Introduction: The Rise of TIL Cancer Therapy in the Fight Against Melanoma
In the ever-evolving landscape of cancer treatment, few breakthroughs have generated as much hope and scientific enthusiasm as tumor-infiltrating lymphocyte (TIL) therapy. At the heart of this innovation is the ability to harness the body’s own immune system—specifically, the lymphocytes that naturally migrate into tumors—to fight cancer from within. As immunotherapy continues to reshape oncology, TIL therapy has emerged as a beacon of promise for patients facing advanced-stage malignancies, particularly melanoma, a notoriously aggressive form of skin cancer.
You may also like: Cancer Research Breakthroughs: How Modern Advancements Are Transforming Treatment
Melanoma poses unique challenges in oncology due to its high metastatic potential and resistance to traditional chemotherapy. However, recent clinical successes using TIL cancer therapy have ignited renewed optimism. By isolating and expanding these naturally occurring immune cells, researchers can effectively amplify the body’s own cancer-fighting arsenal. With the FDA granting breakthrough therapy designations and clinical trials reporting prolonged remissions, TIL treatment for melanoma is no longer experimental—it is entering a new phase of mainstream integration into oncologic practice.
Understanding TIL Therapy: A Revolution in Personalized Cancer Immunotherapy
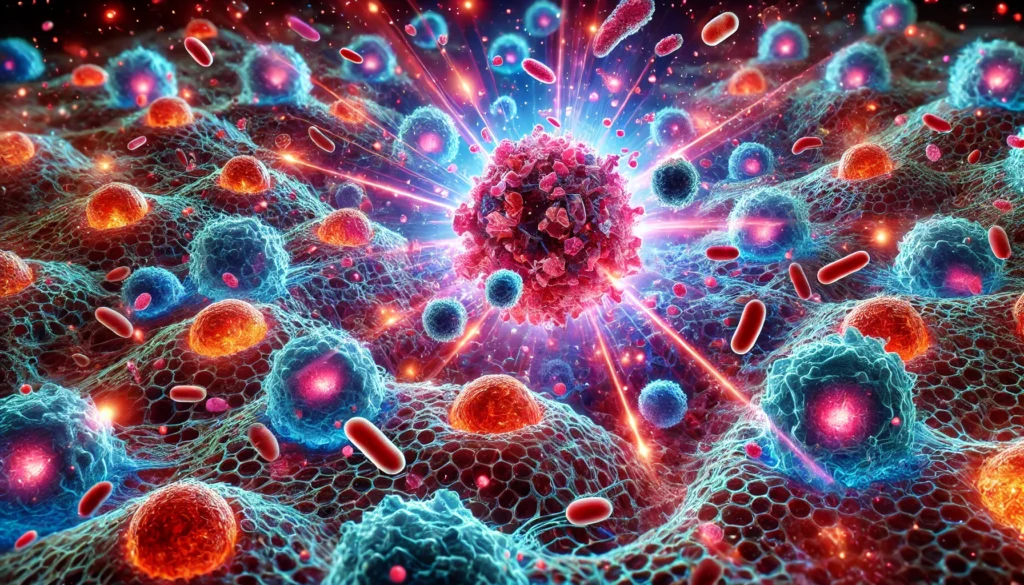
Tumor-infiltrating lymphocytes, or TILs, are a type of immune cell naturally drawn into tumors by the body’s immune surveillance mechanisms. These lymphocytes, primarily composed of T-cells, can recognize and attack cancer cells but often become overwhelmed by the immunosuppressive environment within the tumor microenvironment. This approach supercharges the immune response, creating a robust attack force of cells pre-programmed to target that patient’s specific cancer.
TIL therapy differs from other forms of immunotherapy in several important ways. Unlike immune checkpoint inhibitors, which release the brakes on existing immune responses, or CAR-T therapies, which involve genetic modification of immune cells, TIL therapy relies on the natural tumor-specific reactivity of the lymphocytes already present within the tumor. This gives TIL therapy a unique level of specificity and reduces the risk of off-target effects, which can occur with some other immunotherapies. Moreover, TIL cancer therapy can be personalized down to the cellular level, as it originates directly from each individual patient’s tumor.
Why Melanoma Is an Ideal Candidate for TIL Therapy
Melanoma has been at the forefront of immunotherapy research, not only due to its high immunogenicity but also because of its frequent resistance to traditional treatments. Chemotherapy offers limited long-term benefit, and while checkpoint inhibitors have revolutionized care for many, they don’t work for all patients. This has prompted researchers to explore other immunotherapeutic options like til treatment for melanoma.
Several features make melanoma especially receptive to til cancer treatment. First, melanoma cells tend to carry a high mutation burden, meaning they generate many abnormal proteins—neoantigens—that the immune system can potentially recognize. This increases the likelihood that TILs within the tumor will be tumor-reactive. Second, melanoma tumors often contain a relatively high number of TILs naturally, making it easier to extract and expand these cells for therapy. Third, melanoma’s behavior and progression patterns are well studied, allowing clinical researchers to identify ideal intervention points for TIL-based treatment.

Clinical Evidence: TIL Therapy Shows Durable Responses in Melanoma
The clinical data supporting til melanoma treatment continues to grow with each passing year. One of the most notable studies came from the National Cancer Institute (NCI), where Dr. Steven Rosenberg and his team conducted multiple trials demonstrating objective response rates between 40% and 50% in patients with metastatic melanoma treated with TILs. Some of these responses lasted for years, a significant achievement in patients who had exhausted all other treatments.
More recently, the biotech company Iovance Biotherapeutics developed Lifileucel, a commercial form of TIL therapy specifically for melanoma. In clinical trials involving heavily pretreated patients, Lifileucel demonstrated an objective response rate of 36% and a disease control rate exceeding 80%, with some complete responses persisting beyond 24 months. These results were strong enough to prompt the FDA to grant breakthrough designation, a sign of confidence in the treatment’s potential.
Expanding Horizons: Beyond Melanoma and Into New Cancer Frontiers
While melanoma remains the most studied and successful target for TIL cancer therapy, the approach is not limited to skin cancer alone. Ongoing clinical trials are investigating the application of TIL therapy in cervical cancer, non-small cell lung cancer, head and neck squamous cell carcinoma, and triple-negative breast cancer. Early results suggest that tumour infiltrating lymphocytes melanoma research may offer a template for success in other solid tumors.
These efforts involve not only refining extraction and expansion techniques but also identifying biomarkers that predict TIL reactivity. For example, tumors with high mutational burden, dense immune infiltrates, or PD-L1 expression may be more likely to respond to TIL-based treatments. New studies are also exploring combinations of TIL therapy with checkpoint inhibitors, radiation, or oncolytic viruses to boost efficacy even further.
The Road Ahead: Innovation, Challenges, and the Path to Mainstream Use
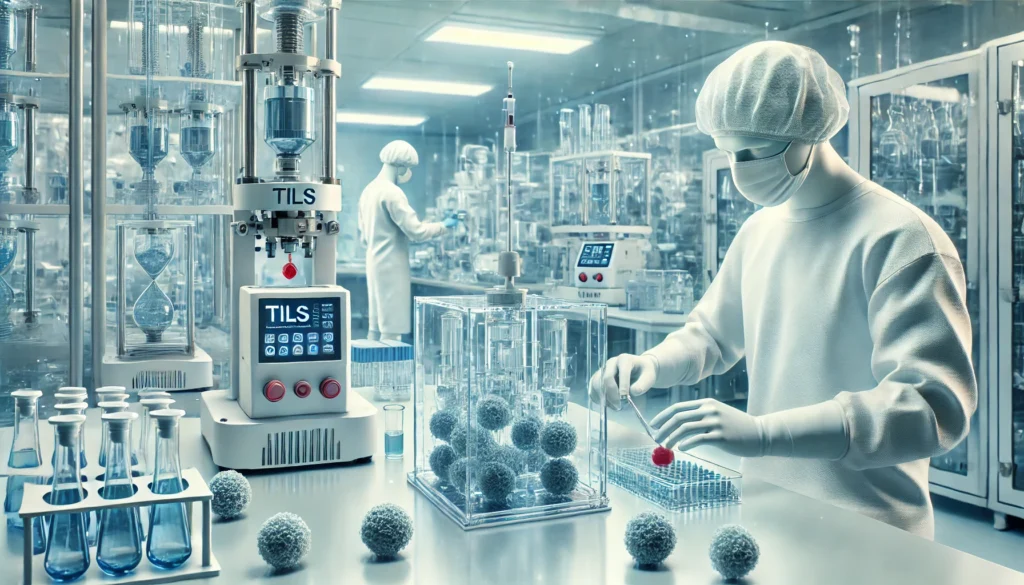
As til therapy melanoma gains clinical traction, several key challenges must be addressed to bring it into wider use. Manufacturing timelines currently range from two to five weeks, which may not be ideal for patients with rapidly progressing disease. Innovations in rapid expansion protocols and cryopreservation of TILs are being tested to shorten treatment windows.
Another issue is patient selection. Not all tumors yield viable TILs, and some patients may not have enough tumor tissue to harvest. New imaging and biopsy-guided techniques aim to optimize tumor sampling and maximize therapeutic cell yield. Moreover, as TIL therapies enter phase III trials, regulators and payers are demanding robust data on long-term outcomes, safety, and cost-effectiveness.
Nevertheless, the momentum is clear. With FDA designations, growing clinical experience, and commercial products entering the market, til cancer therapy is transitioning from experimental concept to therapeutic cornerstone.
Frequently Asked Questions (FAQ): Tumor-Infiltrating Lymphocyte (TIL) Cancer Therapy for Melanoma
1. How does TIL therapy for melanoma compare to CAR T-cell therapy in terms of adaptability across solid tumors?
TIL therapy for melanoma offers unique advantages over CAR T-cell therapy when targeting solid tumors. Unlike CAR T-cell therapy, which requires engineering cells to recognize specific antigens, TIL cancer treatment uses naturally occurring immune cells extracted directly from the patient’s tumor, already primed to recognize diverse tumor antigens. This makes TIL tumor therapy inherently adaptable to a broader array of mutations and tumor types, especially in the genetically diverse landscape of melanoma. Additionally, TIL therapy has shown promise in treating solid tumors with high mutation burdens, where the immune system can better identify neoantigens. While CAR T therapies excel in hematological cancers, TIL cancer therapy is emerging as a frontrunner in solid tumor immunotherapy, particularly for difficult-to-treat cases like metastatic melanoma.
2. What are some emotional and psychological considerations for patients undergoing TIL cancer therapy?
Undergoing TIL cancer therapy can be emotionally taxing due to the intensive nature of the treatment process and the uncertainty of outcomes. Many patients experience anxiety prior to hospitalization, especially when anticipating the lymphodepletion phase and subsequent cell infusion. The high expectations surrounding til therapy melanoma success rates can also create pressure, leading to emotional highs and lows during recovery. Psychologically, patients may struggle with isolation during the treatment period due to immune suppression precautions. Long-term support systems, including counseling and peer networks, can play a crucial role in helping patients manage the emotional toll of TIL melanoma therapy, ultimately contributing to better mental and physical outcomes.
3. Are there long-term health risks associated with TIL treatment for melanoma?
Yes, while TIL treatment for melanoma is promising, it can carry long-term risks that should be weighed carefully. The preparative lymphodepletion phase, which involves high-dose chemotherapy, can have lingering effects on bone marrow function and immune competency. Some patients may experience chronic fatigue or hormone imbalances due to collateral damage to endocrine organs. Additionally, exposure to interleukin-2 (IL-2), which is often used to boost TIL cell activity post-infusion, can lead to vascular leak syndrome or cardiac complications in rare cases. Patients who receive TIL cancer therapy are advised to undergo long-term monitoring for organ function and secondary autoimmune responses. These potential risks underscore the need for expert care teams experienced in managing TIL cancer.
4. How accessible is TIL therapy today, and what factors affect patient eligibility?
Access to TIL therapy remains limited to specialized cancer centers and clinical trials, although this is rapidly changing. One of the key barriers is the complex, time-sensitive process of harvesting and expanding tumour infiltrating lymphocytes melanoma cells in the lab. Patients must have resectable tumors suitable for biopsy, be in good general health to withstand chemotherapy, and have melanoma that is resistant to first-line immunotherapies. Factors such as insurance approval, geographic proximity to a TIL therapy facility, and the availability of trial slots also affect eligibility. However, with the FDA’s recent focus on breakthrough immunotherapies, access to TIL cancer treatment is expected to expand over the next few years, potentially increasing availability beyond major academic institutions.
5. What role does the tumor microenvironment play in the success of TIL therapy?
The tumor microenvironment plays a pivotal role in determining the effectiveness of TIL therapy. A hostile microenvironment—rich in immunosuppressive factors like TGF-beta or regulatory T cells—can hinder the activity of infused TILs. Successful til cancer therapy often depends on the ability of TILs to overcome this suppressive setting and remain functional long enough to attack the tumor effectively. Advances in pre-conditioning regimens are being studied to modify the tumor microenvironment before TIL administration, aiming to make it more conducive to immune activity. Furthermore, research is exploring combination therapies, such as pairing TIL treatment for melanoma with checkpoint inhibitors, to neutralize microenvironmental resistance and enhance overall response.
6. Can TIL cancer therapy be applied to cancers other than melanoma?
Although TIL therapy melanoma applications are currently the most studied and successful, the principles of this approach are being investigated for a broader range of cancers. Tumors with a high mutation burden, such as cervical, lung, and bladder cancers, show early potential for TIL tumor applications. These tumors tend to present a variety of neoantigens, increasing the likelihood that harvested TILs will target cancerous cells effectively. Clinical trials are ongoing to test the efficacy of TIL cancer treatment in these cancers, particularly in patients who have not responded to checkpoint inhibitors. As techniques for isolating and expanding TILs improve, we may see a future where TIL therapy becomes a viable option for multiple hard-to-treat solid tumors beyond melanoma.
7. How does TIL therapy cost compare with other forms of advanced immunotherapy?
TIL therapy cost can be substantial, often comparable to or exceeding the price of other advanced immunotherapies like CAR T-cell therapy. This is due in part to the labor-intensive process of harvesting, expanding, and infusing autologous TIL cells in a controlled laboratory environment. On average, the full TIL cancer treatment cycle—including hospitalization, chemotherapy, and follow-up—can exceed $400,000. However, when successful, til treatment may reduce the need for ongoing therapies, potentially lowering long-term treatment expenses. As commercial manufacturing processes for tumour infiltrating lymphocytes melanoma therapies improve, it’s anticipated that the cost will decrease, making TIL therapy more accessible to a broader range of patients and insurance providers.
8. What innovations are being developed to improve the efficiency of TIL cancer therapy?
Innovations in TIL cancer therapy are focusing on reducing the time required to expand cells, improving the selection of the most potent TILs, and enhancing their durability post-infusion. One promising development involves the use of artificial intelligence to identify the most tumor-reactive lymphocytes during the expansion phase. Researchers are also exploring “off-the-shelf” til tumor options using partially matched donor cells, which could accelerate access for urgent cases. Additionally, genetic modification of TILs to resist exhaustion and suppressive signaling is under investigation to improve their efficacy in hostile tumor environments. These innovations may transform til therapy melanoma protocols from a laborious, bespoke process into a scalable cancer treatment option.
9. How do patients typically feel after completing a round of TIL treatment?
Many patients report mixed experiences following TIL treatment. The initial recovery phase is often marked by fatigue, immune suppression, and the need for close monitoring, especially in the weeks following high-dose IL-2 therapy. However, for patients with durable responses, til melanoma treatment can provide profound relief from disease symptoms and improved quality of life. Some individuals experience long-term remission that allows for the resumption of normal daily activities, travel, and work. Emotional recovery is also significant—patients who have undergone TIL cancer therapy frequently describe a renewed sense of hope, especially after failing standard therapies. The support of multidisciplinary care teams, including mental health professionals, is crucial for helping patients adjust after completing TIL cancer treatment.
10. What is the future outlook for TIL therapy in precision oncology?
The future of TIL therapy lies in its integration into the broader landscape of precision oncology. By pairing genomic sequencing with tumour infiltrating lymphocytes melanoma profiling, clinicians can better select patients who will benefit most from TIL therapy. Moreover, as researchers gain insights into TIL biomarkers, personalized dosing regimens and cell enrichment techniques are being developed. TIL cancer therapy is expected to evolve into a standard second-line or even first-line treatment in melanoma and other mutation-rich tumors. Additionally, global investment in TIL therapy infrastructure, especially in Asia and Europe, points toward a future where til treatment is not just innovative—but widely available, scalable, and personalized for maximum impact.
Conclusion: TIL Therapy for Melanoma Marks a New Era in Precision Oncology
As we stand at the cusp of a new chapter in cancer immunotherapy, TIL therapy shines as one of the most personalized, potent, and promising approaches to treating advanced melanoma. Through the strategic use of tumour infiltrating lymphocytes melanoma treatments, clinicians are unlocking deeper and more durable responses, offering real hope where few options once existed.
Though the til therapy cost and logistical demands remain hurdles, ongoing innovation is driving progress toward broader accessibility. With research expanding into other cancers and combination regimens gaining interest, the influence of til cancer treatment is expected to grow far beyond its roots in melanoma care. As patients and physicians alike look toward more individualized, biology-driven treatments, TIL therapy is poised to play a defining role in the future of oncology.
In the fight against melanoma—and perhaps many other cancers—til cancer therapy is not just a treatment. It is a revolution born from within the tumor itself, wielding the body’s own immune system as both weapon and cure.
immunotherapy for advanced melanoma, adoptive cell therapy, immune checkpoint resistance, personalized cancer immunotherapy, metastatic melanoma treatment options, lymphodepleting chemotherapy, novel melanoma treatments, cancer cell infiltration, autologous T-cell therapy, next-generation immunotherapy, immune system and cancer, tumor microenvironment in melanoma, cancer immunotherapy breakthroughs, advanced melanoma prognosis, IL-2 cytokine therapy, precision cancer medicine, emerging cancer therapies, solid tumor immunotherapy, melanoma clinical trials, advanced oncologic treatments
Further Reading:
Tumour-infiltrating lymphocyte therapy for patients with advanced-stage melanoma
Tumor-Infiltrating Lymphocyte Therapy in Melanoma: Facts to the Future
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.


