Hypertension remains one of the most prevalent and consequential conditions in cardiovascular medicine. Among its various forms, essential hypertension stands out not only for its ubiquity but also for the clinical complexity it presents. Often described as an elevated pressure without apparent cause, essential hypertension—also known as benign essential hypertension—poses a unique diagnostic and management challenge. While the term “benign” may suggest a less threatening nature, the reality is more nuanced. This article explores the essential HTN definition, investigates the implications of benign HTN, and offers an evidence-based perspective on how this condition affects overall cardiovascular health.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Defining Essential Hypertension and Its Clinical Relevance
Essential hypertension is defined as high blood pressure that arises without a clearly identifiable secondary cause. Unlike secondary hypertension, which can be traced to specific conditions such as kidney disease, hormonal disorders, or certain medications, essential hypertension develops insidiously and is influenced by a confluence of genetic, environmental, and lifestyle factors. This form of hypertension accounts for approximately 90 to 95 percent of all diagnosed cases, making it a focal point of clinical concern.
The essential HTN definition centers around persistently elevated blood pressure readings—typically defined as a systolic blood pressure above 130 mmHg or a diastolic pressure above 80 mmHg—without a discernible origin. It is critical to understand that this condition does not imply the absence of risk. Even in the absence of symptoms, prolonged elevated pressure can silently damage vital organs, including the heart, brain, kidneys, and eyes.
Benign Essential Hypertension: Terminology and Implications
The terminology of benign essential hypertension can be somewhat misleading to patients and even to clinicians unfamiliar with the evolution of medical language. Historically, the term “benign” was used to distinguish this form from malignant hypertension, a rapidly progressing and life-threatening condition characterized by extremely high pressures and end-organ damage. However, benign essential HTN should not be regarded as harmless. Over time, untreated or poorly managed benign hypertension can lead to serious complications, including left ventricular hypertrophy, chronic kidney disease, and increased risk for myocardial infarction and stroke.
Although the progression of benign HTN tends to be gradual, its cumulative effects are significant. The designation of “benign” merely reflects the slower course and absence of immediate crisis, not the overall risk profile. Modern guidelines emphasize the importance of treating benign essential hypertension proactively to prevent long-term morbidity and mortality.

Etiology: What Causes Essential Hypertension?
Despite its frequency, the precise etiology of essential hypertension remains elusive. Researchers agree that it is a multifactorial condition with both non-modifiable and modifiable risk factors. Genetic predisposition plays a notable role, with studies indicating that individuals with a family history of hypertension are significantly more likely to develop the condition themselves. Specific gene polymorphisms related to the renin-angiotensin-aldosterone system, sodium handling, and vascular reactivity have been implicated.
Environmental and lifestyle contributors are equally important. Excessive sodium intake, sedentary behavior, chronic stress, obesity, and excessive alcohol consumption all contribute to the development and persistence of high blood pressure. Moreover, age and ethnicity influence prevalence and severity; for instance, essential hypertension is more common and tends to be more severe in African American populations.
Understanding that essential hypertension is also known as a lifestyle disease in many public health narratives underscores the importance of prevention and early intervention. Addressing modifiable risk factors through public education and clinical engagement can significantly alter the disease trajectory.
The Diagnostic Process: Recognizing Benign Essential HTN
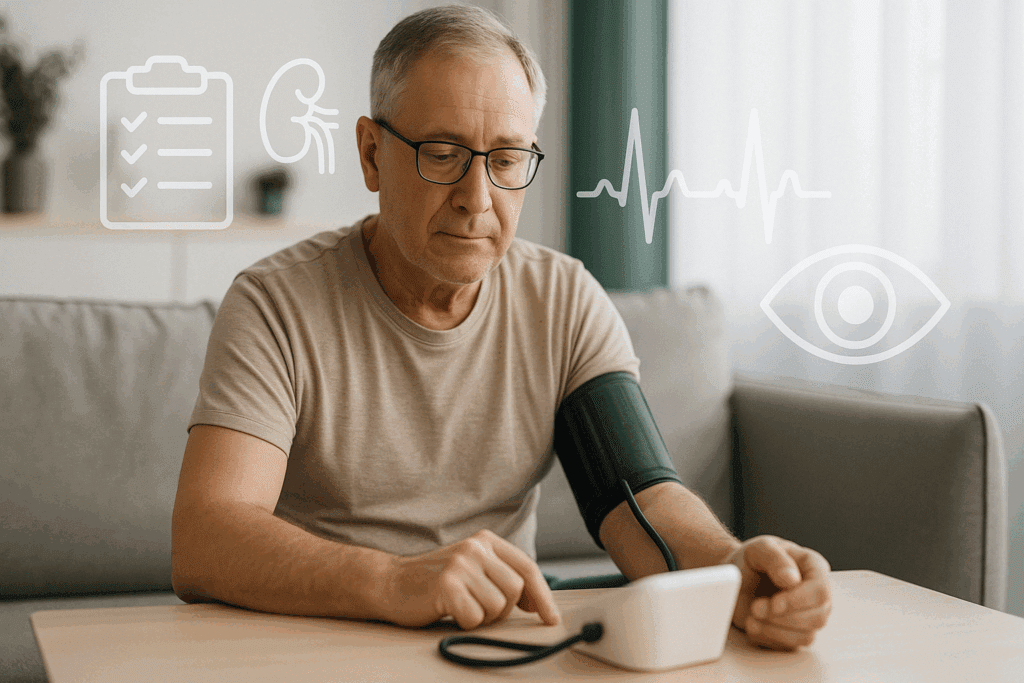
Diagnosing benign essential hypertension involves more than simply noting elevated readings during a single office visit. Clinicians typically require multiple blood pressure measurements over several visits to confirm the diagnosis. Ambulatory blood pressure monitoring and home-based measurements may also be employed to avoid misdiagnosis due to white-coat hypertension.
When no secondary cause is identified after a thorough clinical evaluation—including assessments of kidney function, endocrine parameters, and imaging studies—the diagnosis of essential hypertension is confirmed. In such cases, it becomes essential to educate patients that an elevated pressure without apparent cause is said to be essential in nature, distinguishing it from secondary forms of hypertension that may be curable.
It is equally important to assess for signs of target organ damage at the time of diagnosis. Evaluations might include an electrocardiogram to detect left ventricular hypertrophy, urinalysis for proteinuria, and retinal examination for hypertensive changes. These assessments help stratify risk and inform the intensity of therapeutic interventions.
Clinical Course and Prognosis: How Benign Is Benign?
The natural history of benign essential hypertension reveals a chronic, progressive course. Although the progression is typically slower than in malignant hypertension, the absence of acute symptoms often leads to a dangerous sense of complacency. Over years or decades, consistently elevated blood pressure can compromise vascular integrity, promote atherosclerosis, and impair organ function.
Left untreated, benign HTN increases the risk of cardiovascular events, particularly ischemic heart disease, heart failure, stroke, and renal insufficiency. The likelihood and timing of such complications depend on factors such as baseline blood pressure, coexisting medical conditions, and the presence of lifestyle risk factors. Early identification and intervention remain the cornerstones of improving outcomes.
Despite the term “benign,” essential hypertension is not inherently harmless. A diagnosis of HTN—hypertension benign in nature—still requires ongoing monitoring and management. The key distinction lies in the tempo of disease progression rather than in its ultimate consequences.

Management Strategies for Benign Essential Hypertension
The management of benign essential hypertension involves a multifaceted approach that combines lifestyle modifications with pharmacologic therapy when necessary. Non-pharmacologic strategies should be the first line of defense, especially in patients with mild elevations or those in the early stages of the condition.
Lifestyle interventions include dietary changes such as adopting the DASH (Dietary Approaches to Stop Hypertension) diet, which emphasizes fruits, vegetables, lean proteins, and reduced sodium intake. Regular physical activity, ideally at least 150 minutes of moderate-intensity aerobic exercise per week, has been shown to lower blood pressure and improve overall cardiovascular health. Weight loss, smoking cessation, and stress reduction through mindfulness practices or therapy also contribute significantly to blood pressure control.
When lifestyle measures are insufficient or when blood pressure remains significantly elevated, pharmacologic treatment becomes necessary. Commonly used medications include thiazide diuretics, ACE inhibitors, angiotensin receptor blockers, calcium channel blockers, and beta-blockers. The choice of medication is individualized based on patient-specific factors, including age, race, comorbid conditions, and potential side effects.
Long-Term Monitoring and Patient Engagement
Once treatment is initiated, regular monitoring is essential to assess effectiveness and adjust therapy as needed. Blood pressure goals vary slightly depending on individual risk factors, but most guidelines recommend maintaining values below 130/80 mmHg. Periodic reassessment of cardiovascular risk, kidney function, and adherence to lifestyle changes enhances long-term outcomes.
Patient education and empowerment play a critical role in managing benign essential HTN. Encouraging patients to monitor their blood pressure at home, understand their medications, and recognize the importance of adherence can transform passive recipients of care into active partners. Shared decision-making fosters a sense of ownership and increases the likelihood of sustained success.

Public Health Perspectives and Prevention
From a population health standpoint, addressing essential hypertension requires comprehensive strategies that extend beyond the clinical setting. Public health initiatives aimed at reducing sodium consumption in processed foods, promoting physical activity, and increasing access to nutritious foods are critical components of prevention. Community-based interventions, workplace wellness programs, and school-based education campaigns can influence behavior at scale.
Health disparities must also be addressed to ensure equitable care. Racial and socioeconomic factors significantly influence the prevalence and outcomes of hypertension. Ensuring access to care, culturally sensitive education, and affordable medications are essential steps toward narrowing these gaps. Prevention and early detection can reduce the burden of disease and its downstream complications.
Innovations in Research and Future Directions
Ongoing research continues to enhance our understanding of the pathophysiology and treatment of essential hypertension. Advances in genomics, epigenetics, and systems biology are shedding light on previously unknown mechanisms that contribute to blood pressure regulation. Personalized medicine, driven by genetic and phenotypic profiling, holds promise for tailoring interventions to individual patients.
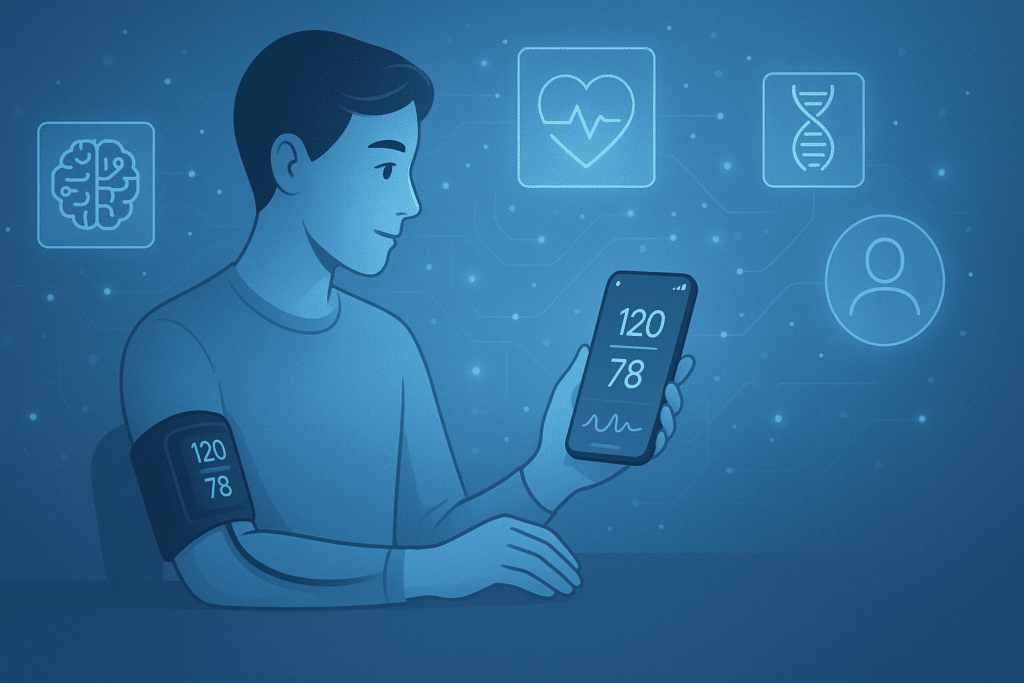
Technological innovations, including wearable blood pressure monitors, mobile health apps, and telemedicine platforms, are revolutionizing hypertension management. These tools facilitate continuous monitoring, real-time feedback, and more timely adjustments to treatment plans. As healthcare moves toward a more patient-centric model, such innovations will likely play an increasingly prominent role in controlling benign hypertension.
Understanding the Interplay Between Lifestyle and Biology
The interface between lifestyle and biology remains a fertile ground for understanding and managing benign essential hypertension. While genetics may set the stage, environmental exposures and personal habits shape the clinical picture. For instance, a person with a genetic predisposition may never develop hypertension if they maintain a healthy weight, avoid excessive salt, and engage in regular physical activity.
Conversely, poor lifestyle choices can override even a favorable genetic background. The concept of epigenetics—where environmental influences can alter gene expression—underscores the importance of modifiable factors. Stress, sleep deprivation, and exposure to pollutants all have measurable effects on blood pressure and vascular health. Recognizing this interplay encourages a more holistic approach to prevention and care.
Patient Stories and Real-World Impact
Real-life patient experiences offer valuable insights into the lived reality of managing benign HTN. Consider the case of a middle-aged man with a family history of hypertension who remained asymptomatic but was found to have elevated blood pressure during a routine check-up. With lifestyle adjustments and a single medication, he achieved good control and avoided complications. His story illustrates that early detection and intervention can lead to favorable outcomes.
Another example involves a woman who struggled with weight gain and stress. Her blood pressure remained elevated despite dietary changes until she incorporated regular exercise and mindfulness meditation into her routine. Over time, her blood pressure normalized without the need for medication. These narratives underscore the importance of personalized care and the power of lifestyle in shaping health trajectories.
Frequently Asked Questions About Benign Essential Hypertension
What are some lesser-known lifestyle changes that can help manage benign essential hypertension?
While common advice includes reducing sodium and increasing physical activity, emerging evidence suggests that micro-lifestyle changes—like maintaining consistent sleep schedules, engaging in forest bathing (spending time in nature), and adopting time-restricted eating—may also benefit those with benign essential hypertension. Practices such as biofeedback and guided breathing exercises have been shown to lower sympathetic nervous system activity, a key driver of elevated blood pressure in individuals with benign HTN. In addition, avoiding exposure to chronic noise pollution—like living near highways or in loud urban areas—may improve long-term outcomes. Individuals with a diagnosis of HTN hypertension benign in form may find improved control when they incorporate these strategies consistently. It’s essential to remember that comprehensive lifestyle approaches complement medication and should be personalized.
Can someone with benign essential HTN still experience symptoms, or is it always silent?
Although benign essential hypertension is often asymptomatic, some individuals report vague or intermittent symptoms such as morning headaches, blurred vision, fatigue, or a sensation of pulsation in the neck. These subtle symptoms often go unrecognized or are attributed to stress or poor sleep. While the essential HTN definition classifies it as a condition without an identifiable cause, this doesn’t preclude occasional physical manifestations, especially when blood pressure rises sharply during stressful periods. It’s important not to ignore these signs, even in the context of benign hypertension, because they can signal either poor blood pressure control or early organ stress. Patients should be encouraged to track any recurring symptoms and report them to their healthcare provider.
Are there psychological effects linked to being diagnosed with benign essential hypertension?
Yes, receiving a diagnosis of benign essential HTN can influence mental health in subtle but significant ways. Patients often struggle with anxiety or worry about long-term complications, particularly if they perceive their condition as a precursor to stroke or heart disease. The label “benign” may ironically minimize the perceived seriousness, which can lead to confusion or neglect of necessary lifestyle changes. Understanding that an elevated pressure without apparent cause is said to be essential hypertension—and that this label doesn’t guarantee safety—can empower patients to stay proactive. Supportive counseling and psychoeducation tailored to people with benign hypertension may improve both emotional well-being and treatment adherence.
How does benign essential hypertension affect cardiovascular risk in women differently than in men?
Gender differences in cardiovascular risk are increasingly acknowledged in the management of benign essential hypertension. While men are more frequently diagnosed at an earlier age, women—particularly postmenopausal women—often experience a steeper increase in blood pressure later in life, placing them at heightened risk for complications. Hormonal shifts, differences in arterial stiffness, and variation in treatment response all play a role. Furthermore, research shows that essential hypertension is also known as a contributor to microvascular disease, which tends to be more prevalent in women and harder to detect. Addressing these gender-based nuances in care can lead to more effective prevention strategies.
Is there a connection between essential hypertension and cognitive decline?
Recent studies have drawn strong links between long-standing essential hypertension and the development of cognitive impairment, particularly vascular dementia. The pathophysiological mechanism involves chronic damage to the small vessels in the brain, leading to reduced perfusion, white matter changes, and eventually, cognitive deterioration. For individuals with benign essential hypertension, the slow and often silent nature of the condition means damage can accumulate unnoticed. Because benign HTN progresses subtly, early and aggressive management becomes critical to preserving brain health. Cognitive screening may be advisable for older patients or those with poorly controlled HTN hypertension benign in origin.
Are there occupational risks that may worsen benign hypertension?
Occupational stress is a significant and often overlooked contributor to the development and persistence of benign essential HTN. High-demand, low-control jobs—such as those in customer service, law enforcement, and healthcare—have been associated with sustained elevations in blood pressure. Sedentary work, long hours, and limited access to healthy food or movement during the workday also play a role. Employers can support cardiovascular health by fostering work-life balance and offering wellness initiatives tailored for workers with benign hypertension. A deeper understanding of how occupational environments exacerbate an elevated pressure without apparent cause is said to be a missing link in comprehensive care models.
What emerging technologies are helping with the management of benign essential HTN?
Digital health tools are transforming how benign essential hypertension is managed. Wearable blood pressure monitors now offer real-time feedback, allowing for better detection of fluctuations throughout the day. Mobile apps can remind patients to take medications, log meals, and even offer meditation exercises designed to reduce sympathetic tone. In addition, machine learning algorithms are being developed to analyze patterns in daily readings and predict future cardiovascular events. These innovations not only empower patients but also provide clinicians with a more nuanced view of how benign HTN behaves over time. The personalization enabled by these tools marks a new frontier in chronic disease management.
How might cultural perceptions influence the treatment of benign hypertension?
Cultural beliefs about health and illness can profoundly affect how individuals respond to a diagnosis of benign essential hypertension. In some communities, the term “benign” may be taken literally, leading to underestimation of the condition’s seriousness and poor adherence to treatment. Conversely, in cultures where chronic illness carries stigma, patients may avoid disclosing their diagnosis or refuse medications due to fears of dependency. Understanding that essential hypertension is also known as a silent but serious condition can help reframe conversations in a culturally sensitive way. Healthcare providers should strive to offer respectful, inclusive care that acknowledges these perceptions while reinforcing medical facts.
Is it possible to reverse benign essential HTN through lifestyle changes alone?
In the early stages, many individuals with benign HTN can achieve normal blood pressure through non-pharmacologic interventions alone. Sustained weight loss, consistent aerobic activity, and salt restriction have all been shown to produce clinically meaningful reductions in blood pressure. However, reversal does not necessarily mean cure—blood pressure may rise again if healthy habits are not maintained. The essential HTN definition implies a long-term tendency toward elevated pressure, so ongoing vigilance is key. That said, early and aggressive lifestyle changes can delay or even eliminate the need for lifelong medication in some patients.
What role do environmental toxins play in the development of benign essential hypertension?
Emerging research suggests that environmental toxins—such as lead, cadmium, and certain air pollutants—may contribute to the pathogenesis of benign essential hypertension. These toxins can induce oxidative stress, inflammation, and endothelial dysfunction, all of which are key mechanisms in the development of high blood pressure. For instance, populations exposed to high levels of airborne particulate matter have higher rates of essential HTN, even after adjusting for socioeconomic status and traditional risk factors. The phrase an elevated pressure without apparent cause is said to be essential hypertension, but ongoing research may soon redefine what is considered an “apparent cause.” As our understanding evolves, public health measures targeting environmental exposure may become an integral part of managing benign hypertension.
A Final Word on Prevention and Vigilance
In sum, benign essential hypertension demands both attention and action. Though it may progress slowly and often without symptoms, it has the potential to cause serious, even life-threatening complications if left unchecked. Recognizing that essential hypertension is also known as a silent killer due to its asymptomatic nature reinforces the need for routine screening and proactive management.
Understanding that an elevated pressure without apparent cause is said to be essential hypertension allows clinicians and patients alike to appreciate the unique nature of this condition. With the right combination of lifestyle changes, medical therapy, and consistent monitoring, benign essential HTN can be effectively managed and its risks mitigated.
Ultimately, the key lies in awareness, engagement, and commitment—from both healthcare providers and individuals. In a world where chronic conditions are becoming increasingly common, taking the time to understand and address benign hypertension is a vital step toward safeguarding cardiovascular health for the long term.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Primary Hypertension (Formerly Known as Essential Hypertension)