Understanding insulin resistance and how nutrition plays a central role in reversing or managing it is becoming increasingly important in a world where metabolic disorders are on the rise. With growing awareness around the connections between diet, blood sugar regulation, and chronic disease prevention, identifying the best diet for insulin resistance is no longer just a matter of weight loss. It is a medical necessity for millions of people seeking better metabolic health. For those affected, following a carefully structured insulin resistance diet plan can make a transformative difference. This article explores doctor-recommended dietary strategies grounded in clinical evidence, designed to naturally support blood sugar stability, hormonal balance, and long-term wellness.
You may also like: Is the Keto Diet Safe or Dangerous? What Experts Say About the Risks, Benefits, and Basics of the Ketogenic Diet
Insulin Resistance and Metabolic Dysfunction: A Silent Epidemic
Insulin resistance occurs when the body’s cells no longer respond effectively to insulin, a hormone produced by the pancreas that helps regulate blood sugar. When insulin signaling is impaired, glucose builds up in the bloodstream, setting the stage for prediabetes, type 2 diabetes, cardiovascular disease, and other serious complications. It is a condition that can develop gradually, often going unnoticed for years. People may experience subtle symptoms such as fatigue, weight gain, brain fog, or skin changes, but these are frequently attributed to aging or stress.
From a medical perspective, insulin resistance is not merely a precursor to diabetes but a central feature of a much broader metabolic imbalance. It is often associated with abdominal obesity, high triglycerides, low HDL cholesterol, and elevated blood pressure—a cluster of risk factors known collectively as metabolic syndrome. Importantly, these are not inevitable consequences of aging but largely modifiable through lifestyle, especially nutrition. This makes dietary intervention both a powerful tool and an essential therapeutic approach. Choosing the best diet for insulin resistance can help reverse the condition or significantly reduce its impact.
Why Diet Matters More Than Ever in Insulin Resistance
Food is not just fuel; it is information that communicates with our cells. Every meal has the potential to either worsen insulin resistance or improve it, depending on its composition. Diets high in refined carbohydrates, added sugars, and processed fats contribute to insulin dysregulation by promoting excessive glucose spikes, oxidative stress, and chronic inflammation. Over time, these metabolic insults damage insulin receptor pathways and exacerbate hormonal imbalances.
Conversely, a well-formulated insulin resistance diet plan emphasizes nutrient-dense, low-glycemic foods that stabilize blood sugar, promote satiety, and enhance cellular function. Such a plan does not rely on deprivation or quick fixes but focuses on sustainable, nourishing patterns of eating. Research consistently shows that individuals who adopt whole-food-based, anti-inflammatory diets experience improvements in insulin sensitivity, lipid profiles, and weight regulation. The emphasis shifts from calorie counting to hormonal healing, from restrictive dieting to metabolic resilience.

Foundational Principles of the Best Diet for Insulin Resistance
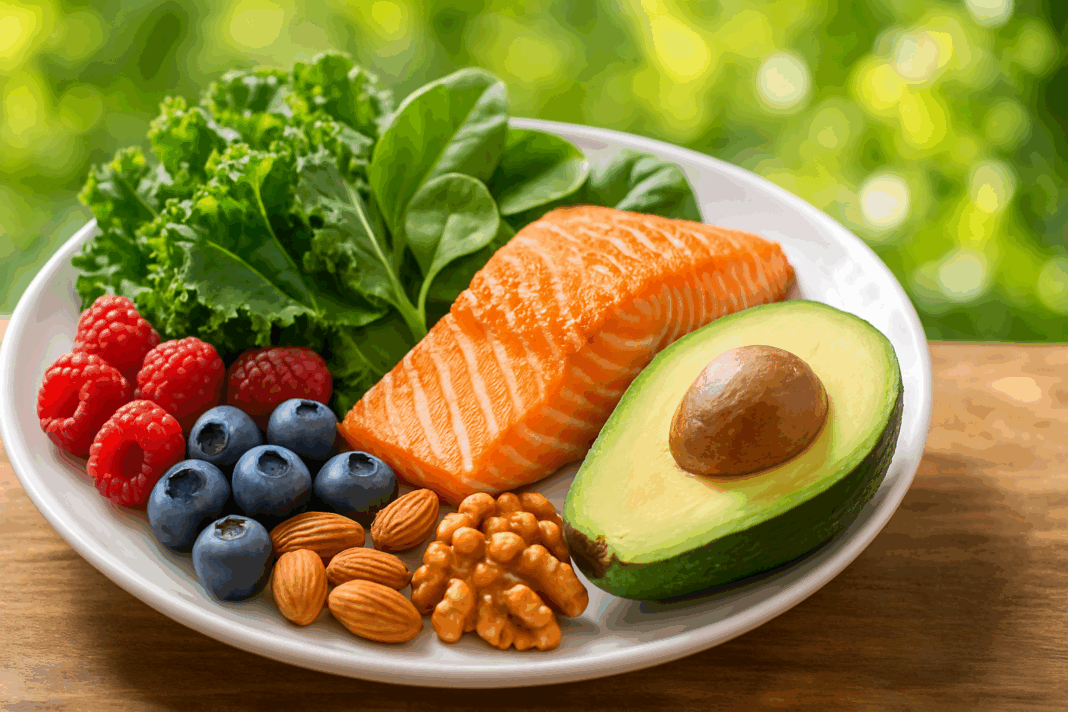
To understand what constitutes the best diet for insulin resistance, it helps to begin with several guiding principles rooted in nutritional science. First, prioritizing low-glycemic foods is essential. These include vegetables, legumes, nuts, seeds, and certain fruits that have a minimal impact on post-meal blood glucose levels. These foods provide fiber, antioxidants, and micronutrients that not only nourish the body but also reduce the glycemic burden of a meal.
Second, balancing macronutrients in every meal supports more stable energy and less insulin demand. This means including high-quality proteins, healthy fats, and complex carbohydrates in appropriate ratios. Lean proteins like poultry, eggs, fish, and plant-based options such as tofu or lentils can help build muscle and regulate hunger hormones. Healthy fats—from sources like avocados, olive oil, and fatty fish—play a crucial role in reducing inflammation and improving lipid metabolism.
Third, eliminating or minimizing refined sugars and ultra-processed foods is a non-negotiable step. These foods disrupt gut microbiota, increase inflammation, and drive insulin resistance through repeated glycemic spikes. Replacing them with whole, unprocessed alternatives is not only healthier but also more satisfying, both physiologically and psychologically. In the long term, these dietary shifts become easier to maintain because they align with the body’s natural regulatory systems.
The Role of Meal Timing and Intermittent Fasting
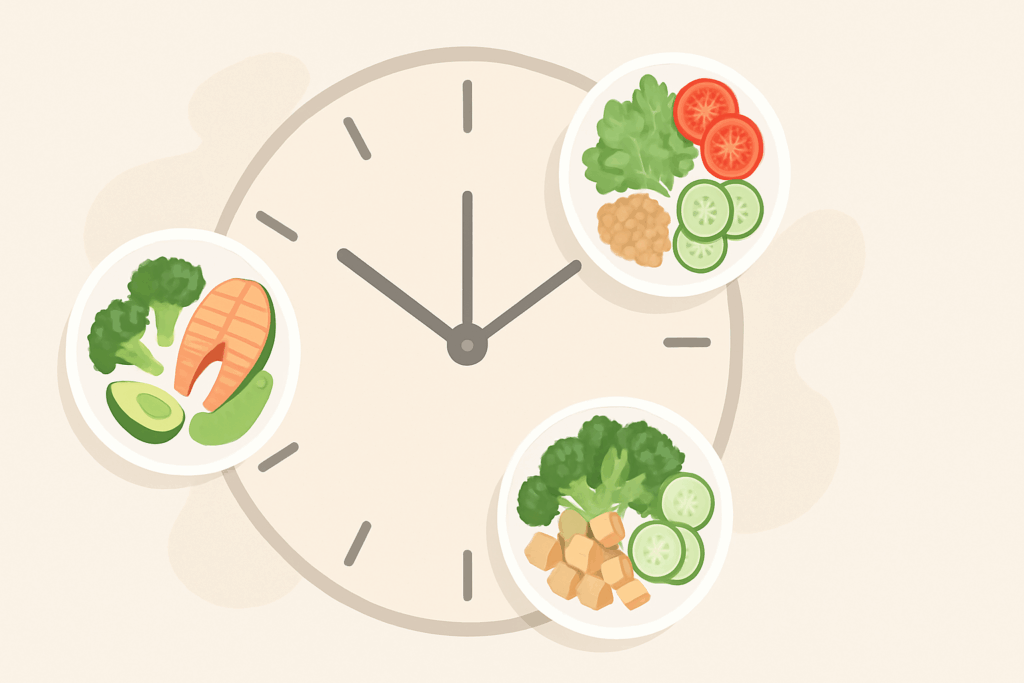
Beyond food choices, when we eat may be just as important as what we eat. Emerging evidence suggests that time-restricted eating and intermittent fasting can significantly enhance insulin sensitivity by allowing insulin levels to fall for extended periods. Unlike constant grazing, which keeps insulin elevated throughout the day, structured eating windows allow the body to enter a state of repair and metabolic reset.
One popular method involves an eating window of 8-10 hours followed by a fasting period of 14-16 hours, often referred to as 16:8 intermittent fasting. This pattern has been shown to reduce fasting insulin levels, lower triglycerides, and promote autophagy—a process by which the body clears damaged cells and improves metabolic efficiency. Importantly, intermittent fasting does not require severe caloric restriction; it simply organizes intake to align better with circadian rhythms and insulin dynamics.
For individuals following an insulin resistance diet plan, meal timing can be an empowering tool rather than a restriction. It encourages mindful eating, reduces late-night snacking, and fosters a deeper awareness of hunger cues. As always, such practices should be tailored to individual needs and medical conditions, ideally under the supervision of a healthcare provider.

Glycemic Load vs. Glycemic Index: Understanding the Distinction
While many people are familiar with the concept of the glycemic index (GI), fewer understand the value of glycemic load (GL), which provides a more accurate picture of a food’s impact on blood sugar. The GI measures how quickly a food raises blood glucose, but it does not account for portion size. Glycemic load, on the other hand, incorporates both the quality and quantity of carbohydrates, making it a more practical tool for meal planning.
For instance, watermelon has a high glycemic index but a low glycemic load due to its high water content and relatively low carbohydrate per serving. This nuance is critical when constructing a diet plan for insulin resistance, as it prevents unnecessary food avoidance and promotes a more inclusive and sustainable approach. Dietitians and endocrinologists increasingly recommend focusing on GL when counseling patients with insulin resistance, as it allows for greater flexibility and better blood sugar management.

The Power of Fiber: Soluble and Insoluble Allies
Among the most powerful yet underappreciated components of an insulin resistance diet plan is dietary fiber. Fiber not only slows the absorption of glucose, thereby reducing post-meal spikes, but it also supports gut health, reduces systemic inflammation, and enhances satiety. Soluble fiber, found in oats, flaxseeds, legumes, and certain fruits, forms a gel-like substance that moderates digestion and supports cholesterol balance. Insoluble fiber, present in whole grains and vegetables, adds bulk and facilitates regular bowel movements.
Fiber also acts as a prebiotic, feeding beneficial gut bacteria that play a role in regulating glucose metabolism. An imbalance in gut microbiota, often driven by low-fiber, high-sugar diets, has been linked to insulin resistance and systemic inflammation. Restoring microbial diversity through a high-fiber, plant-rich diet helps repair intestinal permeability and modulate immune responses.
Patients are often encouraged to aim for at least 25 to 30 grams of fiber daily, with an emphasis on variety. Incorporating a rainbow of plant foods, from leafy greens to cruciferous vegetables and berries, can make meeting fiber targets both enjoyable and nutritionally comprehensive. Moreover, increasing fiber intake gradually and with adequate hydration can help minimize gastrointestinal discomfort during the transition.
The Role of Protein in Metabolic Stability
Protein plays an indispensable role in regulating insulin sensitivity and promoting metabolic stability. Unlike carbohydrates, protein has a minimal impact on blood glucose levels and requires less insulin to metabolize. Including protein in every meal supports muscle maintenance, which is especially important given that muscle tissue is one of the primary sites of glucose disposal. A higher muscle-to-fat ratio contributes to better insulin responsiveness and long-term metabolic health.
Animal and plant-based proteins offer different but complementary benefits. While animal proteins such as fish, poultry, and eggs provide complete amino acid profiles, plant-based options like legumes, quinoa, and tempeh come with added fiber and phytochemicals. For individuals managing insulin resistance, a diverse intake of both sources ensures nutritional adequacy while supporting blood sugar regulation.
It is also worth noting that protein enhances satiety and can reduce overall caloric intake without the need for strict portion control. This aligns with a core principle of the best diet for insulin resistance: to create a pattern of eating that is sustainable, satisfying, and metabolically supportive without being overly restrictive.

The Anti-Inflammatory Advantage: Foods That Heal
Inflammation and insulin resistance are closely linked. Chronic, low-grade inflammation interferes with insulin signaling pathways and contributes to the development of metabolic disorders. Therefore, including anti-inflammatory foods in an insulin resistance diet plan is essential for long-term healing. Omega-3 fatty acids from fatty fish like salmon, sardines, and mackerel have been shown to reduce inflammation and improve insulin sensitivity. Likewise, spices such as turmeric and ginger have bioactive compounds with potent anti-inflammatory effects.
Colorful fruits and vegetables, rich in polyphenols and antioxidants, provide additional protection against oxidative stress. Berries, leafy greens, red cabbage, and pomegranate are just a few examples of foods that help neutralize free radicals and reduce metabolic damage. These foods also contribute to vascular health, which is often compromised in individuals with insulin resistance.
Olive oil, a cornerstone of the Mediterranean diet, is another valuable anti-inflammatory ally. Rich in monounsaturated fats and polyphenols, it supports healthy cholesterol levels and endothelial function. Integrating these healing foods into daily meals does not require elaborate preparation; simple combinations, such as a salad with salmon and olive oil dressing, can deliver powerful metabolic benefits with minimal effort.
Sustainability and Lifestyle Integration
The best diet for insulin resistance is not one that demands perfection but one that promotes consistency. For dietary changes to translate into long-term health gains, they must be sustainable and adaptable to individual lifestyles. This means accounting for cultural preferences, cooking skills, budget, and time constraints. A rigid plan that excludes favorite foods or requires expensive supplements is unlikely to be followed consistently.
Instead, building an insulin resistance diet plan around whole foods, seasonal produce, and minimally processed ingredients allows for flexibility and enjoyment. Cooking at home, planning meals ahead, and practicing mindful eating are practical habits that support adherence. Additionally, involving family members or a support group can increase motivation and accountability.
Lifestyle factors beyond diet, such as physical activity, sleep quality, and stress management, also influence insulin sensitivity. Regular exercise enhances glucose uptake by muscles, while restorative sleep regulates hormones that control hunger and insulin. Stress reduction techniques like yoga, meditation, or simply spending time in nature can lower cortisol levels and reduce metabolic strain. These elements, when combined with a nourishing diet, create a comprehensive approach to reversing insulin resistance.
Navigating Common Misconceptions
Despite the growing body of evidence supporting dietary intervention for insulin resistance, several misconceptions persist. One common myth is that all carbohydrates are bad. In reality, the quality and context of carbohydrate consumption matter more than blanket restriction. Whole food sources of carbs—such as legumes, vegetables, and intact grains—can be part of a balanced insulin resistance diet plan when paired with fiber and healthy fats.
Another misunderstanding is the belief that weight loss must precede improvements in insulin sensitivity. While weight reduction can enhance metabolic function, even modest dietary changes can produce measurable benefits independent of weight. Focusing solely on the scale may obscure more meaningful progress, such as improved fasting glucose or reduced triglyceride levels.
Lastly, some people assume that managing insulin resistance requires a one-size-fits-all approach. In truth, individual responses to food vary widely based on genetics, microbiome composition, and lifestyle factors. Personalization, guided by a qualified healthcare professional or registered dietitian, is key to creating a diet plan that is both effective and sustainable.
Frequently Asked Questions: Best Diet for Insulin Resistance
1. Can the best diet for insulin resistance be adapted for plant-based or vegetarian lifestyles?
Absolutely. Many people assume that managing insulin resistance requires a heavy reliance on animal-based proteins, but a well-structured plant-based version of the best diet for insulin resistance can be highly effective. Legumes, tofu, tempeh, quinoa, and nuts offer excellent protein sources while also providing the fiber that is essential for blood sugar regulation. When building an insulin resistance diet plan for vegetarians, special attention should be paid to avoiding ultra-processed meat substitutes that may be high in sodium or refined carbs. Incorporating low-glycemic vegetables, whole grains like barley and buckwheat, and anti-inflammatory herbs can ensure that a plant-based approach remains nutritionally balanced and metabolically supportive.
2. How can someone track their progress on an insulin resistance diet plan beyond just measuring weight?
Focusing solely on weight loss can be misleading, as metabolic improvements often occur even without dramatic changes on the scale. Better indicators of success on an insulin resistance diet plan include fasting insulin levels, HOMA-IR (Homeostatic Model Assessment of Insulin Resistance), and post-meal glucose trends. Some individuals also use continuous glucose monitors (CGMs) to see how specific foods impact their blood sugar, allowing for real-time adjustments to dietary choices. Improved energy levels, reduced sugar cravings, and better sleep patterns are additional qualitative signs that the best diet for insulin resistance is working. These non-scale victories are often the earliest indicators of restored metabolic function.
3. What are some lesser-known food triggers that may sabotage an insulin resistance diet plan?
While most people are aware of the risks of sugar and white flour, few realize that even “natural” health foods like agave syrup, fruit juice concentrates, and rice-based snacks can undermine an insulin resistance diet plan. These foods may carry health halos but still spike blood sugar due to their high glycemic load. In addition, emulsifiers, artificial sweeteners like aspartame, and even low-fat dairy can affect gut microbiota or stimulate insulin in ways that interfere with metabolic healing. Reading ingredient labels and avoiding foods that cause subtle inflammation or cravings is critical when following the best diet for insulin resistance. Opting for minimally processed foods is a reliable safeguard.
4. Can stress affect the results of an insulin resistance diet plan, and how can it be managed through nutrition?
Yes, stress is a significant but often overlooked factor that can disrupt even the best diet for insulin resistance. Chronic stress elevates cortisol levels, which in turn increases insulin resistance by encouraging the liver to release more glucose into the bloodstream. Including magnesium-rich foods like leafy greens, pumpkin seeds, and dark chocolate can support adrenal health and reduce stress-related metabolic strain. Adaptogenic herbs such as ashwagandha or rhodiola may also provide additional resilience, though they should be used under medical guidance. Managing stress holistically enhances the benefits of an insulin resistance diet plan by improving hormonal balance and reducing inflammatory markers.
5. Are there any advanced testing methods that can personalize the best diet for insulin resistance?
Personalized nutrition is gaining traction, and new tools are making it possible to tailor an insulin resistance diet plan more precisely. Genetic testing for polymorphisms related to insulin signaling or carbohydrate metabolism can guide macronutrient ratios. Gut microbiome analysis can reveal whether specific bacterial strains that support insulin sensitivity are present or lacking. Moreover, metabolomic profiling helps identify nutritional deficiencies or metabolic bottlenecks that may be holding back progress. These tests, though still emerging, offer the potential to fine-tune the best diet for insulin resistance beyond general guidelines and into truly individualized therapeutic plans.
6. What role do social habits and environment play in the long-term success of an insulin resistance diet plan?
Social habits and environment often determine whether someone can maintain the best diet for insulin resistance over time. Eating out frequently, having limited access to fresh produce, or living in a household with unsupportive dietary patterns can create friction with dietary goals. Creating a supportive food environment at home, learning how to navigate social gatherings mindfully, and engaging in shared meal prep can boost adherence. Peer support, whether from family or community programs, adds accountability and motivation. Recognizing these psychosocial dynamics is vital when designing an insulin resistance diet plan that can realistically be sustained in everyday life.
7. How does alcohol consumption impact the effectiveness of the best diet for insulin resistance?
Alcohol can pose a significant obstacle to metabolic recovery, even if consumed in moderation. It disrupts liver function, impairs glucose production, and often leads to poor food choices. While some studies suggest that red wine in small amounts may offer cardiovascular benefits, those with insulin resistance are generally better off minimizing or eliminating alcohol altogether. It also contributes empty calories and can interfere with sleep quality—both of which impair insulin sensitivity. If alcohol is consumed at all, it should be very limited and paired with food to reduce glycemic volatility, particularly within a carefully managed insulin resistance diet plan.
8. Can exercise compensate for a less-than-perfect insulin resistance diet plan?
Exercise is undeniably beneficial, but it cannot completely offset the effects of a poor diet. While physical activity improves glucose uptake in muscle cells and increases insulin sensitivity, dietary quality remains the cornerstone of effective management. Combining strength training and aerobic activity with the best diet for insulin resistance creates a synergistic effect that magnifies results. Relying solely on exercise without addressing dietary triggers like high-fructose corn syrup or trans fats limits long-term progress. For optimal outcomes, both nutrition and movement must work in tandem within an integrated insulin resistance diet plan.
9. What future innovations are being explored to enhance the best diet for insulin resistance?
The field of metabolic health is rapidly evolving, and future innovations promise to further refine the insulin resistance diet plan. Technologies such as AI-driven meal planning apps, precision supplementation based on micronutrient scans, and wearable biosensors will allow for real-time dietary adjustments. Research into nutrigenomics is also unveiling how individual DNA profiles influence responses to specific nutrients and food combinations. Functional foods enriched with bioactives like berberine or resistant starch may also play a more prominent role in next-generation dietary protocols. These emerging tools will help elevate the best diet for insulin resistance from reactive management to proactive optimization.
10. How can individuals prevent burnout when following an insulin resistance diet plan long term?
Diet fatigue is a real challenge, especially when dietary changes are lifelong. One way to prevent burnout is to rotate seasonal ingredients and explore new culinary techniques that align with the best diet for insulin resistance. Experimenting with global cuisines—such as Mediterranean, Thai, or Ethiopian—can keep meals exciting while staying within metabolic boundaries. Allowing for planned indulgences, using intuitive eating principles, and celebrating non-scale victories also fosters a more positive relationship with food. Most importantly, framing the insulin resistance diet plan as a journey of self-care rather than punishment can transform the experience into one of empowerment rather than restriction.
Conclusion: Supporting Metabolic Health with the Best Diet for Insulin Resistance
Addressing insulin resistance through nutrition is one of the most powerful and accessible interventions available today. The best diet for insulin resistance is not a fad or a rigid prescription but a dynamic, evidence-based strategy that emphasizes whole foods, balanced macronutrients, fiber-rich ingredients, and anti-inflammatory support. A carefully designed insulin resistance diet plan does more than control blood sugar; it restores metabolic balance, supports hormonal harmony, and fosters long-term health resilience.
By integrating time-tested principles with personalized strategies, individuals can regain control over their metabolic destiny. Whether through mindful eating, thoughtful meal composition, or lifestyle enhancements like exercise and stress reduction, every step counts. As research continues to deepen our understanding of insulin resistance, the core message remains clear: food is medicine, and healing begins on the plate.
Further Reading:
Meal Planning & Exercise Tips for Insulin Resistance
Insulin resistance and how to eat the right foods for you