Introduction: The Rising Importance of Diabetes Research in Modern Medicine
Diabetes mellitus continues to pose one of the most significant challenges to global public health in the 21st century. With the incidence of both type 1 and type 2 diabetes on the rise, medical researchers and clinicians are racing to uncover more effective strategies for early diagnosis, prevention, and long-term management. A recently published diabetes research paper has ignited renewed hope within the scientific community by highlighting revolutionary breakthroughs in early detection biomarkers and personalized therapeutic approaches. Drawing on robust findings from a peer-reviewed diabetes journal, this research study about diabetes is already influencing clinical guidelines and shaping future investigational paths.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
The urgency surrounding diabetes research cannot be overstated. More than 537 million adults globally are living with diabetes, according to the International Diabetes Federation. This number is projected to rise sharply in the coming decades, compounding the financial, emotional, and physiological burden on patients, families, and healthcare systems. As such, any significant development in diabetes res—short for diabetes research—has profound implications. This article explores in depth the core findings and broader impacts of this pivotal diabetes research paper, while reflecting on its real-world applications for clinicians, patients, and policy makers alike.
Revolutionizing Diagnosis: The Role of Biomarkers in Early Detection
One of the most groundbreaking aspects of the featured diabetes research paper is its focus on identifying novel biomarkers for earlier and more accurate detection of diabetes, even before traditional symptoms emerge. Historically, diabetes diagnosis has relied heavily on fasting glucose levels, HbA1c readings, and glucose tolerance tests. While effective to a degree, these tools often detect diabetes after considerable beta-cell damage has already occurred, limiting the effectiveness of early intervention.
Recent findings published in a leading diabetes journal illustrate how advanced proteomic and metabolomic screening techniques are uncovering previously unrecognized biomarkers that signal metabolic disruption well before glucose dysregulation becomes evident. Specifically, researchers found that elevated levels of branched-chain amino acids (BCAAs) and altered lipid metabolites may precede insulin resistance by several years. These insights pave the way for a more predictive model of diabetes diagnosis—one that allows healthcare providers to intervene during the preclinical stages of the disease.
This research study about diabetes also emphasizes the growing potential of genetic markers in refining risk assessment. By combining polygenic risk scores with metabolic data, scientists can now stratify patients by their likelihood of developing diabetes with unprecedented precision. This evolution in diabetes res reflects a paradigm shift: from reactive disease management to proactive, preventive care grounded in individualized data.
Innovations in Personalized Treatment: Moving Beyond One-Size-Fits-All
Just as the approach to diagnosis is becoming more sophisticated, so too are the treatment strategies being developed as a result of the diabetes research paper. Traditional management protocols for type 2 diabetes have largely centered around lifestyle modifications, oral hypoglycemics, and insulin therapy. However, this model often fails to account for individual variability in disease progression and treatment response.
Emerging data from the diabetes journal in question suggest a more nuanced understanding of diabetes pathophysiology. For instance, researchers identified subtypes of type 2 diabetes based on distinct phenotypic and molecular characteristics, including insulin deficiency, insulin resistance, obesity-related inflammation, and even autoimmunity. These distinctions are clinically meaningful, as they dictate which interventions are most likely to be effective for a given patient.
In practice, this translates into the potential for personalized therapeutic regimens that are tailored to a patient’s unique biological profile. This personalization may involve selecting specific drug classes—such as GLP-1 receptor agonists or SGLT2 inhibitors—based on genetic markers or metabolomic signatures. Moreover, the diabetes research paper underscores the importance of pharmacogenomics in guiding drug dosage and minimizing adverse effects, a factor that could greatly enhance treatment adherence and outcomes.
The Emerging Role of Artificial Intelligence in Diabetes Research
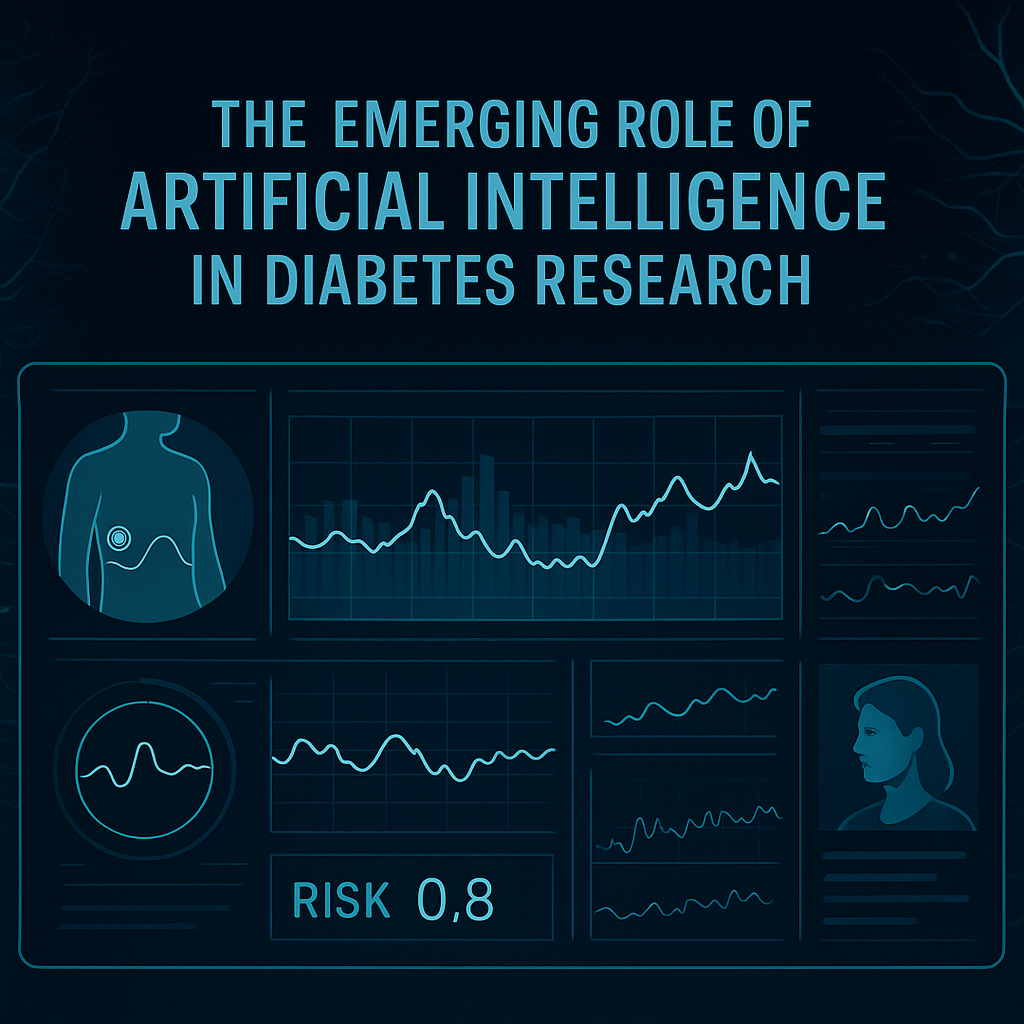
Another compelling theme that surfaces throughout this research study about diabetes is the increasing integration of artificial intelligence (AI) and machine learning into both clinical practice and research methodology. By processing vast datasets derived from electronic health records, wearables, genetic sequencing, and continuous glucose monitors, AI algorithms can identify patterns and correlations that would be impossible to detect manually.
For instance, one component of the diabetes res featured in the paper demonstrated how machine learning models could predict the onset of diabetes up to five years in advance with over 85% accuracy. These models were trained using thousands of patient profiles, integrating lifestyle, dietary, genomic, and biometric inputs to create comprehensive risk profiles. Such predictive models are already being piloted in clinical settings to guide screening and preventive strategies.
Beyond diagnosis and prediction, AI is also playing a pivotal role in the optimization of treatment plans. Personalized insulin dosing algorithms, real-time alerts for hypoglycemia, and predictive models for medication response are examples of how technology is elevating diabetes care. These AI-driven interventions, grounded in the findings of the diabetes research paper, are quickly transitioning from theoretical models to real-world tools, reflecting the rapid pace of innovation in this space.
Epigenetic Discoveries: A New Layer in Diabetes Pathogenesis
While genetic predisposition to diabetes has been well established, the current research study about diabetes delves deeper into the emerging field of epigenetics to understand how environmental factors influence gene expression without altering DNA sequences. This area of diabetes res is particularly fascinating because it helps bridge the gap between nature and nurture—between hereditary risk and lifestyle influences.
Researchers observed that patients with high exposure to early-life stress, poor nutrition, or chronic inflammation displayed distinct DNA methylation patterns in key metabolic genes. These epigenetic modifications were associated with impaired insulin signaling and increased susceptibility to glucose intolerance. Importantly, many of these changes were found to be reversible through targeted lifestyle interventions, such as improved diet and exercise.
This dimension of the diabetes research paper suggests that epigenetic profiling could become a valuable tool not only for risk assessment but also for monitoring the effectiveness of lifestyle-based therapies. It also reinforces the concept that early-life interventions—particularly in children and adolescents at risk—may have long-lasting impacts on disease prevention.
Socioeconomic Disparities and Diabetes Outcomes: A Deeper Look
A truly comprehensive diabetes research paper must consider the societal dimensions of disease burden, and this one is no exception. One particularly revealing section of the diabetes journal article explores how socioeconomic status (SES) continues to influence not only the incidence of diabetes but also the quality of care and health outcomes. Through a large-scale cohort analysis, the researchers highlighted stark disparities in access to preventive services, diabetes education, and advanced treatment options among patients from lower-income backgrounds.
The data show that individuals from socioeconomically disadvantaged populations are more likely to receive delayed diagnoses, face greater challenges adhering to treatment regimens, and experience higher rates of complications such as neuropathy, retinopathy, and kidney disease. These disparities are further compounded by environmental factors like food deserts, limited opportunities for physical activity, and lower health literacy.
Importantly, the diabetes research paper calls for policy-driven solutions, such as community health initiatives, subsidized screening programs, and broader insurance coverage for advanced diabetes therapies. These recommendations are rooted in the understanding that addressing social determinants of health is essential for reducing the overall burden of diabetes and achieving equitable care outcomes.
Implications for Clinical Practice: Bridging Research and Real-World Care
The practical implications of this research study about diabetes are far-reaching and multifaceted. From a clinical standpoint, the shift toward personalized, data-driven care will require significant updates to current protocols, provider training, and electronic health record integration. Clinicians must be equipped not only with an understanding of new biomarkers and treatment pathways but also with the tools to implement them effectively.
One promising avenue discussed in the diabetes journal article is the use of clinical decision support systems (CDSS) that integrate research findings directly into point-of-care platforms. These systems can guide physicians in choosing appropriate diagnostics, interpreting genetic data, and recommending individualized treatment plans based on up-to-date evidence. Such integration ensures that cutting-edge discoveries do not remain confined to academic journals but instead translate into tangible benefits for patients.
Moreover, the research advocates for multidisciplinary care teams—including endocrinologists, nutritionists, genetic counselors, and behavioral health specialists—to deliver truly holistic diabetes care. The emphasis on collaboration and communication reflects an evolving understanding of diabetes as not just a metabolic condition, but a complex, biopsychosocial disease requiring integrated solutions.
Future Directions in Diabetes Research: Charting the Path Ahead
While the current findings represent a significant leap forward, the diabetes research paper also highlights areas where further inquiry is urgently needed. For example, researchers call for more longitudinal studies that follow patients over decades to better understand the natural history of different diabetes subtypes and the long-term impact of personalized interventions.
There is also a growing recognition of the need for greater diversity in clinical trials. Historically, diabetes res has relied heavily on data from populations in high-income countries, often failing to capture the full spectrum of genetic, environmental, and cultural influences that shape disease expression and response to treatment. Expanding global research networks and ensuring representation from underrepresented groups will be critical to building inclusive, generalizable solutions.
Finally, the authors underscore the importance of translational research—efforts that bridge the gap between bench science and clinical application. Investing in the infrastructure, training, and incentives needed to accelerate this translation will ensure that discoveries made in the lab swiftly benefit those in clinical settings.
Frequently Asked Questions (FAQ): Breakthroughs in Diabetes Research and Clinical Implications
1. How do recent diabetes research papers influence everyday clinical practice?
While clinical practice guidelines often evolve slowly, recent diabetes research papers are accelerating that process by offering real-time insights into patient stratification, diagnostic techniques, and therapeutic options. For example, findings from a cutting-edge diabetes research paper might prompt endocrinologists to begin testing for early biomarkers or to consider pharmacogenomic testing before prescribing certain medications. These studies are not just theoretical—they’re driving the creation of clinical decision support systems (CDSS) that bring data directly to the point of care. Additionally, diabetes journals often publish implementation frameworks that guide physicians on how to translate academic insights into practical treatment protocols. The ripple effect is evident in hospital systems that increasingly integrate research-based algorithms for individualized diabetes management.
2. What role do patient-reported outcomes play in diabetes research today?
Although traditionally underutilized, patient-reported outcomes (PROs) are becoming a cornerstone of modern diabetes res. Researchers are realizing that metrics such as quality of life, treatment satisfaction, and emotional well-being offer invaluable insights into treatment effectiveness. In fact, many a recent diabetes research paper includes entire sections dedicated to PROs, especially when evaluating lifestyle interventions or newer drug classes. These subjective inputs are helping shape clinical trials that prioritize patient experience alongside biochemical endpoints. By emphasizing PROs, diabetes journals are signaling a paradigm shift toward holistic, patient-centered care in research and practice.
3. Are there geographic or cultural factors considered in current diabetes res efforts?
Yes, many recent initiatives within diabetes res are making a concerted effort to diversify participant demographics. For years, the lack of representation from low- and middle-income countries skewed global data, but this is changing. Multinational research consortia are now conducting population-specific studies to understand how ethnicity, diet, and cultural practices influence diabetes onset and progression. One diabetes journal recently featured a comprehensive research study about diabetes in sub-Saharan Africa that revealed distinct genetic markers not typically seen in Western populations. By contextualizing data within geographic and cultural frameworks, researchers can develop interventions that are both scientifically valid and culturally sensitive.
4. What makes a diabetes journal article considered high-impact in the medical community?
A high-impact diabetes journal article typically offers novel insights, robust methodology, and real-world applicability. Beyond citation counts, what elevates a paper is its ability to change practice or challenge prevailing assumptions. For instance, a groundbreaking diabetes research paper might redefine diabetes subtypes or reveal the long-term effects of a newly approved therapy. Peer-reviewed journals assess impact through reviewer feedback, citation frequency, and whether the findings influence updates in clinical guidelines. Moreover, a truly impactful research study about diabetes often triggers follow-up studies across disciplines, such as genomics, behavioral science, or public health.
5. How are mental health considerations being integrated into diabetes research studies?
The bidirectional link between mental health and diabetes is gaining more visibility in academic literature. Researchers now routinely include psychological screening tools in diabetes research paper designs to assess conditions like depression, anxiety, and diabetes distress. Some diabetes res initiatives are exploring how cognitive behavioral therapy (CBT) and mindfulness-based interventions influence glycemic control, independent of medication. These studies underscore the idea that managing diabetes isn’t solely about insulin and carbs—it’s also about emotional resilience. More importantly, several diabetes journals are advocating for integrated care models that merge endocrinology with behavioral health for comprehensive management.
6. What technological innovations are being studied for future diabetes management?
A number of diabetes research papers are now focused on emerging technologies such as digital twins, biosensors, and closed-loop insulin delivery systems. A digital twin, for example, creates a real-time, data-driven model of an individual’s metabolic profile, allowing physicians to simulate responses to different interventions before implementing them. These technologies are not science fiction; they are being evaluated in clinical settings and discussed in forward-looking diabetes journals. In addition, smart insulin pens and continuous glucose monitors are being upgraded with AI to improve predictive accuracy. These tools are gaining traction in research study about diabetes because they hold the promise of making diabetes management more precise, proactive, and personalized.
7. How does environmental exposure factor into current diabetes res findings?
Environmental triggers such as pollution, endocrine-disrupting chemicals, and even indoor air quality are emerging themes in diabetes res. Several recent diabetes research papers have examined how long-term exposure to fine particulate matter (PM2.5) increases insulin resistance, especially in urban populations. Some diabetes journals are calling for environmental health to become a standard variable in diabetes risk models. These findings are shifting how public health experts frame disease prevention, moving from solely personal responsibility to also acknowledging societal and environmental contributions. The implications are profound, especially for policymaking, urban planning, and preventive healthcare.
8. Are there any under-researched areas in diabetes studies that need more attention?
Despite substantial progress, several gaps remain. One under-explored avenue in diabetes res involves diabetes remission in type 2 patients—particularly the long-term sustainability of remission achieved through weight loss or metabolic surgery. Another area is the impact of menopause and hormonal therapy on glycemic control, which receives limited coverage despite its significance. Additionally, pediatric diabetes, especially among minority populations, remains a less-charted territory in many diabetes journals. Addressing these research voids would contribute to more inclusive, comprehensive diabetes care. Emerging research study about diabetes must take these gaps seriously if the field is to evolve equitably and effectively.
9. How is wearable technology transforming research design in diabetes studies?
Wearable tech has introduced a new layer of continuous, real-time data collection that enriches the accuracy and scope of diabetes research paper findings. Devices like smartwatches and glucose monitors not only track blood sugar but also sleep patterns, physical activity, and stress indicators. These metrics allow researchers to create more dynamic models of diabetes progression and treatment response. Moreover, several diabetes journals are beginning to publish protocols that rely heavily on wearable data, setting a precedent for future studies. In fact, some research study about diabetes now includes patient-generated health data as a primary endpoint, a major departure from traditional designs.
10. What is the future of interdisciplinary collaboration in diabetes research?
The complexity of diabetes demands collaboration across disciplines—from endocrinologists and geneticists to behavioral scientists and software engineers. Many diabetes research papers are now co-authored by experts from multiple fields, reflecting this integrative approach. Such collaboration is particularly evident in projects involving machine learning or health economics, where input from non-clinical domains is essential. Leading diabetes journals actively promote interdisciplinary special issues that explore connections between fields like epigenetics and population health. As a result, any forward-thinking research study about diabetes is increasingly characterized by its collaborative spirit, marking a decisive evolution in how the scientific community addresses chronic disease.
Conclusion: How a Single Diabetes Research Paper Is Reshaping the Future of Care
The insights presented in this breakthrough diabetes research paper are not merely academic; they represent a turning point in how the medical community approaches one of the most prevalent and impactful chronic diseases of our time. By integrating advanced diagnostics, personalized therapeutics, artificial intelligence, and socioeconomic awareness, this research offers a multidimensional framework for addressing diabetes in a more effective, equitable, and patient-centered manner.
What makes this particular study stand out in the broader field of diabetes res is its commitment to both scientific rigor and practical relevance. Drawing from extensive datasets and multidisciplinary expertise, the research study about diabetes detailed in this article sets a new standard for what is possible when innovation and implementation go hand in hand. It also illustrates how a well-executed diabetes journal publication can serve as a catalyst for systemic change—guiding policy, informing practice, and ultimately improving lives.
As we move forward, the implications of this work will continue to reverberate across healthcare systems, research institutions, and patient communities. It is a compelling reminder that behind every data point lies a person, and that the goal of diabetes research is not just to understand disease, but to prevent suffering, restore health, and inspire hope.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Promising new treatment strategy for type 2 diabetes
The future of diabetes treatment: Is a cure possible?
Emerging Breakthroughs In Diabetes Treatment: A New Era Of Hope
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.