A New Era in Diabetes Management: The Promise of Non-Invasive Technology
For the more than 500 million people worldwide living with diabetes, the daily ritual of pricking fingers and testing blood sugar levels has long been an accepted—though burdensome—part of managing the disease. Traditional blood glucose monitoring, while effective, is inherently invasive and often uncomfortable. But thanks to advances in biomedical engineering and photonics, a new generation of tools is emerging that may offer a radically different future: laser-based non-invasive glucose monitors. Among these innovations, the laser glucose monitor stands out for its potential to transform the landscape of diabetes care.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
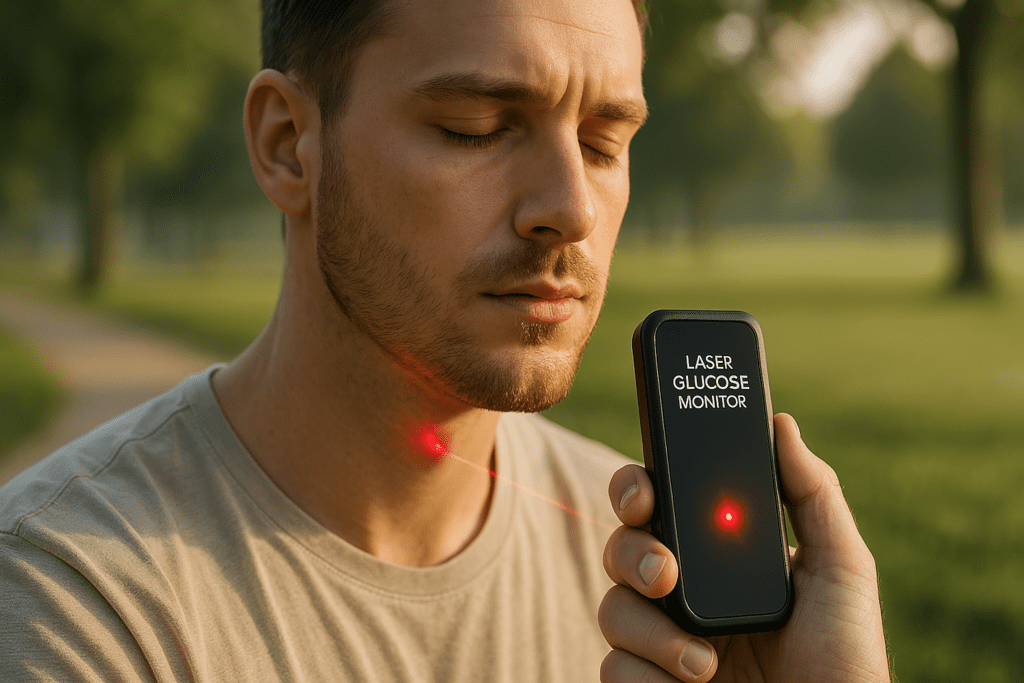
The shift toward non-invasive monitoring isn’t just about convenience. It’s about safety, adherence, and better health outcomes. People with diabetes who experience frequent finger-pricking often reduce their testing frequency, leading to inconsistent data and poor glycemic control. A laser blood sugar monitor eliminates this physical barrier, promising not just a smoother experience, but potentially a more accurate and consistent one. By integrating laser optics and spectroscopy, these devices aim to detect blood glucose levels through the skin without a single drop of blood.
Understanding How Laser Glucose Monitoring Works
At the heart of this emerging technology is a simple but powerful idea: using light to detect the chemical makeup of blood. Laser glucose monitors operate by emitting a low-energy, near-infrared laser beam that penetrates the skin to interact with interstitial fluid or blood vessels just below the surface. The light is absorbed differently depending on the glucose concentration present, and this variation is analyzed through a process known as Raman spectroscopy or mid-infrared absorption spectroscopy.
This process requires a precise calibration algorithm and signal processing capabilities to differentiate glucose signals from the myriad other substances found in the blood and skin. Despite the complexity, the outcome is promising. The technology can offer real-time readings, continuous glucose tracking, and integration with smart health platforms for data analysis and clinical oversight. Unlike previous non-invasive attempts, which often failed due to poor accuracy or impractical designs, today’s laser glucometer models are pushing closer to FDA approval and clinical readiness.
It is important to note that not all laser glucose monitors are the same. Some employ variations in light wavelength and energy levels to improve penetration and accuracy. Others, such as the D Base glucose monitor, aim to combine laser analysis with machine learning to refine results based on user-specific biomarkers. The interplay between biomedical data, wearable technology, and AI is ushering in a new paradigm in diabetes monitoring.
From Concept to Clinical Application: The Research Behind Laser Diabetes Testers
The scientific foundation for laser diabetes testers is not new, but only recently has the technology advanced enough to make it viable for real-world use. Research dating back decades attempted to explore non-invasive glucose detection using light-based methods, but early models were plagued by noise, lack of specificity, and the inability to account for skin variability across individuals.
Recent breakthroughs have overcome many of these limitations. Improvements in photodetector sensitivity, signal amplification, and wearable form factors have enabled the creation of more practical prototypes. Studies published in leading journals, including Diabetes Technology & Therapeutics and Biomedical Optics Express, have shown encouraging accuracy rates—sometimes within 10-15% of traditional finger-stick methods.
Notably, clinical trials for emerging products like the laser glucometer and D Base glucose monitor have reported promising outcomes. In one study, participants using a prototype laser blood sugar monitor were able to maintain glycemic control with fewer calibration events and greater comfort. This not only points to potential improvements in quality of life but also hints at long-term cost savings for healthcare systems burdened by complications from poorly managed diabetes.
Researchers are now focusing on refining the algorithms that power these devices, using larger and more diverse data sets to train machine learning models that can adjust for individual differences. The integration of cloud-based storage and physician access portals also means these tools are poised to play a significant role in the evolution of personalized medicine.
Benefits Beyond Comfort: Why Non-Invasive Monitoring Matters
It is tempting to view non-invasive monitoring purely through the lens of convenience, but its implications reach far deeper. Diabetes is a chronic condition that demands vigilance, and anything that reduces the barriers to consistent monitoring is inherently a health intervention. With tools like a laser glucose monitor, patients are more likely to engage in frequent tracking, detect early signs of dysglycemia, and make timely adjustments to diet, activity, or medication.
There is also the psychological benefit to consider. Finger-pricking, especially for children or those with needle phobia, can create anxiety that leads to avoidance behavior. A laser diabetes tester sidesteps this challenge, offering a painless, less intimidating alternative that supports emotional well-being alongside physical health. The user-friendly design of many modern laser blood sugar monitors also makes them attractive for elderly patients who may struggle with dexterity or vision issues.
Moreover, from a public health perspective, increasing adherence to glucose monitoring has downstream effects on healthcare utilization. When patients are better informed and proactive, they are less likely to experience emergency complications like diabetic ketoacidosis or severe hypoglycemia. This makes the case for broader insurance coverage and healthcare policy support for non-invasive options stronger than ever.
Exploring the D Base Glucose Monitor: Smart Integration Meets Optical Precision
Among the notable innovations in the field, the D Base glucose monitor represents a sophisticated merging of hardware and software. This device uses a finely tuned laser system combined with data analytics platforms that interpret light absorption patterns in real time. What sets it apart is its adaptability: it personalizes readings over time by learning from user habits, dietary intake, and activity levels, thereby increasing accuracy with continued use.
This iterative model stands in contrast to traditional glucometers, which treat each reading as isolated. By incorporating a machine-learning engine, the D Base glucose monitor can predict glucose trends and offer decision-support prompts for users. For example, it may alert the wearer to impending hyperglycemia after identifying a pattern tied to post-meal spikes. These insights are not only empowering but also actionable.
In clinical trials, early adopters reported high levels of satisfaction and ease of use. The device is designed to integrate seamlessly with smartphones and wearables, allowing users to track trends visually, share data with healthcare providers, and receive reminders for medication or activity. This convergence of laser precision and digital health intelligence exemplifies the direction in which diabetes care is moving.

Addressing Challenges: Accuracy, Regulation, and Accessibility
Despite the enthusiasm, there are still hurdles to overcome before laser-based glucose monitoring becomes standard practice. One of the primary concerns remains accuracy. While the gap between non-invasive and invasive methods is narrowing, even a small margin of error can be clinically significant, especially for insulin-dependent individuals who rely on precise data to adjust dosages.
To meet FDA requirements, developers must conduct large-scale, diverse clinical trials to validate both short-term performance and long-term reliability. Variations in skin tone, thickness, hydration levels, and environmental conditions can all affect light-based readings. Ensuring these devices work effectively across all populations is a top priority for researchers and regulators alike.
Cost is another barrier. Early iterations of laser glucometer technology may be priced higher than conventional alternatives. However, as with many medical devices, economies of scale and broader adoption can bring prices down over time. Policymakers and insurers will need to assess the long-term cost-benefit analysis, especially considering potential reductions in diabetes-related complications and hospitalizations.
Finally, education and training will be key. Both patients and healthcare providers must understand how to use, interpret, and trust the data from these new tools. As non-invasive monitoring enters the mainstream, clinical guidelines will need to evolve accordingly.
The Global Race Toward Non-Invasive Glucose Monitoring
Innovation in this space is not confined to a single country or company. Across the globe, startups, research institutions, and tech giants are investing heavily in laser glucose monitor technology. In South Korea, researchers are exploring new wavelength combinations to improve signal clarity. In the United States, companies are working with the National Institutes of Health (NIH) to conduct expansive clinical trials. Meanwhile, European firms are integrating laser sensors into smartwatches, hoping to create multi-function health devices.
The race is on not just to develop the first FDA-approved laser diabetes tester but to create the most reliable, user-friendly, and scalable solution. Competition is fostering innovation, but also necessitating collaboration. Public-private partnerships and international research consortia are becoming more common, as stakeholders recognize the complexity and potential of this challenge.
As countries grapple with rising diabetes rates and aging populations, the pressure to develop sustainable, user-centered solutions has intensified. Non-invasive tools like the laser blood sugar monitor represent not just a technological breakthrough, but a public health imperative.
Ethical and Privacy Considerations in the Age of Smart Monitoring
As with any technology that collects personal health data, the rise of laser glucose monitors raises important questions about privacy and ethics. Continuous glucose monitoring devices often sync with cloud-based platforms, enabling remote tracking by healthcare teams or family members. While this can enhance safety—particularly for children or elderly individuals—it also introduces risks related to data breaches, misuse, and consent.
Manufacturers must prioritize cybersecurity protocols, from encryption to anonymization of sensitive information. Transparency is equally vital. Users should understand what data is being collected, how it will be used, and who has access to it. Regulatory bodies may need to expand current medical device frameworks to include specific guidelines for data governance in smart diabetes tools.
There is also the issue of equity. If advanced monitoring tools like the D Base glucose monitor are only accessible to wealthier patients or those in urban centers, existing disparities in diabetes care could widen. Developers and policymakers must work together to ensure these breakthroughs do not become luxury options but are equitably distributed across socioeconomic and geographic lines.
Looking Forward: A Paradigm Shift in Diabetes Care
The path toward mainstream adoption of laser-based glucose monitoring may still have obstacles, but the momentum is undeniable. As more devices enter clinical testing and edge closer to regulatory approval, the vision of a painless, accurate, and user-friendly blood sugar monitoring system is fast becoming reality.
It is likely that within the next five to ten years, tools like the laser glucose monitor and D Base glucose monitor will become common in diabetes clinics and homes alike. As machine learning continues to evolve, these tools will not only track glucose but anticipate needs, adjust algorithms in real-time, and support holistic disease management. The integration of wearable laser glucometers into broader digital health ecosystems may also enable earlier detection of prediabetes and metabolic syndrome, opening new avenues for prevention.
By shifting the focus from reactive to proactive care, laser diabetes testers have the potential to redefine what it means to live with diabetes. Patients will have greater autonomy, providers will have richer data, and public health systems will benefit from reduced costs and complications.

Frequently Asked Questions (FAQ): Laser-Based Non-Invasive Glucose Monitoring
1. How do environmental conditions affect the accuracy of a laser glucose monitor?
While laser glucose monitors are designed for reliability, environmental factors such as temperature, humidity, and light exposure can subtly influence their readings. For instance, excessive perspiration or extreme cold may interfere with light absorption or skin reflectivity, requiring compensation algorithms to maintain precision. Modern devices like the laser glucometer often include temperature sensors and dynamic calibration to address these variables in real-time. Additionally, the location of use—indoors versus outdoors—may impact device performance due to changes in ambient light, especially for models using mid-infrared wavelengths. As the technology continues to evolve, next-generation laser glucose monitors are expected to incorporate adaptive optics and AI-enhanced correction protocols to further stabilize readings across a wide range of conditions.
2. Can laser blood sugar monitors support early diabetes detection in at-risk populations?
Yes, laser blood sugar monitors have the potential to play a significant role in proactive screening, particularly for those at high risk of developing diabetes. By offering painless and frequent testing, these tools encourage users to monitor fluctuations in glucose metabolism long before clinical symptoms manifest. Over time, patterns such as elevated postprandial spikes or irregular fasting glucose levels can prompt early interventions, including lifestyle changes or medication. Devices like the D Base glucose monitor, which integrate longitudinal data analysis, could one day be programmed to flag prediabetes markers and notify users to consult their healthcare providers. While not a replacement for diagnostic blood work, the laser diabetes tester may soon become a key tool in early detection protocols and population health strategies.
3. How does the user experience of a laser glucometer differ from traditional glucose monitors?
The user experience of a laser glucometer differs dramatically from that of conventional meters. With no lancets, test strips, or manual sampling required, users are spared both the discomfort and inconvenience of finger-pricking. Many laser glucose monitor models are designed as wearable devices or handheld scanners that deliver near-instantaneous readings with a single scan. Additionally, features such as automatic data logging, smartphone syncing, and trend visualization make them more intuitive and integrated with daily life. Unlike traditional systems that often require separate logging or manual data entry, devices like the D Base glucose monitor simplify glucose management through seamless, real-time feedback loops.
4. Are there any known long-term skin effects from using a laser diabetes tester?
To date, research has not identified any significant long-term skin complications from the routine use of a laser diabetes tester. The energy levels employed in these devices are carefully calibrated to remain within safe exposure thresholds for human skin. However, repeated use in the same location may occasionally cause mild irritation or temporary redness, particularly in individuals with sensitive skin or dermatologic conditions. Some models, including newer versions of the laser blood sugar monitor, recommend rotating scan sites to minimize any potential effects. As the field advances, manufacturers are exploring even softer wavelengths and improved ergonomics to ensure maximum comfort and minimal dermal impact over time.
5. How does machine learning enhance the accuracy of a laser glucose monitor?
Machine learning adds a powerful layer of precision to laser glucose monitor systems by enabling them to adapt to individual users over time. These algorithms analyze how a person’s body responds to meals, exercise, medications, and circadian rhythms, refining calibration to account for these fluctuations. In the case of the D Base glucose monitor, continuous learning allows it to build a unique metabolic profile for each user, making future readings more accurate and contextually meaningful. Machine learning also supports anomaly detection—flagging irregular data patterns that might indicate sensor misalignment or biological irregularities. As these systems collect more data, they can even begin to offer predictive alerts, helping users prevent highs and lows before they occur.
6. What makes the D Base glucose monitor different from other laser glucometer devices?
The D Base glucose monitor distinguishes itself through its emphasis on individualized insight and AI integration. Unlike basic laser glucometer models that simply provide one-time readings, the D Base system interprets longitudinal data and offers tailored feedback. Its algorithm adapts in real time, learning from users’ lifestyle habits, meal timing, and exercise routines to offer context-sensitive alerts and suggestions. The device also interfaces with broader health ecosystems, allowing for integration with electronic medical records and physician dashboards. In essence, while both the D Base glucose monitor and traditional laser glucose monitors share core optical technology, the D Base offers a more comprehensive and intelligent user experience.
7. Could laser blood sugar monitors be used in pediatric care or for people with disabilities?
Absolutely. One of the most promising aspects of the laser blood sugar monitor is its suitability for populations that traditionally struggle with invasive testing, including children and individuals with disabilities. Children often fear needle-based glucose checks, which can lead to avoidance and inadequate monitoring. A laser diabetes tester removes that barrier, making regular testing painless and child-friendly. Likewise, individuals with limited dexterity, vision impairment, or cognitive challenges may benefit from the simplicity and automation provided by devices like the laser glucometer. As manufacturers continue to refine user interfaces and accessibility features, these monitors are likely to become critical tools in inclusive, patient-centered diabetes care.
8. What are the global implications of adopting laser glucose monitors in low-resource settings?
Incorporating laser glucose monitors into low-resource environments could radically shift global diabetes care. Traditional supplies such as test strips and lancets create recurring costs and logistical challenges in underserved regions. A reusable, calibration-stable laser glucometer could lower long-term expenses and improve access to reliable glucose data. However, challenges remain, including initial device cost, the need for mobile infrastructure, and training for both patients and providers. Nevertheless, pilot programs using simplified laser diabetes tester models are already underway in parts of Asia and Africa, showing that with the right implementation strategy, this technology could bridge the diabetes care gap globally.
9. How secure is the personal health data collected by laser glucometer devices?
Security is a top concern as laser glucometer devices become increasingly connected to cloud-based systems and mobile applications. Reputable manufacturers now embed robust encryption protocols to protect transmitted data, ensuring that glucose readings, personal information, and medical histories remain private. Devices like the D Base glucose monitor often include biometric or multi-factor authentication for added security. Furthermore, regulatory bodies in regions like the EU and U.S. are beginning to require compliance with standards such as GDPR and HIPAA for digital medical devices. While no system is entirely immune to cyber threats, the latest generation of laser glucose monitors prioritizes data integrity alongside clinical accuracy.
10. What role could laser diabetes testers play in the future of preventive medicine?
Laser diabetes testers could become powerful tools in shifting the medical model from reactive to preventive care. By enabling painless, frequent, and real-time tracking of blood sugar levels, they facilitate better behavioral feedback loops and earlier detection of trends that precede full-blown disease. In combination with wearables that monitor physical activity, sleep, and stress, a laser blood sugar monitor could provide a holistic view of metabolic health. Forward-thinking clinicians are already exploring how continuous data from these devices can support personalized coaching, nutritional counseling, and early intervention protocols. As predictive analytics improve, the laser glucometer may evolve from a glucose tracker into a comprehensive wellness platform that helps users maintain long-term metabolic resilience.
Conclusion: Embracing Innovation with the Laser Glucose Monitor for a Healthier Future
As the global burden of diabetes continues to rise, the urgency for better tools becomes more acute. Laser-based monitoring technologies are answering this call with sophistication, precision, and empathy. The laser glucometer is not merely a gadget; it represents a meaningful evolution in how we approach chronic disease management. With devices like the D Base glucose monitor offering personalized, non-invasive, and smart tracking capabilities, the future of diabetes care looks not only more advanced but more humane.
The continued development and equitable deployment of laser blood sugar monitors will require interdisciplinary collaboration, regulatory vigilance, and patient-centered design. Yet the reward is well worth the effort: a future where managing diabetes no longer means pain, inconvenience, or guesswork, but empowerment, insight, and improved quality of life. In embracing the laser glucose monitor revolution, we are not just advancing technology—we are redefining care for millions around the world.
non-invasive glucose monitoring, painless blood sugar testing, continuous glucose tracking, diabetes technology innovations, smart diabetes devices, wearable health monitors, blood sugar trends analysis, real-time glucose readings, optical glucose sensing, diabetes management tools, glucose monitoring without needles, artificial intelligence in diabetes care, predictive glucose analytics, mobile health for diabetics, personalized diabetes care, advanced biosensor technology, digital health platforms, photonic medical devices, diabetes self-management tools, future of diabetes treatment
Further Reading:
Non-invasive glucose prediction and classification using NIR technology with machine learning
‘Noninvasive’ Glucose Monitoring for Diabetes: Where Is It Now?
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.


