Introduction: Understanding Age and Diabetes
Diabetes is a chronic disease that affects millions of people worldwide. Among the different types of diabetes, type 2 diabetes stands out as one of the most prevalent. While the condition can develop at any age, research has shown that the average age of diabetes diagnosis is steadily increasing. This trend highlights the significant role that age plays in the development and management of type 2 diabetes. The relationship between age and diabetes is complex, and understanding this connection is crucial for both prevention and management.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
The average age of diabetes diagnosis, especially for type 2 diabetes, has been a topic of considerable research over the past few decades. As people age, the risk of developing type 2 diabetes increases, primarily due to changes in metabolism, insulin resistance, and other age-related factors. In this article, we will explore how age impacts diabetes diagnosis, what the average age of diagnosis means for your health, and how lifestyle changes can help manage and prevent the condition as you get older.
The Growing Trend: When Is Type 2 Diabetes Diagnosed?
The average age of type 2 diabetes diagnosis has been a subject of growing concern in medical research. Historically, type 2 diabetes was considered a condition that primarily affected adults over 40. However, with changing lifestyle patterns, dietary habits, and increasing obesity rates, the onset of type 2 diabetes is now being observed in younger populations. This shift underscores the importance of addressing diabetes at earlier stages of life and understanding the risks associated with aging.
Recent studies indicate that the average age of diabetes diagnosis for type 2 diabetes in the United States is around 45 years old. However, this figure can vary based on a variety of factors, including genetics, lifestyle choices, and environmental influences. The age at which individuals are diagnosed with diabetes can provide important insights into the underlying risk factors for the disease and how it develops over time.
The relationship between age and diabetes diagnosis is further complicated by the fact that many people with type 2 diabetes may not be diagnosed until later in life, especially if they are asymptomatic or have only mild symptoms. This delayed diagnosis can make managing the condition more challenging, as diabetes complications tend to worsen over time, particularly if the disease remains untreated or poorly controlled.
Age and the Development of Type 2 Diabetes: Risk Factors
As individuals age, several risk factors for type 2 diabetes become more pronounced. These factors include increased insulin resistance, reduced physical activity, and changes in body composition. Insulin resistance, a condition where the body’s cells do not respond effectively to insulin, is one of the primary contributors to the development of type 2 diabetes. As people age, their bodies become less efficient at using insulin, leading to higher blood sugar levels over time.
Another factor that plays a significant role in the onset of diabetes as people age is weight gain. The average age of a diabetic often correlates with increased body fat, especially around the abdomen. Abdominal fat is particularly harmful because it contributes to the development of insulin resistance. Therefore, maintaining a healthy weight is crucial for older adults in preventing or managing type 2 diabetes.
Physical inactivity also increases the risk of developing type 2 diabetes. As individuals age, they may experience a decrease in physical activity levels, which can exacerbate the risk factors for diabetes. Regular exercise helps improve insulin sensitivity, manage weight, and reduce the risk of developing type 2 diabetes, making it a key preventive measure for older adults.
Additionally, family history plays a significant role in the risk of developing diabetes. Those with a family history of type 2 diabetes are more likely to be diagnosed with the condition, especially as they age. Genetic predisposition, combined with lifestyle factors, can create a perfect storm for the development of type 2 diabetes as individuals move into middle and later adulthood.

The Role of Diet in Diabetes Diagnosis and Prevention
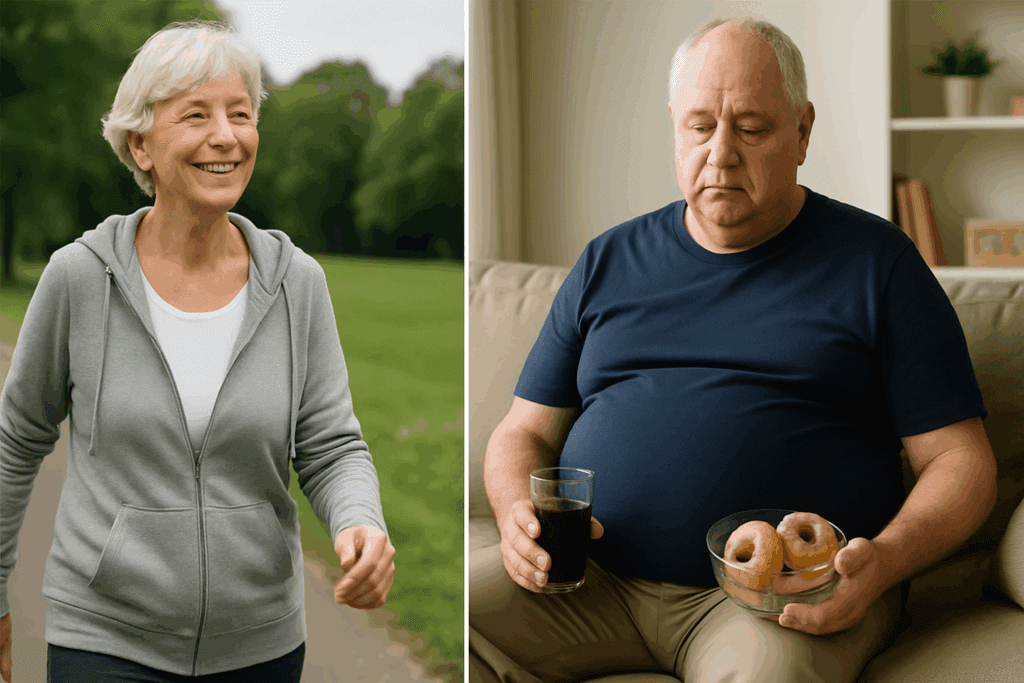
Diet plays an essential role in the development and management of type 2 diabetes, especially as individuals age. The average age of diabetes diagnosis reflects a pattern of dietary habits that have evolved over time. As people get older, they often become less active, and their dietary habits may change, making them more susceptible to insulin resistance and higher blood sugar levels.
Older adults are more likely to consume diets high in processed foods, sugars, and unhealthy fats. These dietary habits can contribute to weight gain and insulin resistance, both of which are key risk factors for type 2 diabetes. A diet rich in whole grains, fruits, vegetables, lean proteins, and healthy fats can help manage blood sugar levels and prevent the development of diabetes.
The Mediterranean diet, for example, has been shown to reduce the risk of developing type 2 diabetes in older adults. This diet focuses on whole foods, healthy fats like olive oil, and plenty of vegetables and fruits. Adopting a balanced diet can not only help prevent diabetes but also improve overall health and reduce the risk of complications associated with aging.
In addition to the types of foods consumed, the timing and frequency of meals can also impact the risk of diabetes. Eating smaller, more frequent meals throughout the day can help stabilize blood sugar levels and reduce the risk of spikes in insulin and blood sugar. For older adults, focusing on nutrition and making healthy dietary choices is one of the most effective strategies for managing and preventing type 2 diabetes.
Understanding the Average Age of a Diabetic: Insights from Research
The average age of a diabetic has shifted over the years, with more and more younger individuals being diagnosed with type 2 diabetes. This shift can be attributed to several factors, including changes in lifestyle, diet, and physical activity patterns. In many cases, people are being diagnosed with diabetes at an earlier age than previous generations, highlighting the importance of early detection and intervention.
Research has shown that the risk of developing type 2 diabetes increases with age, but this relationship is not always linear. While the majority of type 2 diabetes cases are diagnosed in individuals over the age of 45, the rise in obesity and sedentary lifestyles has led to an increasing number of younger individuals being diagnosed. The increasing prevalence of diabetes among younger populations is a cause for concern, as it suggests that the typical progression of the disease is being altered, and the average age of diabetes diagnosis is decreasing.
Studies have also shown that the average age of a diabetic at the time of diagnosis can vary significantly based on ethnicity, socioeconomic status, and geographic location. For instance, individuals of certain ethnic backgrounds, such as African American, Hispanic, and Native American populations, may be diagnosed with type 2 diabetes at younger ages than other demographic groups. Understanding these variations in the average age of diabetes diagnosis is crucial for tailoring prevention strategies and ensuring that individuals at higher risk are monitored more closely.

Prevention and Management: What You Can Do as You Age
As the average age of diabetes diagnosis continues to shift, it’s more important than ever for individuals to take proactive steps to prevent or manage the condition. While age is a significant risk factor for developing type 2 diabetes, there are several lifestyle changes that can help reduce the risk and improve the management of the disease, regardless of when it is diagnosed.
Maintaining a Healthy Weight: As mentioned earlier, excess weight, particularly abdominal fat, is a major contributor to insulin resistance and the development of type 2 diabetes. By maintaining a healthy weight, individuals can reduce their risk of developing the condition and improve their overall health. This can be achieved through a combination of a balanced diet and regular physical activity.
Regular Exercise: Physical activity is one of the most effective ways to prevent type 2 diabetes and manage the condition. Regular exercise improves insulin sensitivity, helps with weight management, and reduces the risk of complications associated with diabetes. Older adults should aim for at least 150 minutes of moderate-intensity exercise each week, which can include walking, swimming, or cycling.
Early Detection: Given the rising prevalence of type 2 diabetes, early detection is essential for managing the condition and preventing complications. Regular screening for diabetes, particularly for those at higher risk due to family history, obesity, or age, can help identify the condition before it becomes more severe. Early diagnosis allows for timely intervention and better management of blood sugar levels.
Frequently Asked Questions (FAQ) on the Average Age of Diabetes Diagnosis
1. What is the average age of diabetes diagnosis for type 2 diabetes?
The average age of diabetes diagnosis for type 2 diabetes has been steadily increasing over the years. Recent studies suggest that the average age of diagnosis is typically around 45 to 50 years old. However, this age can vary based on lifestyle factors, such as diet, exercise, and weight management. It’s also important to note that genetic predispositions and family history play a role in determining when an individual may be diagnosed. While the average age of a diabetic diagnosis tends to occur in middle adulthood, the onset of type 2 diabetes is becoming more common in younger individuals, especially with rising obesity rates.
2. How does age and diabetes relate to risk factors for developing type 2 diabetes?
Age and diabetes are closely linked, as the risk for developing type 2 diabetes increases as people age. Older individuals tend to experience a decrease in insulin sensitivity and a higher likelihood of obesity, both of which are significant risk factors for type 2 diabetes. The average age of diabetes diagnosis reflects these changes in metabolism, as well as the accumulation of lifestyle-related factors over time. In addition, as people age, they may become less active and less vigilant about their diet, further increasing the risk. Early intervention is crucial to managing these risks effectively, and lifestyle adjustments can help delay the onset of the disease.
3. How is the average age of diabetes diagnosis shifting over time?
Over the years, there has been a noticeable shift in the average age of diabetes diagnosis. The average age of a diabetic diagnosis used to be higher, generally occurring in people aged 50 or older. However, with rising obesity rates, sedentary lifestyles, and poor dietary habits, more younger individuals are being diagnosed with type 2 diabetes. Recent trends suggest that the average age diabetes type 2 is now being diagnosed in individuals as young as 30 or 40. This shift is concerning because it suggests that younger generations are facing an increasing risk due to their lifestyle choices and environmental factors.
4. What is the impact of lifestyle on the average age of diabetes diagnosis?
Lifestyle choices play a significant role in determining the average age of diabetes diagnosis. The incidence of type 2 diabetes is closely tied to physical inactivity, poor diet, and obesity. People who maintain a sedentary lifestyle and consume high amounts of processed foods are more likely to develop diabetes at an earlier age. As more individuals embrace unhealthy eating habits and fail to exercise regularly, the average age of diabetes diagnosis continues to decline. Making healthier lifestyle choices, such as engaging in regular physical activity and eating a balanced diet, can delay the onset of diabetes, even in older adults.
5. Can type 2 diabetes be diagnosed at a younger age?
Yes, type 2 diabetes can be diagnosed at a younger age, and this is becoming more common. The average age of diabetes diagnosis for type 2 has steadily declined due to factors like increasing rates of childhood obesity and poor dietary habits. It is no longer uncommon for individuals in their 30s or early 40s to be diagnosed with type 2 diabetes, whereas the condition was once considered an illness primarily affecting older adults. Monitoring for risk factors such as obesity, family history, and lifestyle habits is important, even in younger individuals, to ensure early detection and intervention.
6. How does family history affect the average age of diabetes diagnosis?
Family history plays a crucial role in the average age of a diabetic diagnosis. Individuals with close family members who have type 2 diabetes are more likely to be diagnosed at an earlier age. Genetic factors contribute significantly to the development of insulin resistance, which is a key factor in type 2 diabetes. Even if a person leads a healthy lifestyle, a family history of diabetes may cause them to develop the condition earlier than others, potentially affecting the average age of their diagnosis. Understanding one’s family medical history can help guide proactive measures and encourage early screening, particularly for those with higher genetic risk.
7. What role do hormones and aging play in the average age of diabetes diagnosis?
Hormones and aging are key factors influencing the average age of diabetes diagnosis. As people age, their bodies undergo various hormonal changes, particularly in terms of insulin resistance. Aging leads to a decrease in muscle mass and an increase in fat accumulation, both of which contribute to insulin resistance. As a result, blood sugar levels can rise, eventually leading to type 2 diabetes. This natural decline in insulin sensitivity with age is one reason why the average age of diabetes diagnosis tends to rise in older adults. Monitoring hormonal changes and managing weight and activity levels can help mitigate the effects of aging on diabetes risk.
8. Is the average age of diabetes diagnosis the same globally?
The average age of diabetes diagnosis varies globally due to differences in lifestyle, diet, genetics, and healthcare access. For example, the average age of a diabetic diagnosis in the United States may be different from countries in Europe or Asia, where diabetes might be diagnosed at an earlier or later age depending on local dietary patterns and healthcare systems. In countries with high obesity rates and lower physical activity levels, such as the U.S., the average age diabetes type 2 is diagnosed is typically lower. In other regions, like parts of Europe or Asia, cultural dietary habits and different rates of obesity influence the age at which diabetes is typically diagnosed.
9. How can early detection affect the average age of diabetes diagnosis?
Early detection is key to managing type 2 diabetes and can potentially alter the average age of diagnosis. Identifying individuals at risk for diabetes before they develop significant symptoms can lead to early intervention, such as lifestyle changes or medication. This proactive approach can not only prevent or delay the onset of the disease but also improve the overall management of the condition. Regular screenings and awareness campaigns aimed at detecting type 2 diabetes early can help shift the focus from reactive to preventive care, reducing the average age at which complications arise. By detecting diabetes earlier, individuals have a greater chance of managing the disease effectively and preventing long-term health issues.
10. What are some preventive measures to delay the average age of diabetes diagnosis?
Preventive measures to delay the average age of diabetes diagnosis include maintaining a healthy diet, regular physical activity, and routine medical check-ups. Individuals should aim to eat a balanced diet rich in fruits, vegetables, whole grains, and lean proteins while avoiding excessive processed foods and sugary drinks. Regular exercise is also essential in preventing insulin resistance and maintaining a healthy weight. Additionally, managing stress, sleeping well, and avoiding smoking can all contribute to a lower risk of developing type 2 diabetes. Through these lifestyle changes, people can significantly delay the onset of diabetes and potentially improve the average age of a diabetic diagnosis.
Conclusion: The Importance of Age Awareness in Diabetes Diagnosis
Understanding the average age of diabetes diagnosis and how age impacts diabetes is crucial for both prevention and management. As the global population ages, the risk of developing type 2 diabetes increases, making it more important than ever to adopt healthy lifestyle habits early in life. By focusing on maintaining a healthy weight, eating a balanced diet, and staying physically active, individuals can significantly reduce their risk of developing type 2 diabetes and improve their overall health.
The trend of earlier diabetes diagnosis among younger populations emphasizes the need for increased awareness and preventive measures. Regular screening, early detection, and lifestyle changes are all essential components of managing diabetes and preventing complications. By being proactive and informed about the relationship between age and diabetes, individuals can take control of their health and reduce the risk of this chronic condition.
Further Reading:
How Age Relates to Type 2 Diabetes
Type 2 diabetes – Symptoms and causes
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.