Gastroesophageal reflux disease, more commonly known as GERD, is a chronic digestive disorder that affects millions of adults worldwide. While it often starts subtly, with occasional heartburn or regurgitation, it can evolve into a persistent condition that disrupts daily life. A common and pressing question among those experiencing symptoms is, “how long does GERD last in adults?” The answer varies significantly depending on the underlying cause, severity, lifestyle factors, and treatment adherence. Understanding the nature of GERD, how it develops, and what influences its duration can help adults manage it more effectively and prevent potential complications.
You may also like: How to Meal Prep for the Week: A Dietitian-Approved Guide to Stress-Free Planning, Balanced Nutrition, and Long-Term Wellness
Understanding GERD: A Persistent Digestive Concern
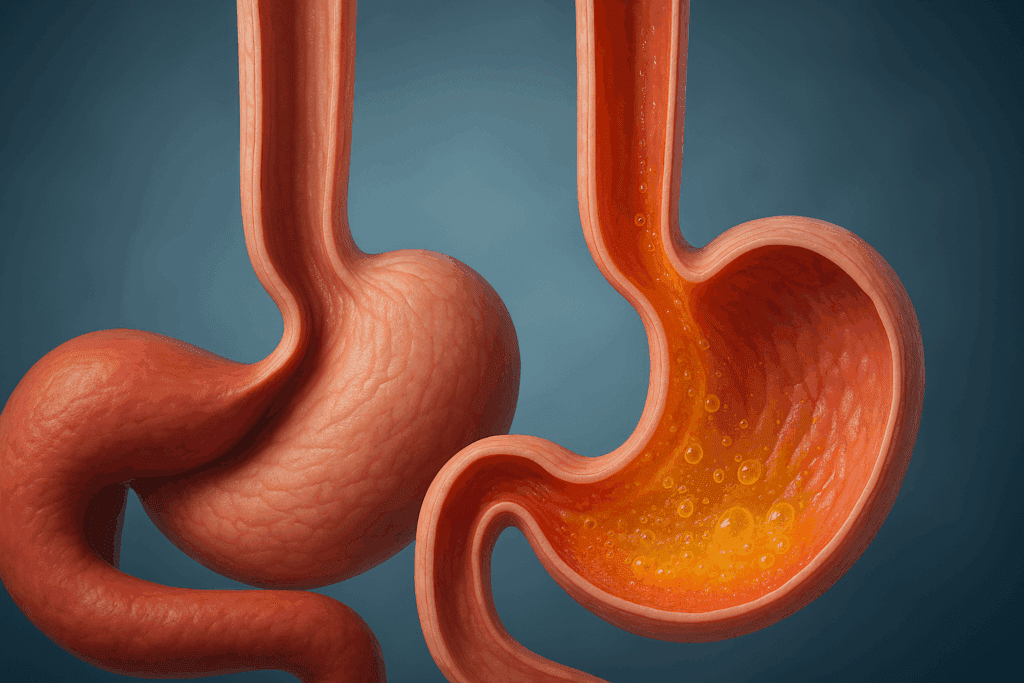
GERD occurs when the lower esophageal sphincter (LES) becomes weakened or relaxes inappropriately, allowing stomach acid to flow back into the esophagus. This backward movement of acid, known as reflux, leads to symptoms like heartburn, chest discomfort, regurgitation, and in some cases, chronic cough or hoarseness. Unlike occasional acid reflux, which is relatively common and transient, GERD is a long-term condition that may require ongoing medical attention. The difference between GERD and acid reflux lies in their frequency and impact; GERD involves more persistent and severe symptoms that can lead to complications if left untreated.
The answer to how long GERD lasts in adults hinges on several variables. For some individuals, GERD is a temporary response to dietary indiscretions or short-term stress. For others, it becomes a lifelong condition requiring consistent lifestyle modifications and medical management. Understanding how GERD happens is critical: factors like obesity, hiatal hernia, smoking, pregnancy, and certain medications can all contribute to its development. Recognizing these risk factors early can influence both the severity and duration of the disease.

Key Triggers and Lifestyle Factors That Influence GERD Duration
Lifestyle and dietary choices play a significant role in the progression and persistence of GERD. Foods high in fat, spicy meals, chocolate, caffeine, and alcohol are known to relax the LES and exacerbate reflux symptoms. Similarly, lying down shortly after eating or wearing tight clothing can increase abdominal pressure and encourage reflux. While some individuals may experience symptoms intermittently, others develop chronic reflux due to ongoing exposure to these triggers.
Stress also influences digestive health, potentially worsening GERD by increasing acid production or triggering behavioral changes like overeating or smoking. Understanding the psychological component is essential when evaluating how long GERD may last in adults. Those who address emotional well-being alongside physical health often report better symptom control. Physical activity, while generally beneficial, can also aggravate GERD if not timed correctly. Exercising immediately after eating or engaging in high-impact sports may worsen reflux.
The presence of underlying health conditions like diabetes, asthma, or connective tissue disorders can prolong the duration of GERD. These conditions may alter esophageal motility or acid clearance, making it more difficult to control symptoms. Therefore, a comprehensive medical evaluation is vital for tailoring treatment to the individual and managing any coexisting disorders.
How Long Does GERD Last in Adults When Left Untreated?
One of the most significant factors determining the duration of GERD is whether the condition is addressed promptly. If GERD is left untreated, it often persists indefinitely, with symptoms waxing and waning over time. Chronic exposure to stomach acid can damage the esophageal lining, leading to complications such as esophagitis, strictures, Barrett’s esophagus, and even esophageal cancer.
These complications of gastroesophageal reflux disease not only impact quality of life but also make treatment more complex. Esophagitis, an inflammation of the esophageal lining, can cause pain and difficulty swallowing. If untreated, repeated cycles of injury and healing may lead to scar tissue, resulting in esophageal strictures that narrow the passageway. Barrett’s esophagus, a condition in which the normal esophageal lining is replaced with abnormal cells, is considered precancerous and requires regular monitoring.
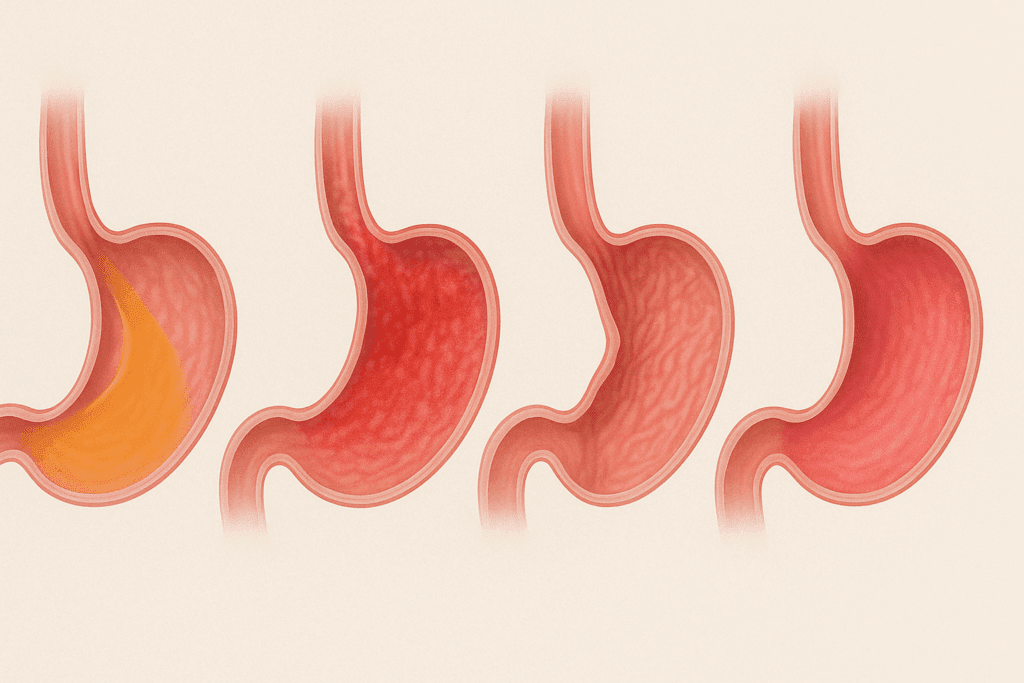
Therefore, understanding the stages of acid reflux disease is critical. GERD may begin with occasional reflux (Stage 1), evolve into persistent symptoms (Stage 2), and lead to complications (Stage 3) if ignored. The longer GERD persists without intervention, the more likely it is to cause permanent esophageal damage. While the initial stages may be reversible with lifestyle changes and medication, later stages often require more intensive treatment and may have lasting consequences.
Diagnosis and Testing: How Is Reflux Diagnosed in Adults?
Accurate diagnosis is essential for managing GERD effectively. Many patients initially self-diagnose based on symptoms like heartburn or the sensation of food coming back up the throat. However, a formal diagnosis by a healthcare provider ensures that other conditions are ruled out, and appropriate treatment is initiated.
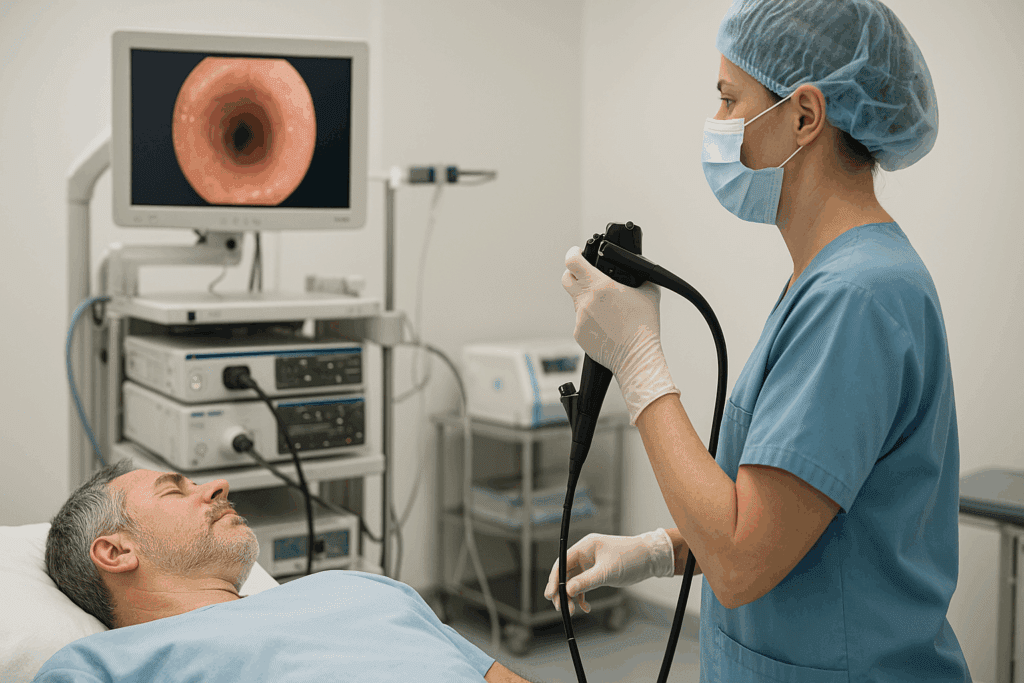
The primary method for diagnosing GERD is through clinical evaluation and symptom history. However, additional tests may be necessary to confirm the diagnosis or assess the extent of esophageal damage. A gastroesophageal reflux disease test may include upper endoscopy, ambulatory pH monitoring, esophageal manometry, and barium swallow studies.
Upper endoscopy involves using a flexible tube with a camera to visually inspect the esophagus and stomach. This test can detect inflammation, ulcers, strictures, and signs of Barrett’s esophagus. In cases of GERD without esophagitis, the esophagus may appear normal despite the presence of significant symptoms, highlighting the need for other diagnostic tools. Ambulatory pH monitoring measures acid exposure in the esophagus over 24 to 48 hours and is especially useful for identifying reflux in patients who do not respond to standard treatment.
Esophageal manometry evaluates the function of the esophagus and LES, particularly in patients with swallowing difficulties or those considering surgery. Barium swallow studies involve swallowing a contrast solution and taking X-rays to visualize structural abnormalities or delayed esophageal clearance. These diagnostic tools not only confirm GERD but also help distinguish it from conditions with overlapping symptoms, such as eosinophilic esophagitis or functional heartburn.
GERD Without Esophagitis: A Hidden Variant
An important variant of GERD that is often underdiagnosed is gastroesophageal reflux disease without esophagitis. In these cases, patients experience the classic symptoms of GERD but have a normal endoscopic exam. This form of GERD can be particularly frustrating for patients who feel dismissed due to the lack of visible inflammation.
The absence of esophagitis does not mean that the condition is less serious. In fact, untreated GERD without esophagitis can still lead to complications over time, including hypersensitivity of the esophagus and chronic cough. This form is also challenging to diagnose without pH monitoring, underscoring the importance of advanced diagnostic methods.
For these patients, symptom control becomes the main focus, with proton pump inhibitors (PPIs), H2 blockers, and lifestyle modifications forming the core of treatment. Long-term follow-up is often needed to ensure that symptoms are adequately managed and to monitor for any progression to visible esophageal damage.
Types and Stages of Reflux: Understanding the Progression
There are various types of reflux that contribute to the spectrum of GERD. Acid reflux is the most common and involves the backflow of acidic stomach contents. However, other forms include non-acid reflux, bile reflux, and silent reflux. Each type presents differently and may require specialized diagnostic and therapeutic strategies.
Silent reflux, also known as laryngopharyngeal reflux (LPR), occurs when stomach contents reach the throat or voice box. Symptoms may include hoarseness, chronic throat clearing, and a sensation of a lump in the throat. Unlike typical GERD, silent reflux rarely causes heartburn, making it more difficult to diagnose.
Understanding the reflux stages helps clarify the progression of GERD. Early-stage GERD may be episodic and triggered by specific foods or stress. Intermediate stages involve more frequent and severe symptoms, often requiring medication. Advanced stages are marked by complications like Barrett’s esophagus or strictures. The ability to recognize these stages allows for timely intervention and may influence how long GERD lasts in adults.
Heartburn vs. Acid Reflux: Clarifying Common Confusion
A frequent point of confusion among patients is the difference between acid reflux and heartburn. Acid reflux refers to the actual physiological event of acid moving from the stomach to the esophagus. Heartburn, on the other hand, is a symptom that results from this reflux. It presents as a burning sensation in the chest, often mistaken for a cardiac issue.
Similarly, the terms GERD and acid reflux are sometimes used interchangeably, which can be misleading. While all GERD involves acid reflux, not all acid reflux qualifies as GERD. The distinction lies in the frequency and severity of symptoms. Understanding this difference helps patients seek medical attention appropriately and avoid delays in diagnosis.
Patients often ask, “is acid indigestion the same as acid reflux?” Though related, acid indigestion is a broader term that may encompass a variety of upper abdominal discomforts, including bloating and nausea, while acid reflux specifically refers to the backflow of stomach acid. Clarifying these terms empowers patients to communicate their symptoms more effectively with healthcare providers.

Is GERD Permanent? Exploring Prognosis and Treatment Outlook
One of the most pressing concerns for individuals with GERD is whether the condition is permanent. The answer is nuanced. For some adults, GERD can be resolved through aggressive lifestyle changes, weight loss, and temporary medication. For others, especially those with anatomical abnormalities or long-standing disease, GERD may become a chronic issue that requires lifelong management.
Whether GERD is permanent often depends on the underlying cause and how early treatment is initiated. Patients who address their triggers and adhere to medical advice often experience significant relief. However, lapses in lifestyle changes or discontinuation of medication can lead to symptom recurrence.
Surgical options, such as Nissen fundoplication or magnetic sphincter augmentation, are available for individuals with severe or refractory GERD. These procedures aim to strengthen the LES and reduce reflux episodes. While surgery can offer long-term relief, it is generally reserved for patients who do not respond to medical therapy or who wish to avoid long-term medication use.
How Long Does GERD Last in Adults with Proper Treatment?
The duration of GERD symptoms can vary considerably based on treatment adherence and individual physiology. With proper treatment, many patients experience symptom relief within a few weeks. However, achieving full resolution and preventing recurrence often requires long-term commitment.
Pharmacologic therapy typically begins with proton pump inhibitors, which reduce acid production and allow the esophagus to heal. These medications are generally taken for 4 to 8 weeks, with some patients requiring ongoing therapy. H2 blockers and antacids may be used for milder symptoms or as adjunctive therapy.
Lifestyle changes remain a cornerstone of effective GERD management. Elevating the head of the bed, avoiding late-night meals, and maintaining a healthy weight can significantly reduce symptom frequency. Stress management techniques, such as mindfulness and cognitive behavioral therapy, may also play a role in symptom control.
For individuals who follow medical advice consistently, GERD can often be brought under control within a few months. However, the condition may return if lifestyle habits regress or new triggers emerge. This cyclical nature underscores the importance of long-term monitoring and patient education.
Prevalence and Public Health Impact: How Many People Have GERD?
GERD is one of the most common digestive disorders worldwide, affecting approximately 20% of the adult population in Western countries. In the United States alone, millions of adults experience weekly symptoms, with many more suffering silently without seeking medical help.
The high prevalence of GERD has significant public health implications. It contributes to reduced work productivity, increased healthcare utilization, and diminished quality of life. The cost burden includes not only direct medical expenses but also the economic impact of missed workdays and impaired daily functioning.
Understanding how many people have GERD also highlights the importance of awareness campaigns and early intervention. Public education on dietary habits, weight management, and symptom recognition can help reduce the overall burden of disease. Clinicians must also be vigilant in screening for GERD during routine check-ups, especially in patients with risk factors.
How to Diagnose GERD Without Endoscopy: Emerging Tools and Techniques
Endoscopy remains a valuable tool for diagnosing GERD, but not all patients require it. For those with typical symptoms and no alarm features, a trial of acid suppression therapy is often used as both a diagnostic and therapeutic strategy. If symptoms improve, a diagnosis of GERD is likely.
Emerging technologies offer additional ways to diagnose GERD without endoscopy. Impedance-pH monitoring, for instance, detects both acid and non-acid reflux, providing a more comprehensive view of reflux patterns. Wireless pH capsules can be temporarily attached to the esophagus during endoscopy and transmit data for several days, enhancing diagnostic accuracy.
Symptom questionnaires and scoring systems, such as the GERD Questionnaire (GerdQ), also provide valuable insight. These tools assess the frequency and severity of symptoms and can guide treatment decisions. While not a substitute for objective testing, they are useful in primary care settings and for monitoring treatment response.
Frequently Asked Questions About GERD in Adults
How Long Does GERD Last in Adults When Managed with Alternative Therapies?
While conventional treatments like proton pump inhibitors remain the cornerstone of GERD management, some adults find lasting relief through alternative approaches. Acupuncture, herbal medicine, and dietary therapy have been explored in various studies for their impact on reflux symptoms. Though research is ongoing, patients who combine these approaches with standard care may experience fewer recurrences. The key lies in consistency and medical supervision, as natural remedies still require careful monitoring. Understanding how long GERD lasts in adults under alternative therapy depends greatly on individual physiology, symptom severity, and the integration of lifestyle practices.
Can GERD Without Esophagitis Still Be Dangerous?
Gastroesophageal reflux disease without esophagitis may appear less concerning due to the absence of visible inflammation, but it can still lead to functional issues and long-term hypersensitivity. Patients often report chronic throat irritation, unexplained coughing, or regurgitation reflux without any abnormalities showing up on endoscopy. The invisibility of damage can delay diagnosis and treatment, compounding discomfort and contributing to mental distress. Over time, untreated GERD without esophagitis may impair esophageal motility and disrupt normal swallowing. It’s crucial to understand that visible damage isn’t always necessary for complications of gastroesophageal reflux disease to develop.
What Is the Difference Between Acid Reflux and Heartburn in Real-World Scenarios?
While many people use the terms interchangeably, the difference between acid reflux and heartburn becomes evident when you consider context. Acid reflux is a physical event, often silent, where stomach contents move upward into the esophagus. Heartburn, however, is the burning sensation that may or may not accompany reflux, depending on pain thresholds and the presence of inflammation. Some patients may experience acid reflux during sleep without any awareness until symptoms like hoarseness or sore throat appear in the morning. Recognizing this difference is essential for accurate diagnosis and effective symptom tracking, especially when managing complex reflux stages.
Why Do People Get GERD Despite a Healthy Lifestyle?
Many individuals wonder why they develop GERD despite having balanced diets and regular exercise routines. Genetics plays a substantial role; certain people inherit a naturally weak lower esophageal sphincter. Others may have undiagnosed anatomical variations such as a small hiatal hernia, which predispose them to reflux. Hormonal changes, including those during pregnancy or menopause, can also alter esophageal function. Even with optimal habits, underlying physiological differences may trigger symptoms, which is why the question “why do people get GERD” doesn’t always have a lifestyle-based answer.
How Does GERD Occur During the Night and What Can Be Done About It?
Nighttime GERD is a particularly disruptive manifestation of the disease. It occurs more frequently when individuals lie flat, allowing gravity to assist the upward movement of acid. This type of reflux is associated with a greater risk of aspiration and respiratory complications. Specialized wedges or adjustable beds can be highly effective in reducing nocturnal symptoms. Understanding how GERD occurs in different postures empowers patients to modify sleeping environments and improve overall outcomes.
What Are the Most Overlooked Signs of GERD Complications?
Beyond the classic heartburn and regurgitation, GERD complications can present in subtle ways. Chronic sinus infections, voice fatigue, and even dental erosion may stem from consistent acid exposure. These manifestations are often misattributed to other conditions, delaying appropriate gastroesophageal reflux disease diagnosis. Recurrent pneumonia or unexplained asthma flare-ups may indicate acid entering the airway. Paying attention to these atypical symptoms can catch gerd complications before they advance into more severe reflux stages.
How to Diagnose GERD Without Endoscopy in Resource-Limited Settings?
In areas where endoscopy isn’t readily available, healthcare providers often rely on detailed symptom questionnaires and therapeutic trials. The GerdQ and similar tools assess symptom frequency and severity, offering a reliable pathway to presumptive diagnosis. A trial of proton pump inhibitors may also serve dual purposes: if symptoms improve, GERD is likely. Community clinics sometimes utilize barium swallow tests as an alternative gastroesophageal reflux disease test. Knowing how to diagnose GERD without endoscopy is essential in rural healthcare, telemedicine contexts, or during pandemics when access to advanced diagnostics is limited.
Understanding Reflux Stages: How Long Does GERD Last in Adults at Each Stage?
The timeline of GERD can vary significantly depending on the stage of the condition. In early stages, symptoms may last only a few weeks and respond rapidly to treatment. Middle stages, where damage begins to accumulate, might stretch over months and require a combination of medications and dietary changes. Advanced stages of acid reflux disease, particularly those involving Barrett’s esophagus or strictures, can persist for years or become chronic. How long GERD lasts in adults depends on both physiological resilience and how promptly each stage is identified and managed. Lifestyle discipline and routine follow-ups are key to avoiding progression.
What Social or Psychological Impacts Are Linked to Chronic GERD?
Living with chronic GERD can take a toll beyond physical discomfort. Constant vigilance over food choices and the unpredictability of flare-ups can lead to anxiety and social withdrawal. Many adults report avoiding social gatherings or travel due to fear of triggering symptoms. These lifestyle constraints may contribute to depression and lowered self-esteem, especially in younger adults balancing work and social life. A comprehensive GERD diagnosis should include psychosocial evaluations, highlighting the importance of a holistic treatment approach.
How Is GERD Different Across the Spectrum of Acid-Related Conditions?
Understanding GERD vs acid reflux involves appreciating its broader scope and potential consequences. While occasional acid reflux might require little more than antacids, GERD often necessitates long-term management. The types of GERD can range from erosive esophagitis to non-erosive reflux disease (NERD), each with unique clinical implications. Meanwhile, terms like heartburn vs acid reflux or is acid indigestion the same as acid reflux continue to create confusion, yet they reference distinct experiences or mechanisms. Clarifying these differences helps avoid under-treatment and ensures that all types of reflux are addressed appropriately within the healthcare system.
Final Thoughts: Why Do People Get GERD and What Can Be Done?
Ultimately, the question of “why do people get GERD” has multiple answers. Genetic predisposition, dietary habits, lifestyle choices, and coexisting health conditions all play a role. Modern sedentary lifestyles and the prevalence of processed foods have likely contributed to the rising incidence of GERD in recent decades.
Preventing GERD involves addressing modifiable risk factors. Encouraging physical activity, avoiding trigger foods, maintaining a healthy weight, and reducing stress are foundational steps. For those already diagnosed, adherence to treatment and regular follow-up are essential for preventing complications.
GERD may not always be curable, but it is manageable. With the right approach, adults can reduce the severity and frequency of symptoms, improve their quality of life, and avoid long-term damage. Whether temporary or chronic, understanding the full scope of GERD empowers patients to take control of their digestive health.


