Proton beam therapy, an advanced form of radiation therapy, has garnered attention for its precision in targeting tumors while minimizing damage to surrounding tissues. As research in oncology continues to advance, this technology has emerged as a promising option for various cancer types. The evolution of proton radiation therapy reflects a significant stride in personalized medicine, especially for patients with tumors located near critical organs or in pediatric populations. However, as with all medical innovations, proton therapy carries certain limitations that must be carefully considered by both clinicians and patients. This comprehensive analysis explores the transformative impact of proton beam therapy while critically evaluating its challenges, including cost, access, and clinical applicability.
You may also like: Cancer Research Breakthroughs: How Modern Advancements Are Transforming Treatment
Understanding Proton Beam Therapy: A Scientific Overview
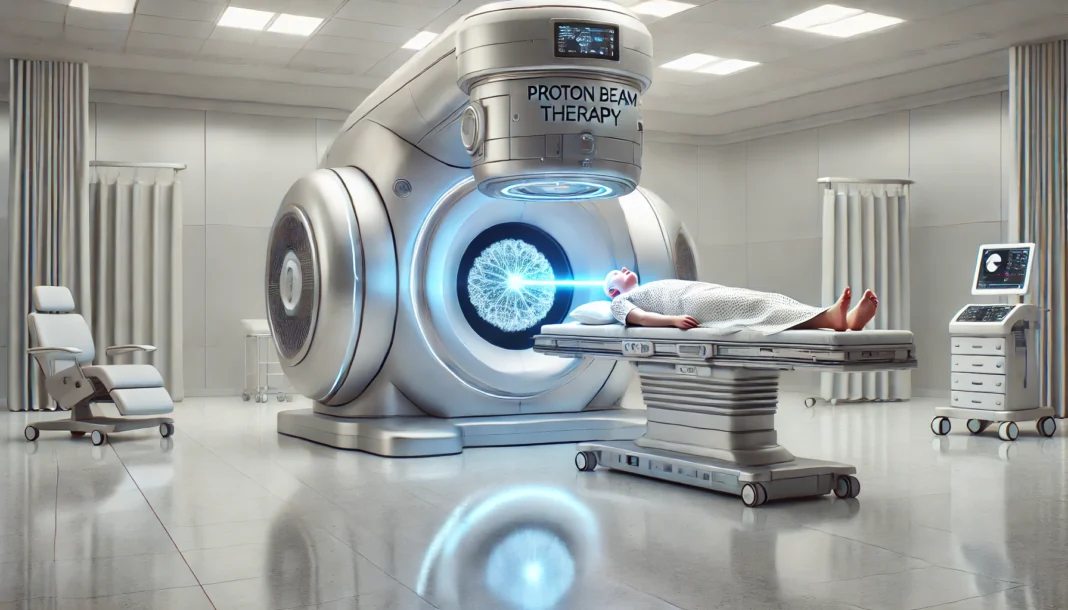
At its core, proton therapy for cancer utilizes protons—positively charged particles—as a highly targeted form of radiation. Unlike conventional photon therapy, which employs X-rays that release energy throughout the body as they pass through tissue, protons deposit the majority of their energy directly at the tumor site. This precise energy release, known as the Bragg peak, allows clinicians to deliver higher doses to tumors with reduced collateral damage to healthy tissue. The physics behind this treatment modality is not merely theoretical; it has been verified through decades of laboratory studies and clinical implementation, supported by the use of a specialized proton therapy machine or proton beam accelerator.
In clinical practice, a proton beam machine directs a focused stream of protons at the tumor. These machines require substantial infrastructure and are typically housed in dedicated cancer centers with the requisite shielding and engineering. One of the critical advantages of proton radiation treatment is its ability to spare normal tissues, particularly in anatomically sensitive areas such as the brain, spine, and eyes. As a result, cancer proton beam therapy is often considered for complex tumors or in pediatric oncology, where minimizing long-term side effects is crucial.
Comparing Proton Therapy vs Radiation: The Photon Therapy Debate
One of the most frequently asked questions among patients and healthcare providers is: is proton therapy better than radiation? To answer this, it is essential to understand the differences between proton vs photon radiation therapy. Photon therapy, the traditional form of external beam radiation, uses X-rays that pass through the body, depositing energy along their path. While effective in treating many cancers, this approach often exposes surrounding tissues to radiation, increasing the risk of side effects.
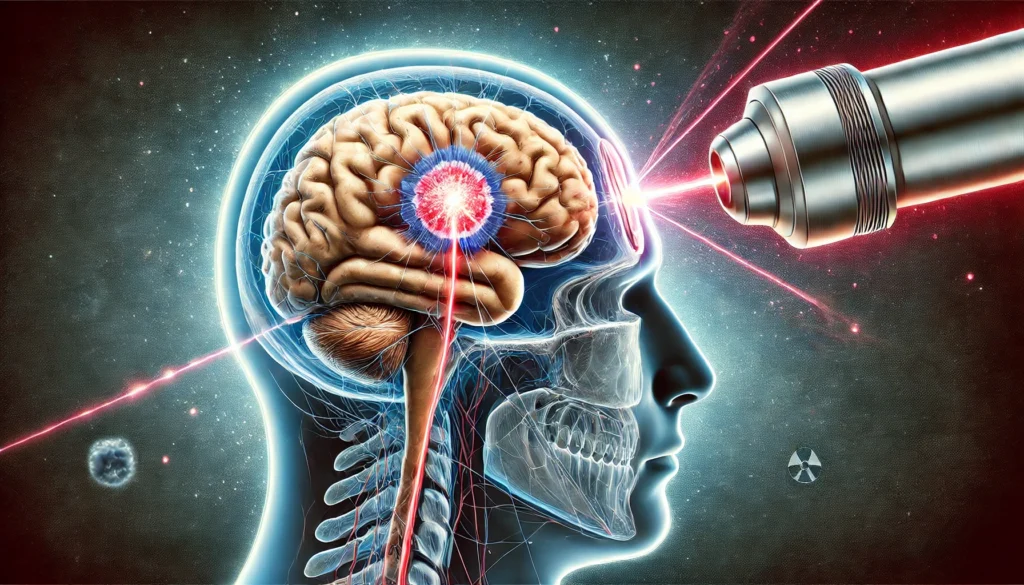
Proton vs photon radiation comparison reveals that the former provides a more localized dose distribution, with a sharp fall-off of radiation beyond the tumor. This feature becomes particularly advantageous when treating tumors near sensitive structures such as the brainstem, spinal cord, or optic nerves. However, it is important to note that clinical superiority in terms of survival outcomes has not been universally demonstrated across all cancer types. While proton therapy reduces radiation exposure to non-target tissues, long-term comparative data for proton therapy vs radiation in terms of efficacy are still emerging.
The Mechanics Behind the Technology: How Does Proton Beam Therapy Work?
To appreciate the therapeutic potential of proton therapy, one must explore the underlying question: how does proton beam therapy work? The answer lies in both the physics of particle interaction and the technological sophistication of the treatment delivery system. When protons are accelerated to high energies using a cyclotron or synchrotron—a form of proton beam accelerator—they travel through magnetic fields and are directed toward the tumor with remarkable precision.
As the protons penetrate bodily tissues, they lose energy gradually until they reach the tumor, where they release the bulk of their energy in a controlled burst—the Bragg peak. This phenomenon is what distinguishes proton radiation therapy from conventional X-ray treatments. Sophisticated imaging and planning software are employed to map the tumor’s exact shape and location, allowing oncologists to conform the dose with sub-millimeter accuracy. The use of pencil beam scanning, a modern advancement in proton beam technology, further refines this targeting by painting the tumor layer by layer with narrow streams of protons.

Limitations and Considerations: Disadvantages of Proton Beam Therapy
Despite its clinical appeal, the disadvantages of proton beam therapy must be carefully acknowledged. One of the primary concerns is cost. Proton therapy machines are expensive to build and maintain, often exceeding $100 million in initial investment. As a result, access to proton treatment is geographically and economically limited, with only select cancer centers offering this technology. Insurance coverage may also be inconsistent, particularly for cancers that are not explicitly approved for proton therapy reimbursement.
In addition, proton therapy disadvantages may include logistical challenges such as longer treatment planning times and more complex setup requirements. Proton radiation side effects, while generally fewer than with photon therapy, are not entirely absent. Fatigue, skin irritation, and localized inflammation may still occur, and in some cases, the high dose delivered to the tumor may increase the risk of necrosis or fibrosis. These risks underscore the importance of meticulous treatment planning and experienced clinical teams.
Reimagining the Future of Cancer Treatment: Final Reflections on Proton Radiation Therapy
As the landscape of oncology continues to evolve, proton beam therapy has firmly established itself as a remarkable innovation with the power to transform cancer treatment. Its capacity for precise dose delivery, coupled with a reduction in collateral damage to healthy tissues, positions proton radiation therapy as a leading option in cases where anatomical complexity or patient vulnerability demands exceptional care. From pediatric oncology to intricate brain tumors and emerging uses in thoracic and gastrointestinal cancers, the potential of this technology continues to unfold.
Nevertheless, it is imperative to approach the growing enthusiasm around proton therapy with a discerning lens. While the technology is undoubtedly impressive, the disadvantages of proton beam therapy—including high costs, limited availability, and gaps in long-term comparative data—must be acknowledged and addressed. The integration of this advanced modality into mainstream clinical practice requires robust evidence, sustainable funding models, and equitable access for diverse patient populations.
Frequently Asked Questions: Expanding Understanding of Proton Beam Therapy
1. How do patient experiences differ when undergoing proton therapy compared to photon therapy?
Patient experiences with proton therapy often involve fewer acute side effects during treatment, particularly when the tumor is located near sensitive structures. For example, patients receiving proton radiation therapy for head and neck cancers may report less severe dry mouth or swallowing difficulty than those undergoing photon therapy. However, it’s important to note that the experience also depends on the facility’s technology and the treatment planning team’s expertise. Proton therapy machines may require longer setup and verification times, which can increase daily session durations. Additionally, because access to a proton beam machine is limited, patients may need to travel far from home, adding logistical and emotional burdens that are less common with more widely available photon therapy options.
2. What is the role of artificial intelligence in enhancing proton beam therapy outcomes?
Artificial intelligence (AI) is emerging as a critical tool in optimizing proton radiation treatment plans. Machine learning algorithms can analyze vast datasets to predict how tumors and healthy tissues will respond to different dose distributions. This allows clinicians to fine-tune proton therapy for cancer with greater accuracy, improving the therapeutic ratio. AI also assists in real-time imaging and adaptive radiotherapy, ensuring that each proton beam conforms precisely to the tumor’s shape, even as anatomy shifts over time. As these technologies evolve, AI will likely reduce planning errors, personalize treatment regimens, and help mitigate the disadvantages of proton beam therapy by making the therapy more efficient and accessible.
3. Can proton therapy be used as part of combination treatments with chemotherapy or immunotherapy?
Yes, proton treatment therapy is increasingly integrated into combination regimens alongside chemotherapy and immunotherapy. This multidisciplinary approach is especially valuable in aggressive cancers where maximizing tumor control is essential. By limiting exposure to surrounding tissues, proton beam therapy allows for higher systemic therapy doses or concurrent treatment without compounding toxicities. Research in cancer proton beam therapy is now exploring how timing and sequencing with immunotherapy might enhance the immune response against tumors. While still an emerging area, these combination strategies have the potential to redefine what proton beam therapy is used for, particularly in recurrent or treatment-resistant cancers.
4. Are there specific pediatric considerations when using proton radiation therapy?
In pediatric oncology, proton therapy is often preferred due to children’s heightened vulnerability to radiation-related side effects. Proton radiation therapy side effects in children, such as growth abnormalities or cognitive deficits, are minimized compared to conventional radiation. Because proton radiation treatment can spare developing tissues and organs, it offers a safer path for long-term survivorship. For instance, using a proton beam accelerator in brain tumors can help preserve IQ and academic performance in young patients. However, proton therapy disadvantages in pediatrics may include the need for sedation during treatment and limited access to facilities, which may delay timely care.
5. How is research evolving to expand the list of cancers treatable with proton beam therapy?
Ongoing clinical trials are central to defining what type of cancer can be treated with proton therapy beyond traditional indications like brain and prostate cancers. Investigations now include breast cancer, esophageal cancer, and even certain lymphomas. These studies aim to determine whether proton radiation therapy can offer not just safer but also more effective treatments in these populations. Proton therapy machines are also being developed in more compact formats, allowing community hospitals to participate in research and extend access. As data accumulates, the boundaries of what proton radiation therapy is used for will likely continue to expand, offering new hope for previously hard-to-treat conditions.
6. What role do insurance companies play in determining access to proton therapy?
Despite its clinical promise, access to proton therapy is often shaped by insurance coverage policies. Many insurers require prior authorization and may deny claims if the cancer type is not among those with established proton beam therapy cancer treatment guidelines. This creates disparities in who can receive proton treatment, particularly in the U.S., where policy variations are vast. Some insurers argue that the proton therapy disadvantages in terms of cost do not justify its use without stronger clinical outcome data. Consequently, patient advocacy groups and professional organizations are working to increase transparency and ensure equitable access to this advanced form of cancer treatment.
7. How does the infrastructure of a proton therapy facility impact the quality of care?
The quality of a proton radiation therapy facility plays a critical role in treatment success. A well-equipped center includes not only a state-of-the-art proton beam machine but also integrated imaging systems, robust quality assurance protocols, and a multidisciplinary team trained in proton therapy for cancer. The use of advanced proton radiation therapy machines and beam-shaping technologies like pencil beam scanning directly influences treatment precision. Conversely, outdated equipment or undertrained staff may increase the risk of suboptimal dosing, which can affect outcomes. Therefore, evaluating a center’s infrastructure is essential when considering where to undergo proton beam therapy.
8. What are the psychological impacts of undergoing proton treatment for cancer patients?
Undergoing proton treatment can be emotionally complex. On one hand, patients often feel hopeful knowing that proton beam therapy offers a cutting-edge option with potentially fewer side effects. On the other, the novelty of the treatment, travel requirements, and limited availability can create stress and uncertainty. Moreover, patients may struggle with insurance denials, leading to frustration that detracts from their healing process. These factors underscore the importance of psychosocial support and clear communication from healthcare teams. As proton radiation therapy becomes more mainstream, mental health support must evolve in parallel to improve overall patient well-being.
9. How are international healthcare systems addressing the limitations of proton therapy?
Globally, healthcare systems are exploring innovative ways to overcome the disadvantages of proton beam therapy. Countries like Japan and the Netherlands have incorporated proton therapy into public healthcare, reducing the financial burden on patients. Some nations are investing in mobile or compact proton beam accelerators to bring treatment closer to underserved populations. International collaborations are also fueling research into cost-effectiveness and expanding knowledge about proton vs photon radiation outcomes. These strategies are creating more inclusive models of care, demonstrating that with thoughtful planning, proton therapy can be both accessible and sustainable.
10. What technological advancements are on the horizon for proton beam therapy?
Future innovations in proton beam therapy are poised to enhance its precision, accessibility, and affordability. Developments include ultra-fast imaging systems that track tumor motion in real time and adaptive treatment algorithms that adjust doses based on daily anatomical changes. Researchers are also exploring FLASH proton therapy, a technique that delivers high doses in fractions of a second, potentially reducing toxicity even further. These advances not only improve the therapeutic index but also reduce the time patients spend undergoing proton radiation treatment. As these technologies mature, they may help address lingering proton therapy disadvantages while broadening the scope of what is proton beam therapy used for in modern oncology.
The future of proton therapy for cancer lies not only in technological refinement but in rigorous scientific inquiry. Ongoing clinical trials will be crucial in determining what type of cancer can be treated with proton therapy most effectively and under what conditions it offers clear advantages over conventional methods. The development of more compact and cost-effective proton therapy machines may also democratize access, bringing this promising treatment to a broader spectrum of patients across the globe.
In reflecting on the path forward, we are reminded that the goal of cancer treatment is not merely to cure disease but to do so with compassion, intelligence, and integrity. Proton beam therapy, with all its promise and limitations, is a vital part of that journey—a testament to how far we’ve come and how far we still have to go in the pursuit of healing.
precision cancer treatment, advanced radiation therapy, pediatric oncology solutions, tumor-targeted therapies, cancer care innovations, non-invasive cancer treatments, radiological oncology techniques, emerging cancer technologies, brain tumor therapy options, cancer survivorship care, personalized oncology approaches, medical physics in oncology, radiation oncology research, patient-centered cancer care, treatment planning in oncology, innovative cancer solutions, low-toxicity cancer therapies, high-tech cancer equipment, oncology patient experience, healthcare technology in cancer treatment
Further Reading:
Proton therapy for cancer treatment
Proton Therapy: The Future Of Precision Cancer Treatment
Exploring treatment options in cancer: tumor treatment strategies
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.