Introduction: The Evolving Landscape of Systemic Cancer Treatment
Cancer, once regarded as a terminal diagnosis in many of its forms, has increasingly become a manageable condition for countless patients across the globe. This paradigm shift is largely attributed to breakthroughs in systemic cancer treatment—interventions that circulate throughout the body, targeting cancer cells wherever they may reside. These therapies have reshaped how we understand, diagnose, and treat a multitude of malignancies, particularly in cases where cancer has spread beyond its point of origin.
You may also like: Cancer Research Breakthroughs: How Modern Advancements Are Transforming Treatment
Unlike localized interventions such as surgery or radiation, systemic therapy for cancer works on a whole-body level. This approach is especially crucial for patients with advanced or metastatic disease, where targeting every tumor site individually is neither practical nor effective. In recent years, systemic treatment has expanded far beyond traditional chemotherapy. Now, it encompasses sophisticated immunotherapies, targeted drug regimens, hormone therapies, and even cell-based treatments such as CAR-T therapy.
Understanding the Foundations of Systemic Therapy for Cancer
Systemic therapy for cancer refers to any treatment that enters the bloodstream and travels throughout the body to destroy or inhibit the growth of cancer cells wherever they are found. This approach contrasts with local therapies like surgery and radiation, which target specific areas of the body. The goal of systemic therapy is not just to treat the primary tumor but also to eradicate microscopic metastases that may not yet be detectable through imaging or biopsy.
The earliest forms of systemic cancer treatment emerged with the development of cytotoxic chemotherapy in the mid-20th century. While chemotherapy was revolutionary at the time, its lack of specificity meant that healthy cells—particularly those that divide rapidly—were often caught in the crossfire, leading to a host of debilitating side effects. Today, systemic therapy includes a diverse range of mechanisms. Hormone therapies, such as those used in breast and prostate cancers, disrupt the signals that fuel tumor growth. Targeted therapies are designed to interfere with specific molecular pathways involved in cancer progression.
The Role of Targeted Therapy in Precision Oncology
Targeted therapies have fundamentally redefined systemic cancer treatment by introducing a level of precision that was previously unattainable. These drugs are designed to interfere with specific molecules—often proteins or genes—that play a critical role in cancer cell survival, proliferation, or metastasis. By focusing on these unique molecular features, targeted therapies can exert powerful anticancer effects with fewer side effects compared to traditional chemotherapy.
The development of PARP inhibitors for BRCA-mutated ovarian and breast cancers exemplifies how genetic profiling can guide treatment selection. These drugs exploit the concept of synthetic lethality, disabling cancer cells’ ability to repair DNA damage while sparing healthy cells. As the field advances, newer generations of targeted therapies are being developed to overcome resistance mechanisms that cancer cells evolve in response to treatment.
Targeted therapy’s contributions to systemic therapy for cancer extend beyond just tumor suppression. They have also enabled more effective use of combination strategies, often pairing targeted drugs with immunotherapies or chemotherapy to maximize response. Importantly, the ability to match a drug to a tumor’s unique genetic profile has brought oncology into the era of precision medicine, where treatment decisions are informed by the biology of each individual’s cancer.
Immunotherapy and the Immune System’s Expanding Role in Systemic Cancer Treatment
Among the most revolutionary advancements in systemic cancer treatment is the rise of immunotherapy. This approach harnesses the patient’s immune system to detect, attack, and destroy cancer cells. For decades, the idea that the immune system could be trained or stimulated to fight cancer remained theoretical. But with the advent of immune checkpoint inhibitors, therapeutic cancer vaccines, and cell-based immunotherapies, that vision has become a reality.
This strategy has shown remarkable success in cancers that were once considered difficult to treat. Melanoma, for instance, has seen a dramatic increase in long-term survival rates with the use of checkpoint inhibitors. Similarly, patients with certain types of lung, kidney, and bladder cancers have experienced improved outcomes through immunotherapy.
Despite its promise, immunotherapy is not without risks. Immune-related adverse events, including inflammation of the lungs, colon, or endocrine organs, can be serious. Nonetheless, with careful monitoring and management, immunotherapy remains a cornerstone of modern systemic therapy for cancer, offering the potential for durable, long-term remission in ways previously unseen.
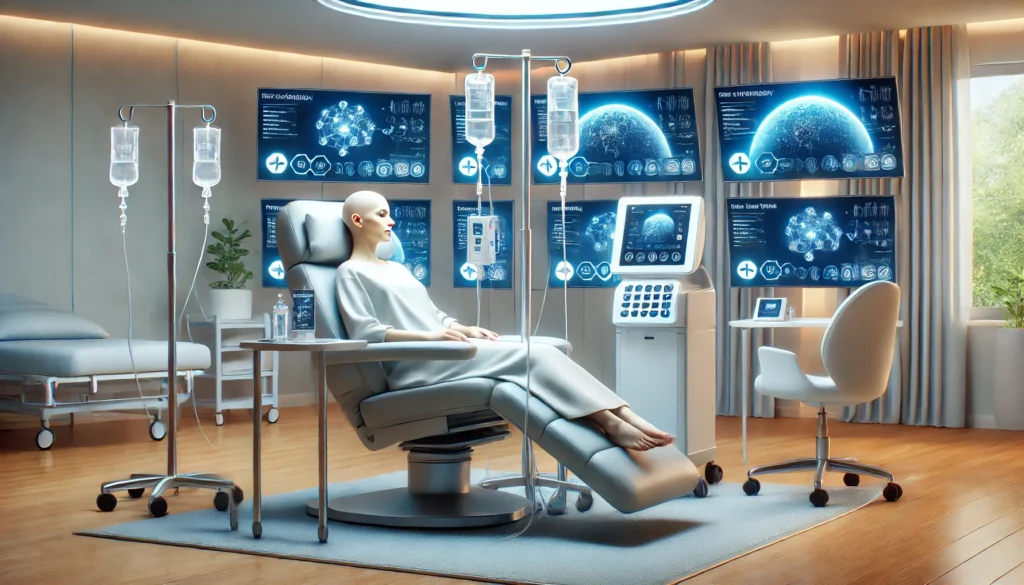
Hormonal Therapies and the Endocrine Dimension of Systemic Cancer Treatment
While often overshadowed by newer technologies, hormonal therapy remains a vital component of systemic cancer treatment, particularly for hormone-sensitive malignancies like breast and prostate cancer. These therapies work by disrupting the hormonal signals that fuel tumor growth, either by blocking hormone receptors or by reducing hormone production within the body.
In breast cancer, estrogen plays a central role in driving tumor progression in approximately 70% of cases. Selective estrogen receptor modulators (SERMs), such as tamoxifen, and aromatase inhibitors, such as letrozole and anastrozole, help to suppress this hormonal influence. These drugs are often used as adjuvant therapy following surgery to prevent recurrence or as long-term maintenance therapy in metastatic disease.
Hormonal therapy’s role in systemic therapy for cancer lies not only in tumor control but also in its ability to maintain a more favorable side effect profile compared to traditional cytotoxic treatments. While endocrine therapies do have adverse effects—such as bone density loss, hot flashes, or cardiovascular changes—they are generally more tolerable and can be used over extended periods.
Overcoming Resistance and Relapse in Systemic Cancer Therapy
While systemic therapy for cancer has made remarkable strides, the development of resistance remains a formidable challenge. Many patients who initially respond well to treatment eventually experience disease progression as cancer cells adapt and evolve mechanisms to evade therapy. Understanding and overcoming this resistance is now a major focus of oncology research.
Resistance can emerge through a variety of biological processes. Cancer cells may acquire secondary mutations that render a drug ineffective, activate alternative signaling pathways, or alter the tumor microenvironment to become less hospitable to immune cells or therapeutic agents. For example, in EGFR-mutant lung cancer, the T790M mutation often arises after treatment with first-generation EGFR inhibitors, necessitating the use of third-generation drugs like osimertinib.
Overcoming resistance is not solely about switching drugs; it often requires a deeper understanding of the tumor’s evolutionary trajectory, its interaction with the immune system, and its response to environmental stressors. By integrating genomic, proteomic, and immunologic data, oncologists can design more resilient treatment strategies that stay one step ahead of the disease.
Bridging Access and Equity in the Era of Systemic Cancer Treatment
As systemic cancer treatment continues to evolve, the conversation must also expand to include issues of access, equity, and healthcare infrastructure. The latest therapies—particularly targeted treatments, immunotherapies, and cell-based interventions—are often expensive, complex to administer, and concentrated in major academic or research institutions. These realities create significant barriers for patients in underserved communities, rural areas, and low- and middle-income countries, where advanced care may be limited or unavailable.
Efforts are underway to reduce these disparities. Global health initiatives are working to improve the availability of generic versions of key cancer drugs, expand telemedicine platforms, and decentralize clinical trial participation. Biosimilars—biologic drugs that are highly similar to approved reference products—are emerging as a more affordable alternative to costly branded medications, helping to bring systemic cancer treatment to a broader population.
Looking Ahead: The Future of Systemic Cancer Treatment
The trajectory of systemic cancer treatment is one of increasing sophistication, personalization, and integration. As our understanding of cancer biology deepens, new treatment modalities will continue to emerge, each building upon the successes and lessons of those that came before. The future promises a dynamic and adaptive ecosystem of therapies designed to outmaneuver the most complex malignancies.
Meanwhile, the convergence of immunotherapy and targeted therapy continues to yield powerful synergies. Researchers are developing next-generation agents that can modify the tumor microenvironment, recruit immune cells more effectively, and overcome resistance mechanisms. Combinatorial regimens that pair immunotherapies with targeted inhibitors, epigenetic drugs, or even metabolic modulators are opening new frontiers in systemic cancer treatment.
Frequently Asked Questions: Breakthroughs in Systemic Cancer Treatment
1. How is artificial intelligence shaping the future of systemic therapy for cancer?
Artificial intelligence (AI) is emerging as a transformative force in systemic therapy for cancer, enabling deeper insights into tumor biology and patient-specific treatment responses. AI tools are being trained on vast datasets—including genomic profiles, clinical trial results, and treatment histories—to identify patterns and predict optimal therapeutic strategies. This is particularly valuable in systemic cancer treatment, where the complexity of multi-organ disease requires rapid, data-driven decision-making. Beyond selecting therapies, AI algorithms are helping detect resistance mutations early by analyzing subtle changes in circulating tumor DNA. As these technologies advance, AI may soon assist in tailoring combination regimens for each patient, maximizing efficacy while minimizing unnecessary toxicity.
2. Can lifestyle modifications enhance the effectiveness of systemic cancer treatment?
While systemic cancer treatment primarily relies on pharmacological interventions, emerging evidence suggests that certain lifestyle choices can modulate the body’s response to therapy. Maintaining a balanced diet rich in anti-inflammatory nutrients, engaging in regular moderate physical activity, and managing stress have been linked to improved immune function and better tolerance to systemic therapy for cancer. For example, exercise has been shown to enhance lymphatic flow, potentially improving drug distribution and immune cell trafficking. Additionally, interventions like mindfulness-based stress reduction may mitigate treatment-related fatigue, improving overall adherence to therapy. These adjunctive measures do not replace medical treatment but may support more favorable outcomes when integrated into a comprehensive care plan.
3. What role does the gut microbiome play in systemic therapy for cancer?
The gut microbiome is increasingly recognized as a key player in determining how patients respond to systemic cancer treatment, especially immunotherapy. Certain bacterial strains in the gut are associated with enhanced T-cell activation and improved immune checkpoint inhibitor efficacy. Conversely, dysbiosis—an imbalance of microbial populations—may reduce treatment effectiveness and increase inflammation. Studies are now exploring whether fecal microbiota transplants or targeted probiotics can optimize the microbiome to boost systemic therapy responses. As this field matures, future systemic therapy for cancer may involve not only analyzing a tumor’s genomics but also profiling a patient’s microbiota to personalize treatment even further.
4. How are systemic treatments being adapted for pediatric cancer patients?
Adapting systemic cancer treatment for children presents unique challenges, as pediatric cancers differ biologically from adult malignancies, and young patients are more vulnerable to long-term side effects. Researchers are developing pediatric-specific dosing protocols and formulating systemic therapies with reduced toxicity profiles. In addition, clinical trials focused on childhood cancers are now exploring the use of systemic therapy for cancer in combination with advanced supportive care to protect developing organs. Gene-targeted drugs and immunotherapies tailored to the distinct molecular drivers of pediatric tumors are also gaining momentum. Importantly, survivorship programs are being built into treatment protocols to monitor and manage delayed complications of systemic interventions over a lifetime.
5. Are there psychosocial factors that affect a patient’s response to systemic therapy?
Yes, psychosocial well-being plays a significant role in how patients tolerate and respond to systemic cancer treatment. Factors such as social support, mental health status, and financial stability can influence medication adherence, recovery rates, and even immunological resilience. Chronic stress and depression have been linked to impaired immune function, which can blunt the effectiveness of systemic therapy for cancer, particularly in immunotherapy-based treatments. Oncology teams increasingly incorporate mental health professionals and patient navigators into care plans to address these variables. Recognizing and supporting psychosocial health is not ancillary—it is a critical component of successful systemic cancer treatment.
6. How does systemic cancer treatment impact long-term survivorship and aging?
As survival rates improve, long-term survivorship is becoming a central focus in oncology. Systemic therapy for cancer can have lingering effects on cardiovascular health, cognitive function, and bone density—especially when administered over extended periods. Survivors often require ongoing monitoring for secondary cancers or late-emerging toxicities related to prior systemic cancer treatment. Research is now emphasizing the development of less toxic agents, as well as interventions to rehabilitate post-treatment patients physically and psychologically. The emerging field of geriatric oncology is particularly focused on how aging interacts with systemic therapies, aiming to balance efficacy with preservation of function and independence in older adults.
7. How are rare cancers being treated with emerging systemic therapies?
Rare cancers have traditionally lacked robust treatment guidelines due to limited research and small patient populations. However, advancements in systemic cancer treatment—particularly tumor-agnostic therapies—are helping close this gap. Molecular profiling allows rare tumors to be treated based on their genetic features rather than tumor origin. For instance, if a rare cancer expresses a targetable mutation like NTRK fusion or MSI-H, systemic therapy for cancer can be selected from a broader drug arsenal. Precision medicine initiatives are also improving trial access for rare cancer patients by designing basket trials that group patients by biomarkers instead of tumor type, vastly expanding their options for systemic treatment.
8. What are some emerging delivery methods for systemic therapy for cancer?
Traditional delivery of systemic therapies—often via intravenous infusion—is being supplemented by new technologies designed to improve precision and convenience. Oral formulations are gaining popularity, allowing patients to administer systemic therapy for cancer at home while maintaining consistent blood levels. Nanoparticle-based drug delivery systems are also under development, enabling targeted release of therapeutic agents directly at tumor sites, thereby minimizing systemic toxicity. Researchers are investigating implantable pumps and biodegradable depots that offer controlled, sustained drug release over time. These innovations not only improve patient quality of life but also enhance therapeutic adherence and pharmacodynamic efficiency.
9. Can systemic therapies prevent cancer recurrence after remission?
Maintenance therapy using systemic cancer treatment is an emerging strategy to reduce the risk of relapse following successful initial treatment. This approach involves continuing a less intense form of systemic therapy to suppress residual disease and prevent dormant cancer cells from reactivating. PARP inhibitors in BRCA-mutated ovarian cancer and lenalidomide in multiple myeloma are notable examples where maintenance regimens have extended progression-free survival. Personalized risk assessments using circulating tumor DNA or other biomarkers are helping determine which patients may benefit most from ongoing systemic therapy for cancer. This paradigm shift from curative to proactive management reflects the chronic disease model now applied to many cancers.
10. What innovations are improving access to systemic cancer treatment in underserved areas?
Global disparities in cancer care access remain a major concern, but several innovations are helping address these inequities. Mobile oncology clinics equipped to deliver systemic therapy in rural regions, digital health platforms that support remote monitoring, and the development of oral systemic cancer treatments have improved reach. Tele-oncology is allowing specialists to consult with community providers in real-time, expanding systemic therapy for cancer to populations previously excluded from cutting-edge care. Furthermore, international collaborations are working to license biosimilars and generic versions of high-cost drugs to increase affordability. These efforts aim to ensure that advancements in systemic cancer treatment benefit not only those in major medical centers but also patients worldwide.

Conclusion: How Breakthroughs in Systemic Cancer Treatment Are Redefining Hope for Patients Everywhere
The last two decades have seen a profound transformation in how we understand and treat cancer, fueled in large part by breakthroughs in systemic cancer treatment. From the advent of molecularly targeted therapies and immunotherapy to the emergence of CAR-T cells and tumor-agnostic drugs, the systemic approach has shifted from a generalized, high-toxicity model to one of personalized, precision-driven care. These advancements are no longer theoretical—they are being implemented every day in oncology clinics, changing lives and redefining what is possible for patients diagnosed with cancer.
AIn this journey, what remains constant is the unwavering commitment to improving patient outcomes. Systemic cancer treatment has proven to be not just a medical intervention, but a gateway to hope—hope grounded in science, reinforced by experience, and shared by millions across the world who are fighting cancer every day. For patients, caregivers, and healthcare providers alike, these breakthroughs represent more than just progress. They represent the promise of a future where cancer is no longer a life sentence, but a life challenge—one that can be met with courage, resilience, and the best that modern medicine has to offer.
advanced cancer therapies, personalized cancer treatment, immunotherapy innovations, precision oncology, targeted drug delivery, molecular profiling in cancer, tumor microenvironment, cancer biomarkers, CAR-T cell therapy, oncology research breakthroughs, hormone-sensitive cancers, cancer immunology, cancer treatment resistance, oncology clinical trials, genomic medicine in oncology, cancer survivorship care, tumor-agnostic therapies, emerging cancer drugs, next-generation cancer therapies, liquid biopsy in oncology
Further Reading:
Advancements in Systemic Therapies for Cancer Treatment
Systemic cancer therapy: achievements and challenges that lie ahead
Advancements in Systemic Therapy for Pancreatic Cancer
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.