Best Blood Pressure Medication Options for Pregnant Women: Maintaining healthy blood pressure during pregnancy is vital for the well-being of both the expectant mother and the developing fetus. Elevated blood pressure, also known as hypertension, can pose serious risks, including preeclampsia, placental abruption, premature birth, and even maternal mortality if left untreated. While lifestyle modifications such as a balanced diet and adequate rest can contribute to managing blood pressure, pharmacological intervention is often necessary for those with chronic or gestational hypertension. However, not all antihypertensive drugs are safe for use during pregnancy, making the selection of pregnancy blood pressure medications a nuanced and carefully considered process.
As the medical community has deepened its understanding of maternal cardiovascular health, researchers and clinicians have identified a variety of pregnancy safe hypertension meds that effectively manage high blood pressure without compromising fetal development. This article explores the pharmacologic landscape for treating hypertension in pregnancy, examining drug safety classifications, recommended medications, potential side effects, and emerging research, all through the lens of medical accuracy, evidence-based guidance, and patient-centered care.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
Understanding Hypertension During Pregnancy: Definitions and Risks
Hypertension in pregnancy is generally categorized into four types: chronic hypertension, gestational hypertension, preeclampsia, and chronic hypertension with superimposed preeclampsia. Chronic hypertension refers to elevated blood pressure diagnosed before pregnancy or before 20 weeks of gestation, while gestational hypertension arises after 20 weeks without the presence of proteinuria or other systemic symptoms. Preeclampsia, a severe complication, involves hypertension and signs of organ dysfunction, such as elevated liver enzymes or kidney impairment. Understanding these distinctions is essential for tailoring appropriate blood pressure treatment strategies.
The risks associated with unmanaged hypertension in pregnancy are multifaceted and can be life-threatening. For the mother, complications include stroke, heart failure, and organ damage. For the fetus, growth restriction, low birth weight, and preterm delivery are common concerns. In severe cases, the condition may lead to intrauterine fetal demise. These risks underscore the importance of timely diagnosis and therapeutic intervention, particularly with pregnancy safe hypertension meds that do not cross the placental barrier or adversely impact fetal physiology.
Criteria for Selecting Pregnancy Safe Hypertension Meds
When determining the most appropriate blood pressure medication for pregnant women, clinicians consider several key factors, including the medication’s mechanism of action, potential teratogenicity, historical safety data, and the mother’s overall health profile. Regulatory agencies such as the U.S. Food and Drug Administration (FDA) have previously categorized drugs into pregnancy risk categories, although more recent guidance emphasizes individualized risk-benefit analyses.
The ideal pregnancy blood pressure medications are those that have a long-standing record of safety and efficacy in pregnant populations. These medications should effectively control blood pressure without impairing placental perfusion or fetal development. Common considerations include the drug’s pharmacokinetics, such as how it is metabolized and excreted, and whether it alters maternal blood volume or systemic vascular resistance. Importantly, patient adherence and tolerance are also central to the selection process, as complex dosing regimens or severe side effects can compromise treatment adherence.
First-Line Blood Pressure Medications for Pregnant Women
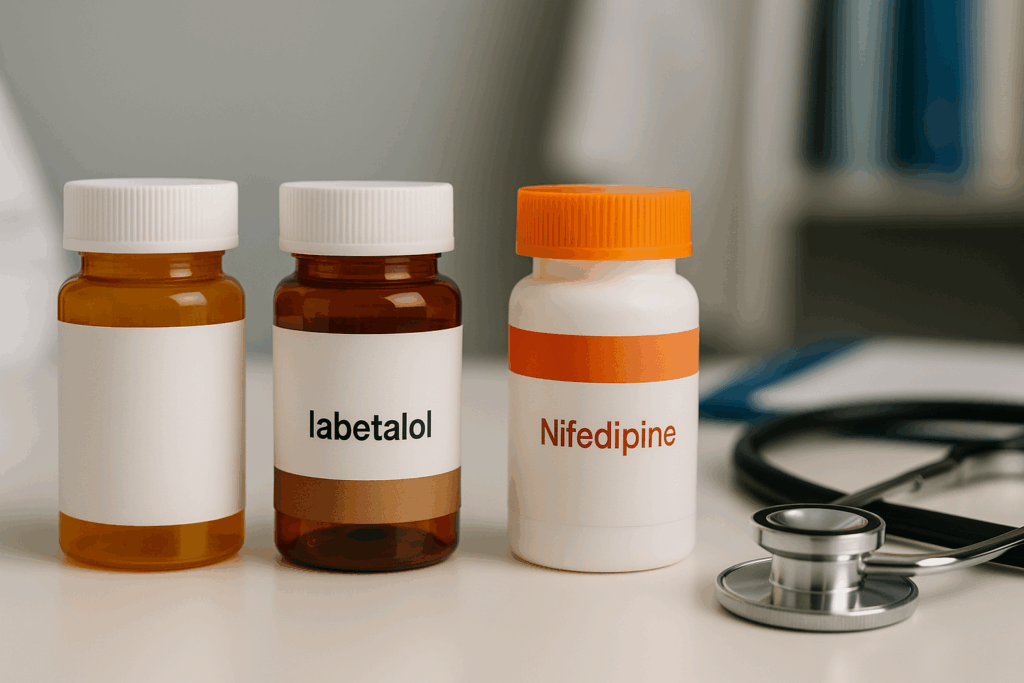
Three antihypertensive agents are widely recognized as first-line treatments for managing high blood pressure in pregnancy: methyldopa, labetalol, and nifedipine. Each of these medications has been extensively studied in pregnant populations and is generally considered safe and effective when used appropriately.
Methyldopa, a centrally acting alpha-2 adrenergic agonist, has a long history of use in obstetric care. It lowers blood pressure by reducing sympathetic nervous system activity and has minimal impact on uteroplacental blood flow. Although methyldopa is not the most potent antihypertensive agent, its safety profile makes it a preferred choice, particularly during the first trimester. Side effects may include sedation, dry mouth, and depression, which should be monitored closely.
Labetalol, a combined alpha- and beta-adrenergic blocker, is another widely used option. It effectively reduces peripheral vascular resistance while maintaining cardiac output, making it particularly useful for women with more severe hypertension. It is often administered orally but may also be given intravenously in acute care settings. While labetalol is generally well-tolerated, it may cause fatigue, dizziness, or mild hypotension.
Nifedipine, a calcium channel blocker, is typically used in its extended-release formulation to manage chronic or gestational hypertension. It acts by dilating arterial blood vessels, thereby reducing systemic resistance. Nifedipine is especially useful in outpatient settings due to its ease of administration and minimal interference with fetal circulation. However, patients may experience headaches, flushing, or palpitations as side effects.

Medications to Avoid During Pregnancy
Not all antihypertensive medications are safe for pregnant women. Some drugs carry significant teratogenic risks and are contraindicated due to their association with congenital malformations or fetal toxicity. Chief among these are angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), and direct renin inhibitors.
ACE inhibitors and ARBs have been linked to serious fetal complications, including renal dysgenesis, oligohydramnios, and pulmonary hypoplasia, particularly when used in the second and third trimesters. These drugs interfere with the renin-angiotensin-aldosterone system (RAAS), which plays a critical role in fetal kidney development. Even a single dose can pose a risk, which is why discontinuation is recommended prior to conception or immediately upon diagnosis of pregnancy.
Other medications, such as diuretics and certain beta-blockers like atenolol, are used with caution. While diuretics may be necessary in some cases, they can reduce plasma volume and compromise placental perfusion. Atenolol, when used in early pregnancy, has been associated with intrauterine growth restriction. The key is to weigh the maternal benefits against the fetal risks and to seek alternatives whenever possible. These distinctions highlight the need for careful selection of blood pressure drugs for pregnancy to avoid preventable complications.

Emerging Research and Evolving Guidelines in Pregnancy Hypertension Management
Recent advances in clinical research have spurred a re-evaluation of how hypertension is managed in pregnancy. Studies such as the CHAP (Chronic Hypertension and Pregnancy) trial have provided valuable insights into the benefits of maintaining tighter blood pressure control, suggesting that treating mild chronic hypertension may reduce the risk of adverse outcomes without harming the fetus.
Updated guidelines from the American College of Obstetricians and Gynecologists (ACOG) and other professional societies now recommend initiating treatment for persistent systolic blood pressure ≥140 mmHg or diastolic pressure ≥90 mmHg, a shift from earlier thresholds that were more conservative. These changes reflect growing consensus around the importance of proactive management using pregnancy safe hypertension meds to prevent escalation to more severe conditions.
In parallel, research into pharmacogenomics and individualized treatment is gaining traction. Scientists are exploring how genetic variations influence drug metabolism and efficacy in pregnant women, potentially paving the way for more personalized approaches. Moreover, the integration of digital health technologies, such as remote blood pressure monitoring and telemedicine consultations, is enhancing prenatal care and medication management. These innovations are expected to improve adherence, reduce hospitalizations, and ultimately lead to better maternal and fetal outcomes.
Practical Considerations for Managing Hypertension in Pregnant Patients
Beyond selecting the right medication, managing hypertension in pregnancy involves a multidisciplinary approach that encompasses patient education, regular monitoring, and lifestyle modifications. Prenatal care providers must educate patients on the importance of adherence to prescribed pregnancy BP meds, potential side effects, and warning signs that warrant medical attention.
Blood pressure should be monitored at home when feasible, with patients instructed on proper technique and frequency. Frequent in-office visits are also necessary to evaluate treatment efficacy and detect any signs of preeclampsia or fetal compromise. Ultrasound assessments and fetal growth measurements may be scheduled more frequently for those with uncontrolled hypertension or a history of complications.
Dietary modifications, such as sodium restriction and increased potassium intake, can complement pharmacologic therapy. Light to moderate exercise, approved by a healthcare provider, may also support blood pressure control. It is crucial, however, that patients understand lifestyle changes are not a substitute for medication when pharmacologic treatment is indicated.
Open communication between the patient and healthcare team fosters a trusting relationship and ensures that concerns about medication safety are addressed promptly. A collaborative care model that includes obstetricians, maternal-fetal medicine specialists, and pharmacists can optimize outcomes and provide reassurance to patients navigating the challenges of hypertensive pregnancy.

The Role of Postpartum Monitoring and Long-Term Cardiovascular Health
While much attention is given to blood pressure management during pregnancy, the postpartum period also demands vigilant monitoring. Hypertension can persist or even worsen after delivery, especially in women who had preeclampsia or chronic hypertension. In some cases, new-onset postpartum hypertension may develop, requiring continued pharmacologic intervention.
Healthcare providers should continue to prescribe blood pressure medication for pregnant women transitioning to the postpartum period, carefully adjusting dosages to reflect the changing physiology after birth. Medications must also be compatible with breastfeeding, further narrowing the list of suitable options. Methyldopa, while safe in pregnancy, is generally avoided postpartum due to its association with depression. Labetalol and nifedipine are more commonly continued after delivery, particularly in breastfeeding mothers.
Long-term, women who experienced hypertensive disorders during pregnancy face a higher risk of cardiovascular disease, including hypertension, stroke, and heart failure later in life. As such, postpartum follow-up is not only critical for short-term recovery but also for identifying and managing future cardiovascular risk. Lifestyle counseling, regular blood pressure checks, and referral to primary care providers for long-term monitoring should be integral parts of the care continuum.
Frequently Asked Questions: Pregnancy Blood Pressure Medications
1. Can pregnancy safe hypertension meds differ based on ethnicity or genetic background?
Yes, emerging research suggests that genetic and ethnic differences can influence how individuals respond to certain pregnancy safe hypertension meds. For instance, African American women may metabolize beta-blockers and calcium channel blockers differently, leading to variations in efficacy or side effect profiles. These differences underscore the importance of personalized medicine, where pharmacogenomic insights help tailor pregnancy blood pressure medications more effectively. However, this area is still developing, and most guidelines rely on broader population studies rather than genetic-specific recommendations. If you have a family history of drug sensitivities or belong to a demographic with known variations in medication response, discuss this with your obstetrician or maternal-fetal medicine specialist.
2. What are some lesser-known side effects of pregnancy BP meds that patients should be aware of?
While the commonly discussed side effects include fatigue or dizziness, pregnancy BP meds can also influence sleep patterns, appetite, or mood in more subtle ways. For example, some women report vivid dreams or insomnia when using certain beta-blockers. Calcium channel blockers like nifedipine may occasionally lead to peripheral edema that mimics normal pregnancy swelling but is drug-induced. Even blood pressure drugs for pregnancy deemed safe can, in rare cases, alter liver enzyme levels or blood sugar control. Monitoring these parameters can help clinicians adjust dosages or switch medications early if adverse effects emerge.
3. Is there a link between blood pressure medication for pregnant women and postpartum depression?
There is growing concern that some pregnancy blood pressure medications, particularly methyldopa, may contribute to postpartum mood disturbances. While the medication itself is well-tolerated during pregnancy, its central nervous system effects have been associated with depressive symptoms in the postpartum period. This underscores the importance of re-evaluating the choice of blood pressure meds for pregnancy after delivery, especially for patients with a history of depression or anxiety. Switching to alternatives like labetalol or nifedipine post-delivery may reduce the risk of postpartum emotional distress. Mental health monitoring should be integrated into postpartum hypertension care plans.
4. Are there pregnancy safe hypertension meds that also benefit other pregnancy complications?
Interestingly, some blood pressure drugs for pregnancy have demonstrated dual benefits. For instance, labetalol may be helpful for women with both hypertension and gestational diabetes due to its limited effect on glucose metabolism. Nifedipine, commonly used as a pregnancy BP med, is also employed off-label to manage preterm labor by relaxing uterine muscles. Such multi-functional uses offer a more efficient approach to managing coexisting conditions during pregnancy. However, combining therapies should always be guided by a specialist to avoid drug interactions or unintended consequences.
5. Can natural supplements be safely used alongside prescription blood pressure meds for pregnancy?
Many women are curious about integrating natural supplements with pregnancy blood pressure medications. However, even seemingly benign supplements can interact with prescription drugs. For example, high doses of calcium or magnesium may amplify the effects of calcium channel blockers, potentially leading to hypotension. Some herbal remedies, like licorice root or hawthorn, can be dangerous in pregnancy due to their cardiovascular effects. Always consult a healthcare provider before combining supplements with pregnancy safe hypertension meds to ensure safety and efficacy.
6. What are the psychological impacts of being prescribed blood pressure medication for pregnant women?
Receiving a diagnosis of hypertension during pregnancy can cause significant emotional distress. Many women report feelings of guilt, anxiety, or failure, believing that their condition poses a threat to their baby. Being prescribed blood pressure meds for pregnancy can reinforce these fears, especially if the medication regimen is complex or associated with hospital monitoring. It is essential for clinicians to address these psychological concerns by offering clear education and reassurance. Involving mental health professionals when needed can make the management of hypertension more holistic and compassionate.
7. How do pregnancy blood pressure medications influence delivery planning?
Certain pregnancy BP meds can influence the timing and method of delivery. For instance, poorly controlled hypertension may necessitate early induction or cesarean delivery to avoid complications like placental abruption. Conversely, effective management with pregnancy safe hypertension meds allows for closer-to-term vaginal deliveries in many cases. Some medications, such as intravenous labetalol, are also used during labor to manage acute blood pressure spikes. Open communication between the obstetrician, anesthesiologist, and primary care provider ensures that both maternal and fetal safety remain top priorities during delivery planning.
8. Are there differences in how blood pressure medication for pregnant women is managed in urban vs. rural settings?
Access to care often plays a critical role in how blood pressure medication for pregnant women is prescribed and monitored. In urban areas, pregnant patients typically have access to maternal-fetal specialists, pharmacists, and high-risk clinics that support comprehensive medication management. In contrast, rural settings may rely more heavily on general practitioners with limited access to up-to-date guidelines or specialist input. This discrepancy can affect the timely adjustment of pregnancy BP meds and follow-up care. Telemedicine is beginning to close this gap, providing remote consultations that enhance care for rural populations.
9. What should women know about stopping or tapering pregnancy blood pressure medications postpartum?
Stopping pregnancy blood pressure medications after delivery requires careful planning. Some women experience normalization of blood pressure within weeks, while others develop or maintain chronic hypertension. Tapering should be done under supervision, especially if breastfeeding, as some blood pressure meds for pregnancy are not compatible with lactation. It is also important to monitor for rebound hypertension, which can be dangerous if overlooked. A gradual reduction in medication, combined with lifestyle counseling, ensures a safe transition to postpartum cardiovascular wellness.
10. How are future pregnancies influenced by the use of blood pressure drugs for pregnancy?
Using blood pressure drugs for pregnancy in one gestation may influence how hypertension is managed in future pregnancies. Women who have previously responded well to a specific pregnancy BP med are often prescribed the same medication in subsequent pregnancies, provided no complications arose. However, long-term use of certain drugs may necessitate closer monitoring of renal function or vascular health before conception. Additionally, women who needed medication in one pregnancy have a higher chance of recurrence in future pregnancies. Preconception counseling and early monitoring are essential components of planning for healthy subsequent pregnancies.
Conclusion: Choosing the Right Blood Pressure Medication for Pregnant Women—A Balancing Act of Safety, Efficacy, and Individualized Care
Selecting the most appropriate pregnancy blood pressure medications involves far more than identifying a drug that lowers blood pressure. It is a complex decision-making process that weighs maternal and fetal safety, considers the severity and timing of hypertension, and respects the individual needs and values of the pregnant patient. With a growing body of evidence supporting the use of specific pregnancy safe hypertension meds, healthcare providers can confidently tailor treatment plans that offer both protection and peace of mind.
Labetalol, nifedipine, and methyldopa remain the cornerstone of safe antihypertensive therapy during pregnancy, with decades of research backing their efficacy and tolerability. Meanwhile, increased awareness of drugs to avoid—such as ACE inhibitors and ARBs—ensures that preventable harms are minimized. As guidelines evolve and new technologies emerge, clinicians are better equipped than ever to manage hypertension in pregnancy with precision and compassion.
Ultimately, optimizing maternal cardiovascular health through the thoughtful use of pregnancy BP meds is not just about preventing complications in the short term. It is about safeguarding the lifelong well-being of two interconnected lives. By prioritizing evidence-based practice, patient education, and comprehensive follow-up care, we can uphold the highest standards of maternal medicine and contribute to healthier futures for both mothers and their children.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Drugs for treatment of very high blood pressure during pregnancy


