Understanding the Electrocardiogram: What Is an EKG and What Does It Do?
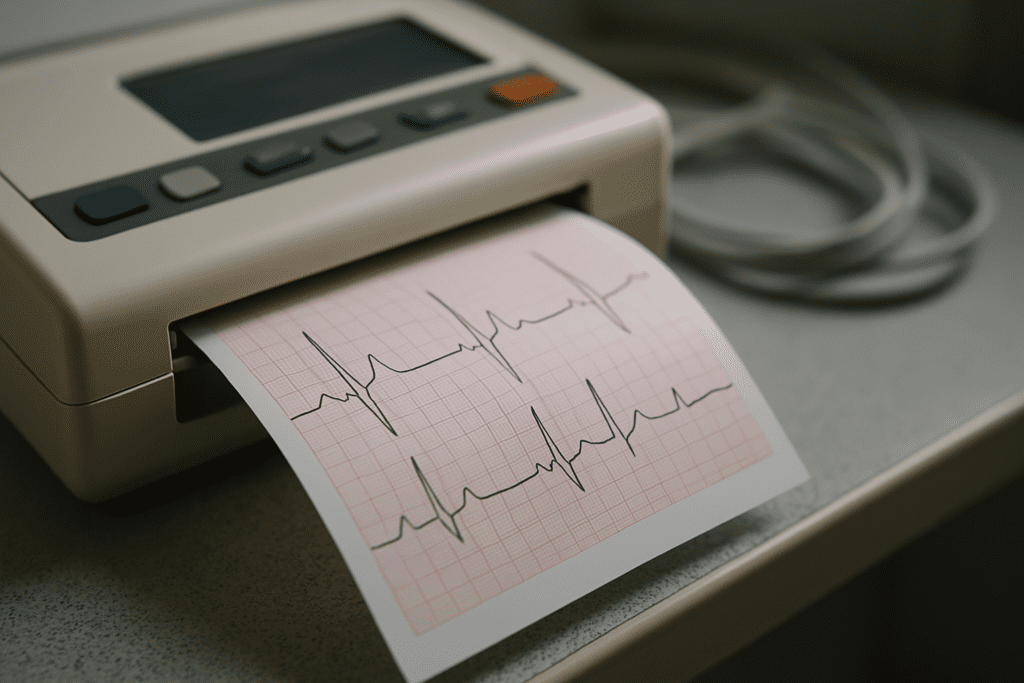
An electrocardiogram, commonly abbreviated as EKG or ECG, is one of the most widely used diagnostic tools in cardiovascular medicine. Though the terms ECG and EKG are often used interchangeably, “EKG” derives from the German word Elektrokardiogramm, while “ECG” is the direct English abbreviation of “electrocardiogram.” For patients and clinicians alike, understanding the distinction between ECG vs EKG is largely a matter of terminology, as both refer to the exact same test. The procedure itself involves placing electrodes on the skin to detect the electrical signals generated by the heart. These signals are then graphically represented as waves, which clinicians interpret to assess heart rhythm, rate, and overall function.
You may also like: Top Cardiologist-Approved Cardio Workouts to Improve Cardiovascular Fitness and Heart Health Naturally
The primary function of an electrocardiogram test is to record the timing and strength of electrical impulses traveling through the heart. These impulses control the heartbeat, and any disruption or abnormality in the pattern can point to underlying cardiac issues. The question that often arises is, “What does an EKG do that makes it so essential in emergency cardiac care?” Quite simply, it provides a real-time snapshot of heart activity, allowing medical professionals to make swift decisions during critical moments. It can detect arrhythmias, ischemia, previous heart attacks, and in some cases, structural abnormalities.
To answer “what does an EKG show,” one must delve into the various components of the EKG waveform, including the P wave, QRS complex, and T wave. Each segment corresponds to specific electrical events in the cardiac cycle. Deviations in these waves can signal serious conditions like myocardial infarction, pericarditis, or electrolyte imbalances. In the realm of emergency medicine, where every second counts, the ability of the EKG or ECG to reveal such precise information is indispensable. Thus, whether one uses the term ECG or EKG, its clinical utility remains profoundly significant in the early detection and treatment of cardiac events.
EKG Meaning and Medical Significance: Beyond the Basics
When patients hear the phrase “EKG,” they often wonder about its full implications. So, what does EKG stand for in medical terms? It stands for electrocardiogram, a noninvasive test that records the electrical activity of the heart over a short period. This is different from an electrocardiograph, which refers to the actual machine used to conduct the test. Understanding this distinction between the electrocardiogram and electrocardiograph helps patients become more informed participants in their healthcare journey.
From a medical standpoint, the EKG meaning goes far beyond a simple test result. It provides physicians with crucial insights into how the heart is functioning at any given moment. For instance, irregularities in rhythm, such as atrial fibrillation or ventricular tachycardia, are easily captured by an EKG. In more chronic conditions, the test can reveal evidence of past heart damage, such as scarring or hypertrophy. Patients might ask, “What is an EKG used for if I don’t have symptoms?” The answer lies in its utility as a preventative and diagnostic tool. It is often used in routine checkups, preoperative assessments, or during annual physical exams for patients with risk factors.
The term “EKG meaning medical” can vary depending on the context. For someone in an emergency room presenting with chest pain, an EKG could mean the difference between early intervention and irreversible heart damage. In contrast, for someone undergoing a wellness check, it may serve as a baseline for future comparisons. Either way, understanding “what does EKG stand for” enables patients to appreciate its importance in detecting subtle and sometimes silent cardiac abnormalities. As heart disease remains the leading cause of death globally, the electrocardiogram test stands out as a cornerstone of modern cardiovascular diagnostics.
Can an EKG Detect a Heart Attack? Exploring the Evidence
The question at the heart of this discussion—can an EKG detect a heart attack?—is both timely and essential. The short answer is yes, but the details matter. An EKG is one of the first diagnostic tests administered to patients suspected of having a myocardial infarction, commonly known as a heart attack. But how exactly does an EKG show a heart attack, and can an EKG determine a heart attack with high reliability?
When a person experiences a heart attack, part of the heart muscle is deprived of oxygen due to a blocked coronary artery. This oxygen deprivation alters the electrical conductivity of the heart tissue, which is picked up by the EKG in real time. The test may reveal characteristic changes, such as ST-segment elevation, T-wave inversions, or the appearance of abnormal Q waves—all of which help physicians identify the presence, severity, and location of the infarction. These patterns are so specific that clinicians are trained to recognize them within seconds, making the EKG one of the most powerful tools in acute cardiac care.
Despite its effectiveness, there are limitations. A normal EKG does not always rule out a heart attack. In some cases, especially in the early stages of myocardial infarction or in patients with small, localized damage, the EKG may appear deceptively normal. This is why doctors often use additional tests such as cardiac biomarkers (like troponin levels) and imaging studies to confirm the diagnosis. So while the EKG is critical, it is not infallible. Still, when people ask, “Can EKG show heart attack?” or “Will a heart attack show on an EKG?” the answer is usually yes—particularly when the test is administered at the right time and interpreted by experienced professionals.
What an EKG Looks Like During a Heart Attack: Comparing Heart Attack ECG vs Normal
One of the most visually compelling aspects of electrocardiography is the stark difference between a normal ECG and one recorded during a heart attack. When comparing a heart attack ECG vs normal heart patterns, the abnormalities become strikingly evident to a trained eye. In a healthy individual, the EKG will show consistent waveforms with predictable intervals. The P wave, QRS complex, and T wave are clearly delineated, and the segments between them maintain expected proportions.
In contrast, a heart attack cardiogram often displays changes such as elevated or depressed ST segments, inverted T waves, and the emergence of pathological Q waves. These patterns signify different types of myocardial infarction. For example, an ST-elevation myocardial infarction (STEMI) is characterized by a pronounced elevation in the ST segment, indicating complete blockage of a coronary artery. In non-ST-elevation myocardial infarctions (NSTEMIs), the EKG may not show dramatic ST changes, but other subtler abnormalities can still be present. This is why clinicians are trained to detect nuanced differences in heart attack ECG vs normal readings.
Patients often ask, “What does an EKG look like for a heart attack?” The answer varies depending on the stage and severity of the cardiac event, but the presence of any ST-segment abnormalities should always raise red flags. Moreover, serial EKGs—taken over time—can provide additional insights, especially in evolving infarctions. While an initial EKG may appear normal, subsequent tests may reveal developing signs of myocardial damage. In this context, knowing how to interpret “normal ECG and heart attack” presentations becomes an invaluable skill for physicians and emergency personnel.
The Role of EKG in Emergency Cardiology: Early Detection Saves Lives
In emergency medical settings, time is myocardium. This phrase underscores the critical importance of rapid diagnosis and treatment in heart attack scenarios. The electrocardiogram test is often the first line of defense in such emergencies, allowing clinicians to quickly determine the presence of ischemic changes. When someone presents with symptoms such as chest pain, shortness of breath, or radiating arm discomfort, the immediate question becomes, “Can an EKG diagnose a heart attack accurately and in time?”
Given the high stakes involved, emergency departments have protocols in place to ensure an EKG is administered within minutes of a patient’s arrival. The test not only helps in diagnosing heart attacks but also aids in stratifying risk. A severely abnormal EKG may prompt immediate interventions such as thrombolytic therapy or emergency catheterization, while a normal EKG might lead to further observational care and additional testing. The beauty of the EKG lies in its noninvasive nature—it poses no risk to the patient and can be repeated as needed.
However, patients should understand that while the EKG is highly sensitive, it is not always specific. This means it may detect abnormalities that resemble a heart attack but are caused by other conditions, such as pericarditis, left bundle branch block, or even anxiety-induced tachycardia. Therefore, “Do ECGs detect heart attacks?” Yes, but they are one piece of a larger diagnostic puzzle. Still, the EKG remains the most efficient initial screening tool in emergency cardiology. It empowers clinicians to make life-saving decisions within minutes—an extraordinary feat in modern medicine.
Why Would You Get an EKG? Common Reasons and Clinical Applications
An electrocardiogram is not reserved solely for emergencies. In fact, there are numerous reasons why a healthcare provider might order this test. When patients inquire, “What are 3 reasons a person would get an EKG?” the answers often reflect a blend of preventive, diagnostic, and monitoring purposes. First, an EKG can be used as part of a routine physical exam, especially for those with risk factors such as high blood pressure, diabetes, or a family history of heart disease. This allows clinicians to establish a baseline for future comparison.
Second, the test is often employed when someone is experiencing symptoms that could be cardiac in origin—such as dizziness, palpitations, or unexplained fatigue. Even in the absence of chest pain, these symptoms might prompt an EKG to rule out underlying arrhythmias or other abnormalities. Third, for patients with known heart conditions, the EKG serves as a monitoring tool to track disease progression or evaluate the effectiveness of treatment. Medications such as beta-blockers or antiarrhythmics can affect heart rhythms, and regular EKGs ensure these therapies are working as intended.
The versatility of the EKG is one of its greatest strengths. Whether it’s detecting subtle changes in heart function, confirming a diagnosis, or ruling out serious conditions, the electrocardiogram test plays a critical role in comprehensive cardiac care. This is why understanding the broader clinical implications of “EKG means” can enhance patient engagement and confidence in the medical process.

EKG Test Results and What They Reveal About Your Heart
Interpreting EKG test results is both an art and a science. While the machine prints out a series of waves and intervals, it is up to the clinician to decipher what those results actually mean. Each component of the waveform holds diagnostic value. For instance, a prolonged PR interval may suggest first-degree heart block, while a wide QRS complex might point to a ventricular conduction delay. Thus, when asking “What does an EKG do?” the answer encompasses not just data collection, but also complex interpretation.
Patients are often curious about their EKG test results, especially if they are normal. It’s important to note that a normal EKG does not guarantee a healthy heart in every case. Some forms of heart disease, like angina or intermittent arrhythmias, may not show up during the short duration of the test. This is why doctors often recommend additional testing, such as Holter monitoring or echocardiography, when symptoms persist despite normal EKG readings. Nevertheless, when abnormalities are present, the EKG can offer critical clues that guide further evaluation and management.
Among the most pressing concerns is whether “does EKG show heart attack?” or more precisely, can an EKG detect a heart attack in progress? As discussed earlier, the answer is frequently yes, especially when the infarction is acute and involves significant myocardial tissue. But the interpretation of EKG test results must always be placed within a broader clinical context. Combining EKG findings with patient symptoms, medical history, and additional diagnostics ensures the highest level of accuracy in cardiovascular care.
Frequently Asked Questions (FAQ): EKGs and Heart Attacks
1. How accurate is an EKG in detecting a heart attack in real-world emergency settings?
While the electrocardiogram test is highly effective in detecting acute heart attacks, its accuracy often depends on when the test is performed and how the heart is affected. In emergency medicine, the ability of an EKG to show classic signs—like ST elevation or abnormal Q waves—makes it invaluable for rapid diagnosis. However, not all heart attacks display textbook changes on an initial EKG. Silent or early-stage infarctions may require serial testing or further imaging to confirm diagnosis. This is why many hospitals utilize continuous telemetry or repeated ECGs over several hours, improving sensitivity. So, if you’re wondering “can an EKG detect a heart attack,” the answer is yes in most cases, but it’s often part of a broader diagnostic process that includes lab markers and clinical examination.
2. Why do some patients have a normal EKG even during a heart attack?
A heart attack may not always produce the hallmark signs on an electrocardiogram, especially in the case of non-ST-elevation myocardial infarctions (NSTEMIs). This discrepancy between a heart attack ECG vs normal patterns can occur due to the location of the blockage or the extent of damage. In some cases, electrical activity remains within expected limits, despite underlying ischemia. Moreover, microvascular disease—common in diabetics or women—can cause symptoms without EKG changes. When interpreting whether a heart attack will show on an EKG, physicians also consider the patient’s risk factors and symptoms, not just the test results. That’s why “does an EKG show heart attack” isn’t a yes-or-no question but depends on clinical context.
3. What’s the difference between an electrocardiogram and electrocardiograph, and why does it matter?
The terms electrocardiogram and electrocardiograph are often confused but refer to two distinct things. The electrocardiogram is the result—the graphical tracing of heart activity—while the electrocardiograph is the machine used to record it. Understanding this distinction is helpful not only in interpreting EKG test results but also in understanding the medical workflow. For instance, portable electrocardiograph devices now allow for remote monitoring, a significant innovation in telecardiology. As digital health tools evolve, knowing how the electrocardiograph integrates with cloud systems could redefine how quickly we respond to events like a heart attack EKG pattern.
4. Can wearable ECG monitors reliably detect heart attack symptoms at home?
With the advent of consumer-grade wearable technology, such as smartwatches equipped with ECG capabilities, more people are asking if these devices can detect heart attack signs. While these devices offer useful data for chronic rhythm issues like atrial fibrillation, their ability to act as a reliable heart attack cardiogram is still limited. Most wearables provide a single-lead ECG, while clinical tests typically use 12-lead configurations to detect complex issues. This difference in resolution means that although helpful, these tools should not replace a formal electrocardiogram test when heart attack symptoms appear. Users should still seek immediate medical care if they suspect an acute cardiac event, even if the wearable does not flag any abnormalities.
5. Are there non-cardiac conditions that can mimic heart attack patterns on an EKG?
Yes, several conditions can produce EKG changes that resemble those seen during a heart attack. These include electrolyte imbalances (like high potassium), pericarditis, pulmonary embolism, and even severe anxiety attacks. For this reason, understanding what does an EKG do in different physiological states becomes critical for accurate interpretation. Physicians are trained to distinguish between true infarctions and “pseudoinfarctions” by correlating EKG findings with lab tests and clinical signs. Thus, if someone asks, “can an EKG determine a heart attack for sure?” the answer is—it provides strong clues but must be interpreted in context.
6. How do age, gender, and ethnicity affect EKG interpretation in heart attack diagnosis?
There’s growing recognition that factors like age, gender, and ethnicity can influence both the presentation and interpretation of EKG results. For example, younger individuals may naturally exhibit early repolarization patterns that mimic heart attack signs. Women often present with subtler symptoms, and their heart attack EKG results may lack the classic ST elevation seen in men. Additionally, certain populations may exhibit normal EKG variants that differ from textbook examples. Therefore, understanding what an EKG looks like for a heart attack must include cultural and demographic competency. This nuanced approach is key to reducing disparities in cardiac care and outcomes.
7. Why do doctors sometimes order an EKG even when a patient has no symptoms?
An EKG is not just a diagnostic tool but also a preventative and monitoring measure. When discussing what are 3 reasons a person would get an EKG, beyond symptom-based evaluation, clinicians often cite pre-operative clearance, medication monitoring, and routine heart health assessments in high-risk patients. These applications help establish a baseline, which can later be compared with future readings to detect subtle changes. In asymptomatic individuals, changes in an ECG or EKG can flag previously undiagnosed issues like left ventricular hypertrophy or arrhythmias. Thus, the utility of an EKG goes beyond emergency use—it plays a role in comprehensive cardiovascular wellness planning.
8. Are false positives or false negatives common in EKG readings for heart attacks?
Although the electrocardiogram test is a cornerstone of cardiac diagnostics, it is not without its limitations. False positives can occur in people with pre-existing conduction abnormalities, while false negatives may arise in early-stage infarctions. The challenge lies in the fact that no single test is definitive in every case. When patients ask, “does ECG detect heart attack reliably?” or “do ECGs detect heart attacks consistently?” the answer depends on factors like timing, lead placement, and physician interpretation. New technologies like AI-assisted analysis are being developed to reduce human error and increase diagnostic accuracy, offering promising advances in cardiac care.
9. How are EKG results used during long-term cardiac rehabilitation?
After a heart attack, an EKG is often used as a monitoring tool in rehabilitation settings. It helps clinicians track changes in rhythm and recovery of cardiac function over time. Understanding the differences in a heart attack ECG vs normal readings becomes particularly important during stress testing. This allows rehab professionals to tailor exercise protocols that are both safe and effective. Moreover, subtle shifts in EKG test results during physical exertion can indicate whether a patient is recovering adequately or needs further intervention. In this sense, asking “what does an EKG show after a heart attack?” opens a conversation about ongoing cardiac care and prevention of future events.
10. What role will AI and machine learning play in the future of EKG interpretation?
Artificial intelligence is poised to transform how we analyze electrocardiograms. Currently, AI models are being trained to recognize complex patterns in ECG or EKG readings that even experienced cardiologists might miss. These systems can assist in identifying rare arrhythmias, predicting cardiac arrest risk, or even distinguishing between normal ECG and heart attack signals in ambiguous cases. As these technologies advance, they may reduce diagnostic errors and shorten the time it takes to interpret heart attack EKGs in emergency settings. Still, human oversight will remain essential, especially when contextualizing what does an EKG show within a broader clinical picture.
Conclusion: How EKG Tests Help Detect Heart Attacks and Protect Heart Health
In the grand landscape of cardiovascular diagnostics, few tools offer the immediacy, precision, and life-saving potential of the electrocardiogram test. For patients wondering, “Can an EKG detect a heart attack?” the evidence is overwhelmingly affirmative—especially when interpreted by trained professionals within the right clinical setting. Whether you’re grappling with symptoms of chest discomfort or simply undergoing a routine heart health check, the EKG provides a window into your cardiac function that few other tests can match.
From clarifying the nuances of ECG vs EKG and exploring what does an EKG show, to understanding how an EKG or ECG can differentiate between a normal ECG and heart attack scenarios, this diagnostic modality proves invaluable across a spectrum of clinical situations. It not only helps confirm or rule out the occurrence of a heart attack, but also contributes to ongoing cardiac monitoring, medication management, and risk assessment.
Incorporating the electrocardiogram and electrocardiograph into routine care, especially for those at high cardiovascular risk, represents a proactive approach to heart health. While no single test offers a complete picture, the EKG stands out for its speed, noninvasiveness, and diagnostic clarity. Ultimately, its role in detecting early warning signs, initiating rapid intervention, and improving survival rates cannot be overstated. As heart disease continues to affect millions worldwide, timely access to and understanding of EKG test results could be the difference between recovery and tragedy. In this light, embracing the insights provided by the EKG is not just medically wise—it’s potentially lifesaving.
cardiac rhythm analysis, heart monitoring test, signs of myocardial infarction, electrocardiogram interpretation, heart diagnostic tools, cardiovascular emergency response, ischemic heart disease detection, noninvasive heart testing, abnormal heart rhythms, electrical activity of the heart, acute coronary syndrome evaluation, cardiology diagnostic procedures, ECG waveform abnormalities, silent heart attack signs, heart health screening, ventricular arrhythmia detection, emergency heart assessment, interpreting ECG readings, cardiac waveform analysis, early heart attack warning signs
Further Reading:
Electrocardiogram (ECG or EKG)
Can an EKG Detect a Previous Heart Attack?
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.


