Description
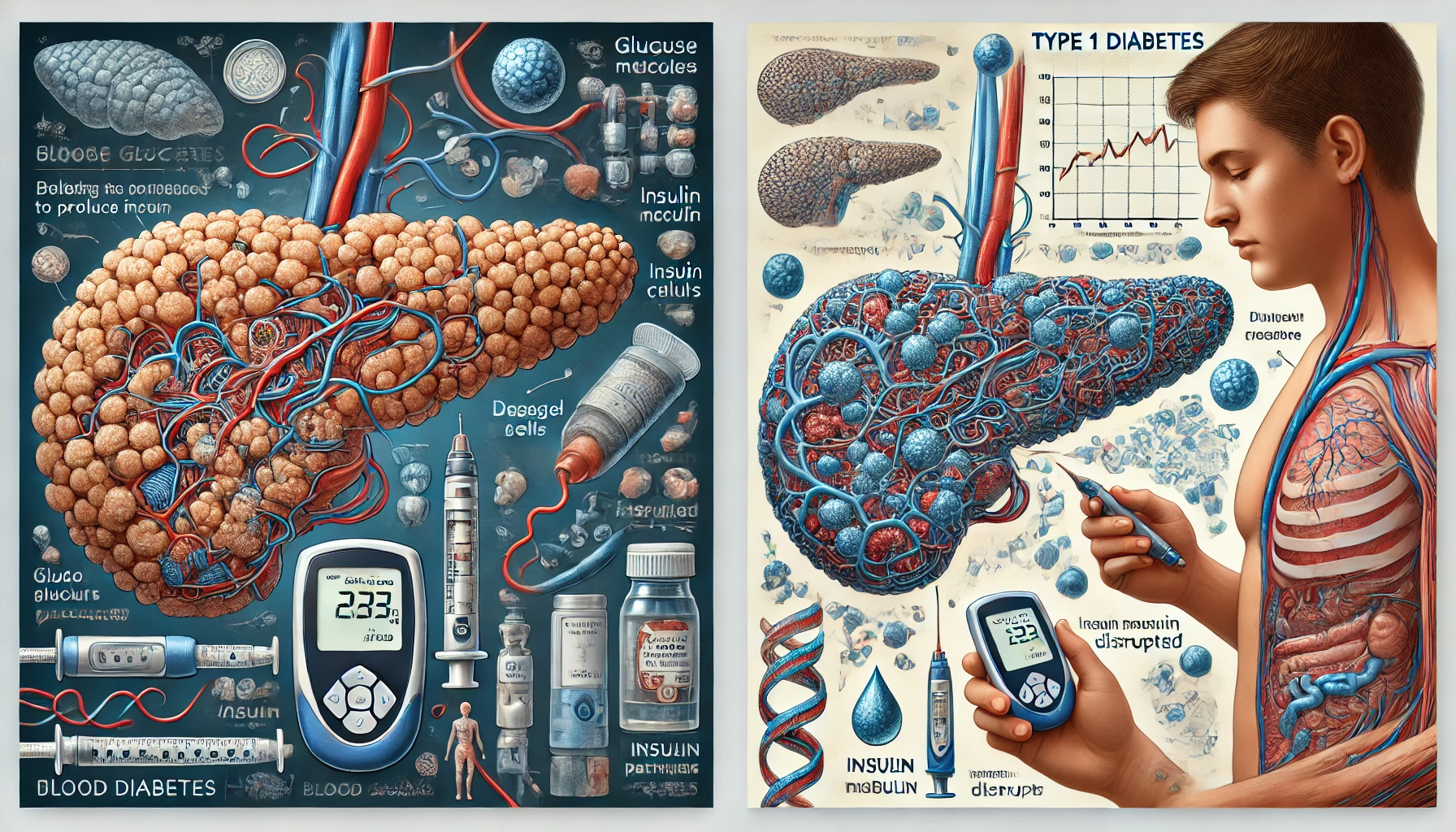
A complex metabolic condition called diabetes mellitus causes high blood glucose levels as a result of impaired insulin synthesis and/or action. Type 1 diabetes represents an autoimmune disorder in which the body’s immune system unintentionally targets and kills insulin-secreting beta cells inside the pancreas. Type 1 diabetes, sometimes called juvenile diabetes, diabetes involving insulin reliance, or any age, typically manifests during childhood or adolescence.
It causes between 5 and 10% of all instances of diabetes. An utter lack of insulin, a hormone necessary for controlling blood glucose levels, is the main warning sign for type 1 diabetes. Hyperglycemia, or high blood sugar, and a number of related problems result from a lack of insulin because glucose cannot reach cells for energy.
The following are some essential traits underlying type 1 diabetes: –
Dependency on Exogenous Insulin: The only way for people with Type 1 diabetes to control their blood glucose levels is through external sources of insulin, commonly delivered through insulin pumps or injections.
Beta Cell Autoimmunity-mediated Destruction: Beta cells located in the pancreas are mistakenly thought to be foreign invaders by the body’s immune system, which then starts an immunological response to kill them in type 1 diabetes. Insulin production is severely reduced or completely stopped as a result of this autoimmune attack.
Symptoms: Polydipsia (excessive thirst), polyuria (frequent urination), unexplained weight loss, weariness, and blurred vision are typical signs of Type 1 diabetes. If untreated, it may result in diabetic ketoacidosis, a disease that could be fatal.
You May Also Like:
CREST syndrome | Limited cutaneous systemic sclerosis: Description, Causes, and Treatment Protocol
Diabetes, type 1: Description, Causes, and Treatment Protocol is an original (MedNewsPedia) article.
Possible Causes
Type 1 diabetes is thought to be brought on by a confluence of immunological, genetic, and environmental factors. However, its precise etiology is yet unknown. Several possible causes and risk aspects include: –
Autoimmune Response: The immune system incorrectly targets and kills beta cells in Type 1 diabetes, which has an autoimmune component. For those with a genetic predisposition, environmental triggers like viral infections (such as enteroviruses) can trigger an autoimmune reaction.
Genetic Predisposition: People with family histories of type-1 diabetes are more likely to have the disease. Specific genetic traits, like particular HLA genotypes, are linked to an elevated risk.
Environmental Factors: Type 1 diabetes has been linked to exposure to specific environmental factors, including early childhood illnesses, nutritional problems, and low vitamin D levels.

Exacerbating and Mitigating Factors
Diabetes type 1 requires careful management to regulate blood sugar levels since it is marked by the autoimmune death of beta cells that produce insulin. While aggravating factors might increase blood glucose levels, mitigating factors may help to maintain stability.
The exacerbating factors include: –
Dietary Choices: Blood sugar surges can be caused by excessive consumption of refined carbs and sugary foods. Thus, maintaining a healthy diet is essential.
Inadequate Insulin Management: Skipping or taking insufficient amounts of insulin can cause hyperglycemia and ketoacidosis, which pose serious health hazards.
Stress: Stress hormones cause the release of glucose, which raises blood sugar. Glycemic regulation can be hampered by persistent stress.
Physical Inactivity: Living a sedentary lifestyle decreases insulin sensitivity, which makes controlling blood sugar levels more difficult.
Illness and Infections: The body’s inflammatory reactions and insulin resistance during infections and illnesses might result in increased blood sugar levels.
The mitigating factors include: –
Healthy Diet: Blood sugar levels can be stabilized by a balanced diet that emphasizes whole foods, fiber, complex carbs, and portion control. Meal preparation is aided by carb counting.
Insulin Management: Glycemic management depends on regular insulin usage, a proper dose, and adherence to recommended routines.
Regular Exercise: Exercise increases insulin sensitivity, promoting effective glucose use and steady blood sugar levels.
Stress Management: The blood sugar fluctuations brought on by stress can be lessened by using relaxation techniques like meditation.
Regular Monitoring: Regular blood glucose testing and continual glucose monitoring systems allow prompt interventions and corrections.
Education and Support: Individuals are empowered to manage their diseases through diabetes education initiatives and healthcare practitioner guidance.
Illness Management: To combat heightened insulin resistance during sickness, careful tracking of blood sugar and insulin dose modifications may be required.
Omega-3 promotes heart health and reduces inflammation—Take Control, Buy Omega-3 Supplements Today!

Standard Treatment Protocol
Insulin therapy is at the core of the typical Type 1 diabetes treatment regimen. The usual treatment protocol’s main elements are listed below: –
Insulin Therapy: Since their bodies cannot generate insulin, individuals with Type 1 diabetes require exogenous or external insulin. The start, peak, and period of action of the various kinds of insulin are characterized. Typical insulin varieties include: –
Rapid-Acting Insulin
Starts functioning in 15 minutes, spikes in around an hour, and lasts for four hours. The insulins lispro, aspart, and glulisine are a few examples.
Short-Acting Insulin
Immediately begins to work, peaks in effectiveness, and continues for 3-6 hours. This group includes regular insulin, often called short-acting insulin.
Intermediate-Acting Insulin
Duration is 12–18 hours, peak is 4–12 hours, and onset is 2–4 hours. NPH insulin is one illustration.
Long-Acting Insulin
Starts operating within 1-2 hours, lasts for around 24 hours, and doesn’t have a clear peak. Insulin detemir and insulin glargine are two examples.
Blood Glucose Monitoring: For changing insulin dosages and upholding glycemic control, regular blood glucose monitoring is crucial. Usually multiple times per day, patients frequently monitor the sugar levels in their blood using glucose meters.
Carbohydrate Counting: To precisely calculate insulin dosages depending on the quantity of carbohydrates taken, patients are trained to count the carbohydrates in their food and snacks.
Insulin Delivery Methods: These consist of the following: –
Multiple Daily Injections (MDI)
Several individuals adopt MDI therapy, which entails administering several doses of insulin using disposable insulin pumps, pens, or syringes each day.
Continuous Subcutaneous Insulin Infusion (CSII)
Many people choose insulin pumps, which can give an ongoing supply of insulin and deliver increased bolus doses as necessary.
Annual Health Checkups: Periodic appointments with healthcare providers help assess overall health and screen for potential complications, such as retinopathy (eye damage), nephropathy (kidney damage), neuropathy (nerve damage), and cardiovascular issues.
Education and Support: Patients and family members can better understand the disease, its treatments, and self-management techniques thanks to diabetes awareness and assistance programs. These initiatives enable people to choose their diabetes treatment in an informed manner.

Treatment Options
Numerous adjunct treatment alternatives are available to help with glucose control, symptom management, and general health, alongside insulin therapy and conventional diabetes care techniques. Following are some alternatives for complementary medicine: –
Glucagon-Like Peptide-1 (GLP-1) Receptor Agonists: GLP-1 receptor agonists belong to a group of drugs that are mostly used to treat type 2 diabetes. Some, including liraglutide (Victoza), are nevertheless authorized as Type 1 diabetic adjunct medicines. In order to manage blood sugar levels, GLP-1 receptor agonists cause the pancreas to produce more insulin while producing less glucagon. These drugs may help people lose weight, enhance satiety, and decrease blood sugar surges after meals.
Sodium-Glucose Co-Transporter 2 (SGLT-2) Inhibitors: While empagliflozin (Jardiance), an SGLT-2 inhibitor, is predominantly used to treat type 2 diabetes, it has also shown potential as an additional therapy for type 1 diabetes. SGLT-2 inhibitors cause the kidneys to reabsorb less glucose, which lowers blood sugar levels through increased urine excretion of glucose. They may enhance glycemic control, decrease the need for insulin, and maybe assist the cardiovascular system.
Over-the-Counter Formulations: Some over-the-counter supplements, often containing ingredients like chromium, alpha-lipoic acid, and berberine, are marketed as blood sugar stabilizers.
Nutritional Supplements: These are as follows: –
Vitamin D
For general health and potential immunological support, optimal vitamin D levels remain crucial. Many people having Type 1 diabetes experience decreased vitamin D levels, thus supplements could be required.
Boost your body’s resilience with Vitamin D—Support Balanced Glucose Levels, Shop Now!

Omega-3 Fatty Acids
For those with type 1 diabetes, omega-3 supplements typically available in fish oil possess anti-inflammatory characteristics and may enhance heart function.
Natural Remedies: These include the following: –
Fenugreek
Although further research is needed to confirm the usefulness of fenugreek seeds, they have demonstrated potential for decreasing blood sugar levels.
Cinnamon
Cinnamon may enhance insulin sensitivity and lower fasting blood sugar quantities, according to certain research. To prove its effectiveness, more research is necessary.
Herbal Therapies: These are listed below: –
Gymnema Sylvestre
An Indian plant called Gymnema Sylvestre is thought to lessen sugar absorption within the intestines, which may result in better blood sugar regulation.
Bitter Melon
It has been researched whether bitter melon, a herb with a long history of usage in traditional medicine, contains the ability to reduce the levels of blood sugar. It can be taken as a drink or supplement, among other things.
However, it is important to stress that, despite the possibility of advantages, these complementary therapies should not take the place of insulin treatment or other prescription pharmaceuticals. In order to develop individualized treatment programs that are in line with each patient’s health objectives and preferences, collaboration between Type 1 diabetes patients and their healthcare professionals is imperative. People should also be vigilant about any possible interactions between other drugs and adjunct therapy.
Conclusion
Type 1 diabetes represents a lifelong autoimmune condition requiring diligent management and a comprehensive approach to maintain glycemic control and prevent complications. With advancements in insulin therapies, continuous glucose monitoring, and education, individuals can achieve improved outcomes and enhanced quality of life. A well-balanced diet, regular exercise, and stress management play integral roles in complementing medical treatments.
Collaboration between patients and healthcare providers is essential for tailoring treatment strategies to individual needs, ensuring effective disease management. Moreover, the exploration of adjunct therapies, when combined responsibly with standard care, may provide additional support in managing blood sugar levels. With informed choices and proactive care, individuals with Type 1 diabetes can lead fulfilling and healthy lives.

Additional resources for further reference
https://www.ncbi.nlm.nih.gov/books/NBK507713
https://www.healthdirect.gov.au/type-1-diabetes
https://www.thelancet.com/journals/lancet/article/piiS0140-6736(18)31320-5/fulltext
https://www.nature.com/articles/nrdp201716
Important Note: The information contained in this article is for general informational purposes only, and should not be construed as health or medical advice, nor is it intended to diagnose, prevent, treat, or cure any disease or health condition. Before embarking on any diet, fitness regimen, or program of nutritional supplementation, it is advisable to consult your healthcare professional in order to determine its safety and probable efficacy in terms of your individual state of health.
Regarding Nutritional Supplements Or Other Non-Prescription Health Products: If any nutritional supplements or other non-prescription health products are mentioned in the foregoing article, any claims or statements made about them have not been evaluated by the U.S. Food and Drug Administration, and such nutritional supplements or other health products are not intended to diagnose, treat, cure, or prevent any disease.