, heart disease, and type 2 diabetes. Early diagnosis through accurate sleep apnea testing can therefore have life-saving implications. Treatment options include continuous positive airway pressure (CPAP), mandibular advancement devices, lifestyle modifications, and in some cases, surgical interventions. Understanding how these options relate to individual sleep study findings is key to effective long-term management.
Preparing for Your Sleep Study: What to Know and Expect
Patients often feel apprehensive about participating in a sleep test, but understanding the preparation process can ease much of this anxiety. Whether undergoing a home-based or lab-based sleep study, the objective is to capture a typical night of rest. Therefore, maintaining a normal sleep schedule in the days leading up to the study is essential.
Patients are typically advised to avoid caffeine, alcohol, and naps on the day of the test. Comfortable, loose-fitting sleepwear is encouraged, and personal items such as a favorite pillow can be brought along to help ease the transition. In the case of a lab-based study, medications should be discussed with the supervising clinician, as certain drugs can alter sleep architecture or mask symptoms.
Upon arrival, a technologist will guide you through the sensor attachment process, ensuring that each monitor is placed correctly and comfortably. While the experience may feel clinical at first, most patients adapt quickly and are able to sleep relatively normally. Understanding these steps in advance can greatly diminish stress and enhance the accuracy of the study results.
Addressing Common Concerns About the Sleep Test Experience
Despite reassurances, many patients harbor concerns about sleeping under observation or whether they will be able to sleep at all during the test. These worries are valid but usually unfounded. The staff is trained to create a comfortable, nonjudgmental environment, and patients are allowed ample time to fall asleep naturally.
A frequently asked question is whether the wires and sensors will interfere with sleep. While the setup may take some getting used to, the design prioritizes comfort and minimal intrusion. Most patients are surprised to find that they can sleep better than expected. The technologist is always nearby to make adjustments if necessary, and every effort is made to ensure a smooth, restful experience.
Another common concern relates to privacy. Modern sleep labs are equipped with discreet, non-invasive video monitoring systems, and data is handled with the utmost confidentiality. Understanding these protocols can help reassure patients that the test is both safe and respectful of personal boundaries.

How Does a Sleep Study Work for Diagnosing Pediatric Conditions?
Children, too, can suffer from sleep disorders, and pediatric sleep studies are designed with their unique needs in mind. Parents often ask how does a sleep study work for children and whether it differs significantly from adult testing. While the core principles remain the same, pediatric sleep studies involve additional considerations related to development, behavior, and comfort.
A parent is usually allowed to stay overnight with the child, and the testing environment is tailored to be more child-friendly. Smaller sensors and age-appropriate explanations help put young patients at ease. Pediatric sleep studies are particularly useful for diagnosing obstructive sleep apnea linked to enlarged tonsils or adenoids, as well as behavioral sleep disorders such as night terrors or sleepwalking.
Because children have different sleep patterns and needs, interpreting pediatric results requires a specialized skill set. Sleep specialists trained in pediatric medicine review the data within the context of the child’s age, developmental stage, and reported symptoms. Timely diagnosis and treatment can make a profound difference in a child’s cognitive, emotional, and physical development.
From Diagnosis to Treatment: Navigating the Next Steps After Your Sleep Study
Completing a sleep study is just the first step on the path to better rest and improved health. Once the results are in, the journey transitions from diagnosis to treatment. Depending on the findings, your sleep specialist may recommend further testing, lifestyle changes, or therapeutic interventions.
For patients diagnosed with sleep apnea, CPAP therapy remains the gold standard. This device delivers a constant stream of air to keep the airway open during sleep. Alternatives include dental appliances, weight loss programs, and positional therapy. Those diagnosed with insomnia may benefit from cognitive behavioral therapy or medication, while narcolepsy patients often require stimulants or wakefulness-promoting agents.
Regardless of the treatment approach, ongoing follow-up is essential. Sleep disorders are chronic in nature and may evolve over time. Continuous collaboration between patient and provider ensures that treatment remains effective, side effects are minimized, and quality of life is enhanced. This personalized, evidence-based approach lies at the heart of modern sleep medicine.
FAQ: Exploring the Complexities of Sleep Studies and Testing
How Does a Sleep Study Work When You Have Multiple Health Conditions?
When you’re managing more than one health condition—like diabetes, chronic pain, or cardiovascular disease—the way a sleep study works can be more nuanced. Clinicians will take a comprehensive medical history and may coordinate with other specialists to ensure the sleep test accounts for overlapping symptoms or medication side effects. For example, beta blockers can affect REM sleep patterns, and chronic pain may lead to frequent awakenings unrelated to a primary sleep disorder. The monitoring setup may also be modified to include additional sensors, such as continuous glucose monitoring or extra oxygen saturation probes, to capture a more holistic picture of the patient’s overnight physiological state. In these cases, how does a sleep study work extends beyond standard protocol, becoming an individualized diagnostic approach that helps untangle complex symptom presentations.
What Are the Psychological Effects of Undergoing a Sleep Study?
While the sleep study itself is non-invasive, it can trigger mild anxiety in some patients—especially those unaccustomed to medical environments or being observed overnight. Anticipation of the test may lead to pre-sleep jitters, a phenomenon known as “first-night effect,” where sleep patterns are less natural due to unfamiliar surroundings. Clinicians often mitigate this by providing detailed pre-test counseling and environmental accommodations, such as bringing your own pillow or using ambient white noise. In some cases, psychological responses post-study can be surprisingly positive, especially when patients gain a concrete diagnosis after years of ambiguity. The clarity provided by a sleep study test can have powerful emotional and mental health benefits, alleviating frustration and validating long-standing concerns.
How Does a Sleep Study Work in Remote or Rural Locations?
Accessing sleep study services in remote or underserved areas presents unique challenges, particularly where no sleep labs are available within a reasonable distance. In these cases, home-based sleep apnea testing becomes a vital alternative. Portable diagnostic kits are shipped to the patient, and telemedicine is used to walk them through the setup process. The data is then uploaded or returned via courier for specialist review. While not as comprehensive as a lab-based sleep study, these sleep tests offer a critical lifeline to diagnosis for patients who might otherwise go undiagnosed. Innovations in wearable technology and 5G connectivity are poised to further revolutionize remote sleep diagnostics, making access to care more equitable across geographies.
Can Lifestyle Changes Improve the Accuracy of Sleep Study Test Results?
Yes, adopting certain lifestyle habits before your scheduled test can significantly impact the reliability of the sleep study test. Sleep specialists often recommend stabilizing your sleep schedule at least a week in advance, avoiding stimulants like caffeine or alcohol, and limiting screen time in the evenings. These measures help your body establish a more predictable circadian rhythm, which in turn leads to data that more accurately reflects your natural sleep architecture. Some patients also keep a sleep diary or wear an actigraphy watch leading up to the test, providing useful context that augments the formal evaluation. Ultimately, well-prepared patients contribute to more precise diagnoses and treatment planning.
What Can a Sleep Study Diagnose That Might Surprise Most People?
Beyond the well-known diagnosis of sleep apnea, a sleep study can reveal subtler and sometimes unexpected conditions. For instance, bruxism—or teeth grinding during sleep—is often picked up via EMG (electromyography) readings, which track jaw muscle activity. A sleep test can also detect nocturnal seizures that may mimic parasomnias or simply go unnoticed by the sleeper and their partner. Furthermore, circadian rhythm disorders such as delayed sleep phase syndrome often become apparent through changes in sleep onset timing and phase shifts observed in the test data. This demonstrates that the answer to what can a sleep study diagnose extends far beyond basic respiratory assessments—it can uncover neurologic and behavioral patterns that influence sleep quality in profound ways.
Is There a Way to Monitor Sleep Without a Formal Sleep Study?
While nothing matches the clinical accuracy of a formal sleep study, there are validated consumer tools that offer useful, if limited, insights. High-quality wearable sleep trackers now include pulse oximetry, heart rate variability, and movement sensors to approximate sleep stages and detect anomalies. These tools are particularly beneficial for tracking trends over time and identifying patterns that may warrant formal evaluation. However, they cannot provide the depth of information needed for diagnosing complex conditions like REM sleep behavior disorder or central sleep apnea. Still, for patients hesitant to commit to a full sleep study, these technologies can serve as a stepping stone and open up conversations with healthcare providers about further testing.
How Does a Sleep Study Work Differently for Shift Workers?
Shift workers often suffer from disrupted circadian rhythms, making it more challenging to obtain accurate sleep data if testing occurs during conventional nighttime hours. In such cases, scheduling the sleep test during the individual’s typical sleep window—whether it’s daytime or early evening—is essential. The sleep lab adjusts its staffing and monitoring schedules to accommodate these atypical hours, ensuring that the data reflects the patient’s actual sleep-wake cycle. Polysomnographic scoring criteria may also be interpreted differently, with particular attention paid to markers of circadian misalignment. Understanding how does a sleep study work for shift workers involves an appreciation of biological clock variability and tailored clinical protocols.
What Happens if You Can’t Fall Asleep During the Sleep Study?
One of the most common concerns is the fear of being unable to sleep under observation, which could potentially affect the outcome of the sleep study test. While it’s true that patients may take longer to fall asleep in a new environment, labs allow extended monitoring time to ensure enough data is captured. Typically, just four hours of recorded sleep is considered sufficient for diagnostic purposes. If sleep latency is significantly prolonged, some centers may reschedule the test or recommend repeating it under mild sedation. The clinical team is trained to assess whether the limited data is adequate for a reliable diagnosis or if alternative approaches are needed. In any case, protocols are in place to prevent the test from becoming a wasted effort.
How Does a Sleep Study Work for Detecting Rare Sleep Disorders?
When it comes to diagnosing rare sleep disorders such as REM Sleep Behavior Disorder (RBD), fatal familial insomnia, or idiopathic hypersomnia, sleep studies require an elevated level of precision and customization. These tests often involve both overnight polysomnography and daytime multiple sleep latency testing (MSLT). In addition to standard biosignals, researchers may employ video monitoring with synchronized audio to capture behavioral anomalies during REM sleep. Sleep logs, genetic testing, and cerebrospinal fluid analysis may also be integrated into the diagnostic journey. Understanding how does a sleep study work in these advanced contexts reveals just how multi-dimensional and sophisticated sleep medicine has become.
Can a Sleep Study Help Improve Long-Term Cognitive Health?
Emerging research increasingly supports the link between quality sleep and long-term brain health. Conditions like sleep apnea, when left untreated, have been associated with increased risks of memory impairment, Alzheimer’s disease, and other forms of dementia. A sleep study can serve as a preventive health tool, identifying disturbances that compromise the brain’s overnight repair processes. Through interventions such as CPAP therapy or cognitive behavioral therapy for insomnia, patients may be able to preserve or even enhance cognitive function over time. Thus, beyond immediate symptom relief, a sleep study can play a pivotal role in safeguarding neurological well-being across the lifespan.
Conclusion: Embracing the Vital Role of Sleep Studies in Lifelong Wellness
Understanding how does a sleep study work unveils far more than the logistics of a single test. It opens a gateway to better health, restored energy, and improved quality of life. Sleep studies serve as a vital diagnostic tool that can detect a range of conditions, from sleep apnea and restless legs syndrome to parasomnias and narcolepsy. Each test offers a window into the complex, multifaceted world of sleep physiology and provides actionable insights that empower both patients and clinicians.
The decision to undergo a sleep study should be seen not as a final resort, but as a proactive investment in lifelong wellness. With precise diagnostic capabilities, individualized treatment pathways, and a foundation built on trust and scientific rigor, sleep studies represent the best of modern healthcare. By removing the mystery behind the process and embracing its potential, individuals can take meaningful steps toward reclaiming restful nights and vibrant, energetic days. Whether you’re grappling with chronic fatigue or unexplained sleep disturbances, the clarity offered by a comprehensive sleep study may be the first step on your journey to better health.


