Introduction: Unleashing the Immune System’s Hidden Warriors in the Fight Against Cancer
Cancer immunotherapy has revolutionized how we approach cancer treatment, offering hope to patients whose disease resists conventional methods like chemotherapy and radiation. Within this innovative field, tumor infiltrating lymphocytes (TILs) have emerged as one of the most promising agents in adoptive cell therapy. These immune cells naturally recognize and enter tumors, responding to abnormal proteins and attempting to destroy cancer from within.
You may also like: Cancer Research Breakthroughs: How Modern Advancements Are Transforming Treatment
Unlike generic immune cells, TIL lymphocytes are uniquely tuned to the patient’s specific tumor environment. Their therapeutic potential lies not only in their innate ability to recognize tumor antigens but also in their adaptability. While traditional immunotherapies such as checkpoint inhibitors depend on existing immune responses, TIL therapy directly delivers tumor-reactive cells to the patient, amplifying the immune attack.
The study and application of TILs are grounded in decades of rigorous research, notably pioneered by Dr. Steven Rosenberg and his team at the National Cancer Institute. Today, this approach is transforming clinical protocols, especially for patients with advanced, treatment-resistant cancers. As we explore the science behind TIL therapy, its clinical applications, and its future role in oncology, it becomes clear that tumor infiltrating lymphocytes are reshaping the immunotherapeutic landscape.
Understanding Tumor Infiltrating Lymphocytes: Nature’s Built-In Defense System
TIL lymphocytes are T cells that migrate into tumor tissue in response to the presence of cancer-specific antigens. Their presence indicates an active immune response, albeit one that is often suppressed by the tumor’s immunosuppressive microenvironment. Isolated from resected tumor tissue, these lymphocytes are expanded in the lab and reintroduced into the patient in large numbers.
What sets TILs apart is their natural specificity. Unlike engineered immune cells that must be programmed to recognize certain antigens, TILs have already proven their ability to locate cancer cells. This makes them especially valuable in targeting the heterogeneous populations of cells within a tumor, including resistant subclones.
Moreover, TIL density has prognostic value. Tumors with higher TIL infiltration, often referred to as “hot” tumors, tend to respond better to immunotherapies. Conversely, “cold” tumors, which lack immune presence, are more resistant. This distinction informs treatment strategies and reinforces the importance of fostering immune cell entry into tumors for effective therapeutic response.
The Biology of TIL Lymphocytes: Mechanisms of Action and Tumor Targeting
The function of TIL lymphocytes is centered on antigen recognition and cytotoxic response. CD8+ TILs use their T cell receptors (TCRs) to recognize tumor-specific antigens presented by MHC molecules. Upon recognition, they release perforin and granzyme enzymes that induce apoptosis in tumor cells. TILs also secrete cytokines such as IFN-γ and IL-2, creating an inflammatory environment that recruits and activates other immune cells.
Tumors, however, often develop mechanisms to evade TIL-mediated attack. These include upregulating PD-L1 to inhibit T cell function, secreting immunosuppressive molecules like TGF-β, and developing physical barriers that restrict immune cell access. Therefore, TIL therapy often involves lymphodepleting chemotherapy to suppress regulatory T cells and improve the effectiveness of the infused TILs.
Recent studies have identified specific TIL subtypes, such as stem-like and tissue-resident memory T cells, which demonstrate enhanced proliferation and durability. Selecting and expanding these potent TIL subsets is now an important focus in clinical manufacturing protocols, aimed at improving patient outcomes and long-term remission rates.
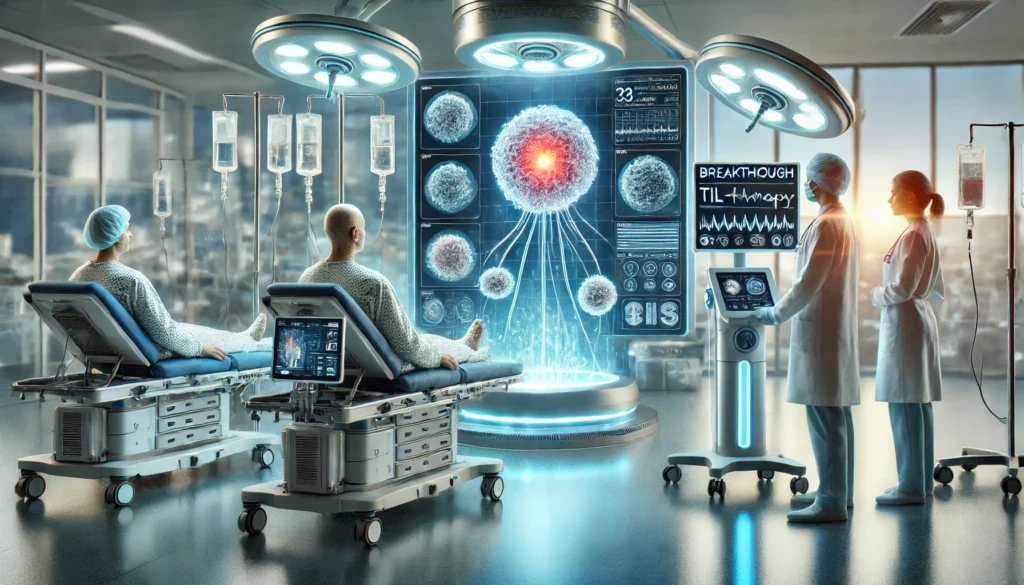
TIL Therapy in Clinical Practice: How It Works from Tumor to Treatment
TIL therapy is a highly individualized process. It begins with the surgical removal of tumor tissue from the patient. From this sample, TILs are extracted and expanded in the laboratory using high concentrations of IL-2. This expansion process can take two to three weeks, producing billions of tumor-reactive cells.
Before infusion, patients receive lymphodepleting chemotherapy, typically a combination of cyclophosphamide and fludarabine. This clears space in the immune system for the incoming TILs and reduces suppressive factors. The TILs are then infused intravenously, followed by additional IL-2 administration to support their activation and survival.
Clinical trials, particularly in metastatic melanoma, have shown response rates of 40–50%, with some patients achieving durable complete remission. These results are especially impressive in patients who have failed multiple prior treatments. As experience with TIL therapy grows, it is being increasingly adapted for other cancer types beyond melanoma.
Expanding Applications Beyond Melanoma: TIL Therapy for Multiple Cancer Types
Although originally developed for melanoma, TIL therapy is now being explored in a variety of solid tumors, including cervical cancer, non-small cell lung cancer (NSCLC), ovarian cancer, and head and neck cancers. These malignancies differ in their immunogenicity and tumor microenvironment, but TIL lymphocytes have demonstrated promising early results in several of them.
Cervical cancer, often linked to HPV, presents viral antigens that can be targeted effectively by TILs. Trials have shown objective response rates exceeding 40% in some patients. Similarly, NSCLC has a high mutational burden, providing a rich source of neoantigens that TILs can recognize.
Even in tumors considered “cold,” strategies are emerging to convert the microenvironment into one more amenable to TIL activity. These include combining TIL therapy with checkpoint inhibitors, radiation, or drugs that modify tumor immunogenicity. As data continues to accumulate, it is increasingly clear that TIL therapy may have a much broader clinical application than previously thought.
Comparing TIL Therapy to CAR-T and Checkpoint Inhibitors: Strengths and Limitations
While all forms of immunotherapy aim to empower the immune system, TIL therapy has unique advantages compared to CAR-T cells and checkpoint inhibitors. CAR-T therapy is highly effective in blood cancers but has struggled in solid tumors due to antigen heterogeneity and physical barriers. Checkpoint inhibitors work best in tumors with preexisting immune infiltration but are ineffective in patients with immune-excluded tumors.
TIL lymphocytes offer a middle ground. Because they are derived from the tumor itself, they target a wide range of antigens and can adapt to tumor heterogeneity. However, their use is limited by the need for viable tumor tissue, complex manufacturing, and the toxicity associated with IL-2 therapy.
Combining TIL therapy with other immunotherapies may amplify benefits. For example, using checkpoint inhibitors alongside TIL infusion can overcome tumor-induced immunosuppression, improving TIL persistence and function. Such synergistic approaches are becoming a focal point of ongoing trials.
Challenges and Limitations: Biological, Technical, and Logistical Hurdles
Despite its promise, TIL therapy faces several challenges. One is the variability in TIL quantity and quality between patients. Not all tumors yield sufficient or functional TILs, and the expansion process is time-consuming and costly.
Logistical issues also limit widespread access. TIL therapy is currently offered at only a few specialized centers due to the need for advanced cell processing facilities. Additionally, IL-2 administration can cause severe side effects, necessitating inpatient care and specialized monitoring.
Regulatory and reimbursement issues add further complexity. TILs are classified as advanced therapy medicinal products (ATMPs), subject to strict quality control. The high cost of production raises questions about scalability and access, especially in resource-limited settings.
Future Directions: Innovations in TIL Therapy and What Lies Ahead
Research is now focused on improving the potency, durability, and accessibility of TIL therapy. One strategy involves preselecting TIL populations with the most potent tumor-killing abilities. Another is modifying TILs genetically to resist tumor-induced suppression or to express additional immune-boosting factors.
Artificial intelligence is being used to identify biomarkers that predict response to TIL therapy. This may improve patient selection and personalize treatment. Additionally, efforts are underway to automate TIL manufacturing, potentially reducing costs and expanding access.
Combination therapies remain a major focus. Trials are testing TILs alongside PD-1 inhibitors, cytokines like IL-15, and targeted therapies to enhance efficacy. As these innovations mature, TIL lymphocytes may become a cornerstone of multimodal cancer immunotherapy strategies.
Frequently Asked Questions (FAQ): Tumor Infiltrating Lymphocytes (TIL Lymphocytes) and Cancer Immunotherapy
1. How do researchers determine which tumor infiltrating lymphocytes are most effective against cancer cells?
Scientists use sophisticated techniques such as single-cell sequencing, flow cytometry, and T cell receptor (TCR) profiling to identify which tumor infiltrating lymphocytes demonstrate the strongest reactivity against tumor-specific antigens. By analyzing gene expression patterns and cytokine profiles, they can select TIL lymphocytes with high cytotoxic potential and long-term survival characteristics. One emerging method is the identification of TILs that express markers associated with “stem-like” or memory phenotypes, which tend to be more robust and persistent after infusion. Researchers are also increasingly using artificial intelligence to predict TIL functionality based on tumor microenvironment characteristics. This level of precision ensures that only the most effective TIL lymphocytes are selected and expanded for therapeutic use.
2. Can tumor infiltrating lymphocyte therapy be combined with other emerging immunotherapies for better outcomes?
Yes, combination therapy is rapidly becoming a key focus in TIL lymphocyte research. Many studies are exploring how checkpoint inhibitors, such as PD-1 and CTLA-4 blockers, can synergize with TIL infusions by preventing immune suppression within the tumor. In addition, oncolytic viruses are being tested to precondition tumors and attract more TIL lymphocytes to the site. Cancer vaccines that prime the immune system to recognize neoantigens can also enhance the effectiveness of TIL therapy. These integrative approaches are showing promising results in early-phase trials and could redefine how we sequence and combine immune-based cancer treatments in the near future.
3. What makes TIL lymphocytes especially promising for cancers with high mutational burden?
Cancers with a high mutational burden, such as melanoma, non-small cell lung cancer, and some colorectal cancers, produce a broad array of neoantigens—mutated proteins not found in healthy tissue. This antigenic diversity creates more opportunities for tumor infiltrating lymphocytes to recognize and target malignant cells. TIL lymphocytes collected from such tumors often display high specificity to unique mutations, reducing the risk of attacking healthy cells. Furthermore, their adaptability allows them to address multiple tumor subclones simultaneously, a crucial advantage in cancers with genetic heterogeneity. This intrinsic versatility is part of what makes TIL therapy such a powerful and personalized approach for these types of malignancies.
4. Are there psychological or emotional factors patients should consider before undergoing TIL therapy?
Absolutely. Undergoing TIL therapy involves a complex and intensive process, including tumor surgery, lymphodepleting chemotherapy, and potential inpatient recovery from IL-2 side effects. Patients may experience anxiety about the physical toll, the experimental nature of the treatment, or the uncertainty of outcomes. Support systems—both psychological and social—are crucial during this time. Oncology psychologists often recommend cognitive-behavioral therapy or mindfulness-based stress reduction for patients anticipating TIL lymphocyte therapy. Discussing expectations and mental preparedness with a multidisciplinary care team can significantly enhance a patient’s resilience and treatment experience.
5. How might advances in gene editing affect the future use of tumor infiltrating lymphocytes in therapy?
The intersection of gene editing technologies, such as CRISPR/Cas9, with tumor infiltrating lymphocyte therapy is an exciting frontier in immuno-oncology. Scientists are now experimenting with genetically enhancing TIL lymphocytes to improve their persistence, metabolic fitness, and resistance to immunosuppressive signals in the tumor microenvironment. For example, knocking out PD-1 expression in TILs may prevent them from becoming “exhausted” upon entering the tumor. Other modifications may enhance their ability to traffic to tumors or survive longer in circulation. These engineered TILs represent a new generation of “supercharged” immune cells, potentially increasing the efficacy and durability of treatment across many cancer types.
6. What are some of the socioeconomic barriers limiting access to TIL lymphocyte therapy today?
While the science behind TIL therapy is advancing rapidly, socioeconomic challenges remain. The therapy is currently available only at select academic or research institutions with access to GMP (Good Manufacturing Practice)-compliant cell processing facilities. Many patients must travel long distances and may face significant out-of-pocket expenses for lodging, transportation, or even elements of the treatment itself. Additionally, insurance reimbursement for tumor infiltrating lymphocytes is still in flux, as regulatory bodies have yet to establish standardized billing codes. Efforts to decentralize TIL production and implement payer support programs are underway, but broader access will depend on addressing these deeply rooted healthcare disparities.
7. Can TIL lymphocytes be used to treat rare or pediatric cancers?
Although most current research focuses on adult cancers with high mutational loads, there is growing interest in exploring TIL lymphocyte therapy for pediatric and rare cancers. Challenges include the smaller tumor sizes in pediatric cases, which may limit the amount of viable TILs that can be extracted, and the less mutagenic nature of some childhood cancers. However, advances in TIL culture techniques and the identification of non-mutational tumor antigens could make these therapies feasible for young patients. Pediatric trials are already being developed for sarcomas and brain tumors, and early preclinical data are encouraging. Long-term safety will remain a key concern, particularly in growing children, but the future is cautiously optimistic.
8. How do tumor infiltrating lymphocytes behave differently in immunologically “cold” tumors?
In immunologically “cold” tumors, TIL lymphocytes often struggle to infiltrate or activate due to the presence of physical barriers and suppressive signaling molecules. These tumors typically lack strong antigenic stimuli or may actively repel immune cells using factors such as TGF-β or dense extracellular matrix proteins. When TILs are reintroduced via infusion, they may not survive long enough or receive the necessary co-stimulation to exert their full cytotoxic effect. Researchers are working to “heat up” these tumors through combination therapies like radiation, epigenetic modulators, or bispecific antibodies. The goal is to condition the tumor environment so that TIL lymphocytes can persist and function at full strength.
9. What are the long-term follow-up considerations after receiving TIL therapy?
Patients who undergo TIL lymphocyte therapy require comprehensive follow-up to monitor immune reconstitution, late toxicities, and disease response. Immune profiling is often conducted periodically to evaluate the persistence of infused TILs in circulation and their clonal expansion over time. Physicians also assess organ function, particularly in the kidneys, heart, and lungs, due to the potential cumulative impact of IL-2 and chemotherapy. Psychosocial support is essential, as survivors often face anxiety about recurrence or side effects. Some patients may enter long-term remission with no further therapy, while others might need maintenance treatments, especially if minimal residual disease is detected via advanced imaging or molecular diagnostics.
10. What are researchers doing to make TIL therapy more scalable and accessible in the coming years?
To broaden the impact of tumor infiltrating lymphocyte therapy, several innovations are in development. Automated bioreactor systems are being designed to standardize and accelerate TIL expansion, reducing manufacturing times and costs. Academic consortia are working to share GMP infrastructure and training across centers, allowing more facilities to offer TIL therapy. Meanwhile, companies are developing off-the-shelf TIL-based products for common tumor antigens, although these face challenges with antigen variability. Artificial intelligence is also being integrated into the TIL selection process to streamline cell profiling and match patients more efficiently with appropriate therapies. Together, these advancements aim to transition TIL lymphocytes from niche applications into broader clinical practice.

Conclusion: Why Tumor Infiltrating Lymphocytes Represent a Turning Point in Immunotherapy
TIL lymphocytes represent more than just another immunotherapy—they embody a shift toward deeply personalized, adaptive cancer care. By leveraging the body’s own tumor-targeted immune cells, TIL therapy offers a sophisticated and potentially curative approach for patients with difficult-to-treat cancers. As clinical trials expand, manufacturing processes improve, and combination therapies evolve, tumor infiltrating lymphocytes are poised to play a central role in the next generation of cancer treatment.
With continued innovation and investment, TIL lymphocytes could redefine the boundaries of what is possible in oncology, delivering hope to patients once considered untreatable. Their story is one of scientific perseverance, clinical excellence, and the promise of immune-based precision medicine at its finest.
adoptive cell therapy, immune cell therapy for cancer, personalized cancer treatment, T cell cancer therapy, immunotherapy clinical trials, solid tumor immunotherapy, cancer fighting white blood cells, advanced oncology treatments, tumor-specific T cells, cell-based cancer therapies, immune system and cancer, next-generation cancer immunotherapy, lymphocyte-based therapy, cancer microenvironment research, innovative melanoma treatment, immune checkpoint resistance, tumor neoantigen targeting, precision oncology approaches, biologic cancer treatments, immunotherapy research breakthroughs
Further Reading:
Tumor-Infiltrating Lymphocyte Therapy: A New Frontier
Tumor-Infiltrating Lymphocyte Therapy in Melanoma: Facts to the Future
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.