The relationship between birth control pills and high blood pressure is a medically significant topic that continues to gain attention among healthcare professionals, researchers, and patients alike. As millions of women worldwide rely on hormonal contraceptives for family planning and health management, understanding how these medications may affect cardiovascular health is critical. Among the concerns raised in recent years is the possibility that birth control pills may elevate blood pressure, potentially increasing the risk of hypertension and related cardiovascular complications. In this article, we explore the scientific evidence behind the question: can birth control cause high blood pressure? Drawing on current research and clinical insights, we’ll examine how different types of birth control interact with the cardiovascular system, who is most at risk, and how to make informed, medically sound decisions regarding contraceptive use.
You may also like: Sudden Spikes in Blood Pressure: What Can Cause a Sudden Increase and When to Seek Medical Attention
How Hormonal Birth Control Works and Its Systemic Effects
Hormonal birth control methods primarily work by altering a woman’s hormonal balance to prevent ovulation, change cervical mucus consistency, and modify the uterine lining to reduce the likelihood of pregnancy. The most common forms include combined oral contraceptive pills (which contain both estrogen and progestin) and progestin-only pills. These hormones mimic natural reproductive hormones but at levels and combinations designed to suppress fertility.
While effective for contraception, these synthetic hormones can have broad systemic effects beyond the reproductive system. Estrogen, in particular, has known effects on the vascular system. It can influence blood vessel tone and fluid retention, which in turn may contribute to elevated blood pressure in some individuals. The interplay between estrogen and the renin-angiotensin-aldosterone system—a hormonal system that regulates blood pressure and fluid balance—is one area where scientists have observed potential cardiovascular impacts. These interactions underscore why the connection between birth control pills and high blood pressure is of clinical interest and deserving of further exploration.
Evidence Linking Birth Control Pills and High Blood Pressure
The question of whether birth control pills and high blood pressure are linked has been addressed in several large-scale epidemiological studies and clinical trials. Research has consistently shown that women who use combined oral contraceptives (COCs) may experience a slight but measurable increase in blood pressure. According to data published in the journal Hypertension, women taking COCs are more likely to develop hypertension compared to non-users, particularly when use is prolonged over many years.
Notably, the increase in blood pressure associated with COCs tends to be dose-dependent. Earlier formulations of the pill, which contained higher doses of estrogen, were associated with a more significant rise in blood pressure. Today, most birth control pills contain much lower estrogen concentrations, which has helped mitigate some of these effects. However, even with lower estrogen doses, there is still evidence that certain individuals remain at risk. Understanding whether birth control can cause high blood pressure is not a matter of yes or no but rather one of assessing risk factors, formulation types, and individual variability.

Who Is Most at Risk for Developing High Blood Pressure on Birth Control?
The risk of elevated blood pressure from birth control use is not evenly distributed among all women. Certain populations are more susceptible due to a range of genetic, lifestyle, and health-related factors. For example, women with a family history of hypertension, preexisting cardiovascular disease, or conditions such as diabetes or kidney disease may be at heightened risk.
Age is another important consideration. Women over the age of 35 who smoke and take birth control pills face a significantly increased risk of developing high blood pressure and even more serious cardiovascular events such as heart attack or stroke. This is why healthcare providers typically recommend alternative forms of contraception for older women who smoke or have other cardiovascular risk factors.
Obesity, sedentary lifestyle, and high dietary sodium intake can also exacerbate the hypertensive effects of birth control pills. For these reasons, routine blood pressure monitoring is advised for all women using hormonal contraception. Identifying whether birth control pills and high blood pressure are a personal concern requires a thorough health assessment and ongoing vigilance.
Mechanisms Behind the Blood Pressure Increase
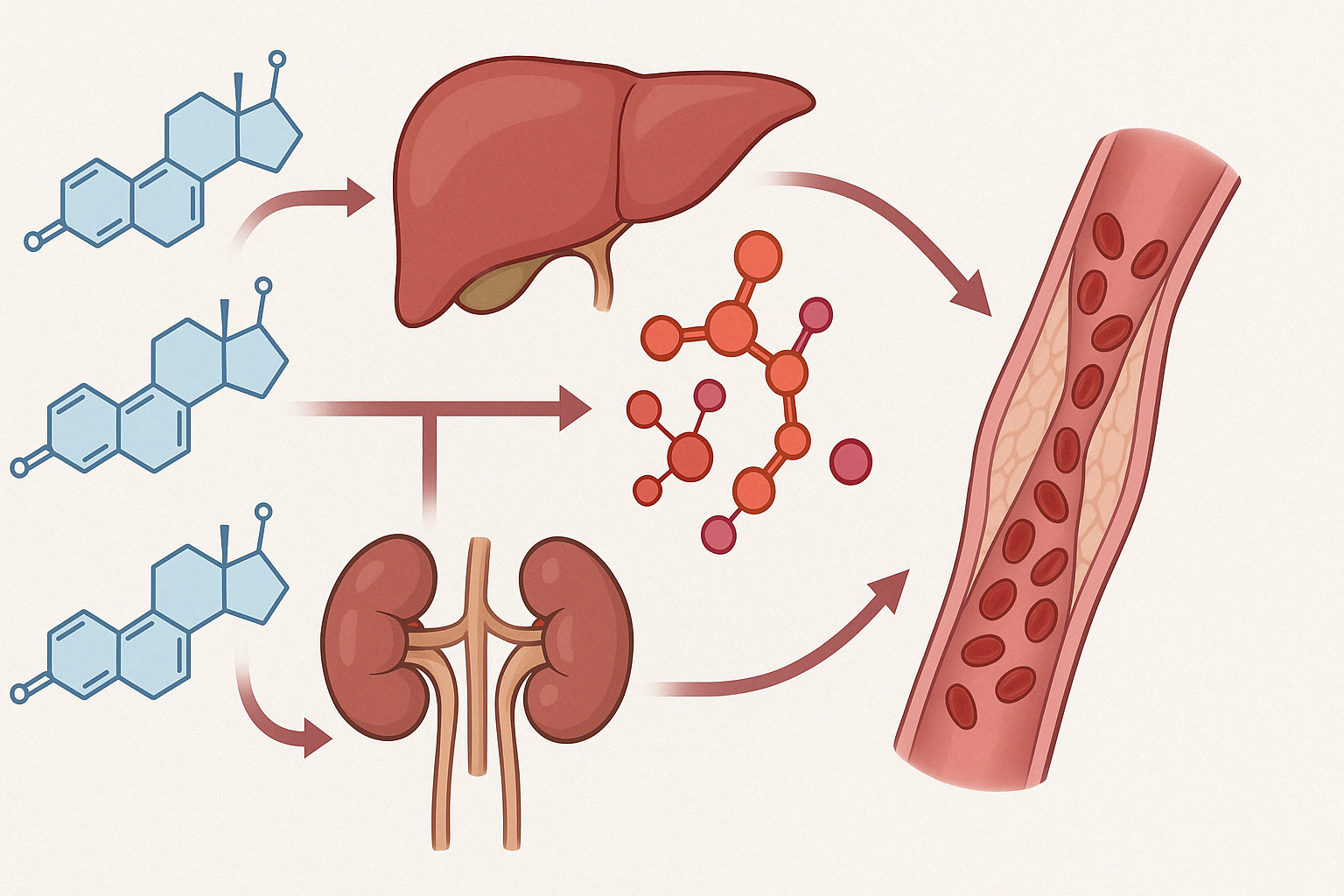
Understanding the physiological mechanisms behind why birth control can cause high blood pressure provides further clarity on the issue. One proposed mechanism involves the upregulation of hepatic production of angiotensinogen by estrogen. Angiotensinogen is a precursor to angiotensin II, a potent vasoconstrictor that can increase blood pressure by narrowing blood vessels and promoting fluid retention.
Estrogen can also increase sympathetic nervous system activity, contributing to higher blood pressure. Meanwhile, progestins—particularly older, androgenic types—may exert additional effects that influence vascular tone and resistance. Newer generation progestins tend to have less impact on blood pressure, which is an important factor to consider when selecting a contraceptive method.
Furthermore, hormonal contraceptives may influence endothelial function. The endothelium, or lining of the blood vessels, plays a crucial role in vascular health. Impairment in endothelial-dependent vasodilation—caused by hormonal alterations—could be another pathway through which oral contraceptives exert hypertensive effects. Thus, the relationship between birth control pills and high blood pressure is mediated through a complex network of hormonal and vascular interactions.
Progestin-Only Pills: A Safer Alternative?
For women concerned about the potential for high blood pressure, progestin-only pills (POPs) are sometimes considered a safer alternative. These pills do not contain estrogen, which is the hormone most commonly implicated in raising blood pressure. As a result, POPs are often recommended for women with contraindications to estrogen, such as those with a history of thromboembolic disorders or migraine with aura.
However, POPs are not entirely without cardiovascular considerations. While generally associated with a lower risk of hypertension, some studies have found that certain types of progestins may still affect blood pressure, albeit to a lesser extent. It’s also worth noting that POPs must be taken at the same time every day to maintain their effectiveness, which may pose adherence challenges for some women.
The choice between combined and progestin-only contraceptives should be made based on a careful evaluation of individual health profiles, preferences, and risk factors. Consulting with a healthcare provider is essential for making an informed decision about whether birth control pills and high blood pressure present a concern in a particular case.
Long-Term Cardiovascular Implications of Hormonal Contraceptive Use
While short-term increases in blood pressure may be modest for most women, the long-term implications of hormonal contraceptive use deserve careful consideration. Sustained elevations in blood pressure, even if mild, can contribute to cumulative cardiovascular risk over time. Chronic hypertension is a well-established risk factor for heart disease, stroke, and kidney failure, all of which can have life-altering consequences.
Moreover, if a woman develops hypertension while using birth control and continues to take the pill without medical supervision, she may unknowingly increase her vulnerability to cardiovascular events. For women with multiple risk factors—such as age over 35, smoking, obesity, and metabolic syndrome—the compounding effects can be particularly concerning. Therefore, answering the question, “Can birth control cause high blood pressure?” has serious implications for long-term health and disease prevention.

Monitoring and Managing Blood Pressure While on Birth Control
One of the most practical steps women can take to minimize cardiovascular risk while on hormonal contraceptives is regular blood pressure monitoring. Baseline blood pressure should be assessed before initiating any hormonal birth control method, and follow-up checks should be conducted periodically thereafter. This proactive approach allows for early detection of changes and timely intervention if needed.
Lifestyle modifications can also help counterbalance any potential increases in blood pressure. These include maintaining a healthy diet low in sodium and rich in potassium, engaging in regular physical activity, avoiding tobacco products, and managing stress. Women who adopt these healthy habits may be better able to tolerate hormonal contraceptives without significant hypertensive effects.
For those who do develop elevated blood pressure while on birth control, options include switching to a different formulation, using non-hormonal methods such as copper IUDs, or treating hypertension with appropriate medication under medical supervision. Personalized care is key to ensuring that birth control pills and high blood pressure do not become an unchecked or unmanaged health issue.
Alternative Contraceptive Options for Women with Hypertension
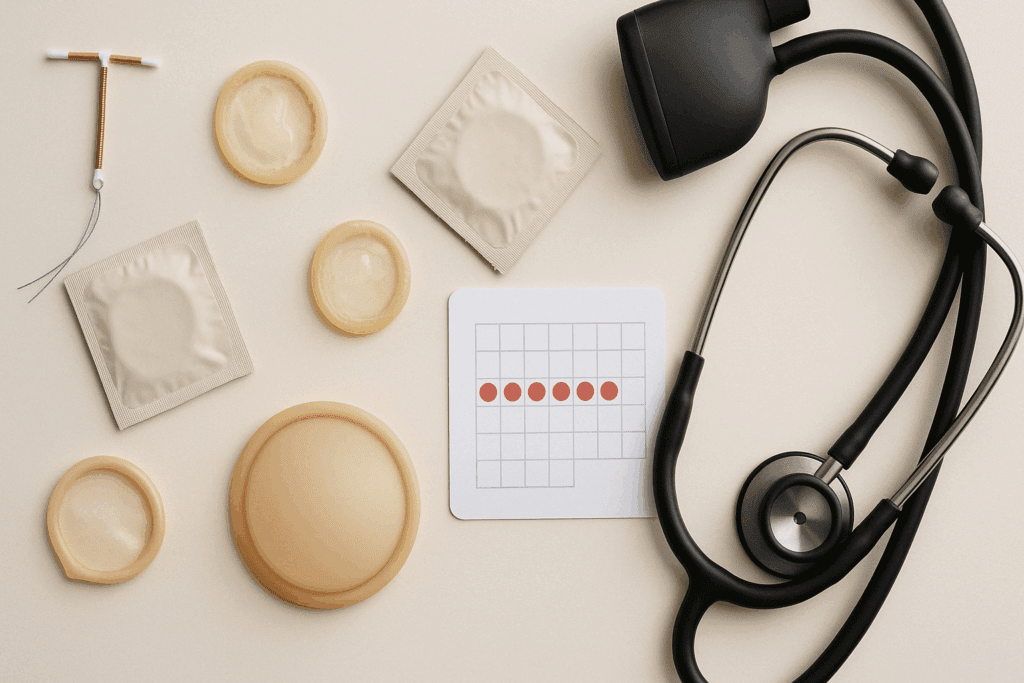
When birth control pills are not a viable option due to high blood pressure or other cardiovascular concerns, a variety of alternative methods are available. Non-hormonal options such as copper intrauterine devices (IUDs), condoms, diaphragms, and fertility awareness methods provide contraception without affecting blood pressure levels. These may be suitable for women seeking effective birth control without the added cardiovascular risk.
Hormonal options with lower systemic impact, such as the levonorgestrel-releasing IUD or the contraceptive implant, may also be considered in consultation with a healthcare provider. These methods release progestin locally rather than systemically and are less likely to influence blood pressure. However, every case is unique, and a comprehensive evaluation is necessary to determine the best approach.
Understanding the spectrum of contraceptive options allows women to make informed decisions in collaboration with their healthcare providers. Whether or not birth control causes high blood pressure may depend on the method chosen, individual susceptibility, and the presence of modifiable or non-modifiable risk factors.
Current Research Directions and Future Considerations
Ongoing research continues to shed light on the nuanced relationship between hormonal contraceptives and cardiovascular health. Studies are increasingly focusing on identifying genetic markers and hormonal pathways that may predispose some women to adverse blood pressure responses. As our understanding of personalized medicine evolves, future contraceptives may be designed to minimize cardiovascular side effects based on an individual’s unique genetic and physiological profile.
In addition, public health efforts aim to improve education around safe contraceptive use and the importance of cardiovascular monitoring. Greater awareness can lead to earlier interventions and better health outcomes for women worldwide. For researchers, clinicians, and patients alike, the intersection between birth control pills and high blood pressure remains a dynamic and essential area of inquiry.
Frequently Asked Questions: Birth Control Pills and High Blood Pressure
1. Are there any early warning signs that birth control is raising my blood pressure?
Yes, although many individuals may not notice symptoms in the early stages, some signs could indicate that birth control is influencing your blood pressure. Subtle symptoms such as frequent headaches, dizziness, fatigue, or a general feeling of being unwell may signal rising blood pressure. Because high blood pressure is often asymptomatic, regular monitoring is essential, particularly if you’re taking hormonal contraceptives. In cases where the link between birth control pills and high blood pressure is present, these symptoms may be the first clue. Consulting your healthcare provider for a blood pressure check after beginning a new contraceptive is a prudent step, even if you feel perfectly fine.
2. Can certain types of birth control reduce the risk of high blood pressure?
Yes, not all hormonal contraceptives carry the same risk. For example, non-estrogen-based options, such as progestin-only pills or hormonal IUDs, may have a less pronounced effect on blood pressure. Some newer birth control formulations use lower doses of hormones or newer-generation progestins that appear to pose fewer cardiovascular risks. If you’re concerned about whether birth control can cause high blood pressure, consider discussing these alternatives with your doctor. Customizing your contraceptive method to your personal health profile can significantly reduce your risk.
3. Why might some women develop high blood pressure on birth control while others do not?
Genetic predisposition, underlying health conditions, lifestyle factors, and even ethnic background can all contribute to individual variability. For instance, women with a family history of hypertension are more likely to see an increase in blood pressure with hormonal contraceptive use. Additionally, factors like stress, diet, and physical activity play a role in how the body responds to these medications. Therefore, the link between birth control pills and high blood pressure is not universal but highly individualized. Understanding your personal risk factors allows you to make more informed choices about contraception.
4. Is it safe to stay on birth control if I already have slightly elevated blood pressure?
It depends on the severity of your blood pressure and the specific type of birth control you’re using. Some women with borderline hypertension may still safely use certain low-dose contraceptives under close medical supervision. However, if your blood pressure readings are consistently elevated, your healthcare provider may recommend switching to non-hormonal methods or progestin-only options. The concern that birth control can cause high blood pressure becomes more significant when hypertension is pre-existing, making regular health checkups even more important in such scenarios.
5. How often should blood pressure be monitored while on birth control?
Ideally, your blood pressure should be measured before starting hormonal contraception and then checked at least every six months thereafter. However, if you have known risk factors such as obesity, smoking, or a family history of cardiovascular disease, more frequent monitoring may be necessary. Since the relationship between birth control pills and high blood pressure can be gradual and subtle, early detection through routine checks helps prevent complications. Home blood pressure monitors offer a convenient way to stay proactive between doctor visits. Keep a log of your readings and share them with your provider to guide ongoing contraceptive decisions.
6. Can lifestyle changes help mitigate the blood pressure effects of birth control?
Absolutely. A heart-healthy lifestyle can make a meaningful difference in reducing the hypertensive effects of birth control. Engaging in regular exercise, following a low-sodium diet, quitting smoking, and managing stress through mindfulness or relaxation techniques are all helpful practices. These habits can lower your baseline blood pressure and improve your overall cardiovascular resilience. If you’re using hormonal contraceptives and wondering whether birth control can cause high blood pressure in your case, these lifestyle changes offer an added layer of protection. They also contribute to better health outcomes across many dimensions.
7. Are younger women immune to the blood pressure effects of birth control?
Not necessarily. Although younger women generally have lower baseline cardiovascular risk, they are not entirely exempt from experiencing a rise in blood pressure due to hormonal contraceptives. Some young women may have undiagnosed conditions such as polycystic ovary syndrome (PCOS) or genetic predispositions that increase susceptibility. Additionally, lifestyle factors like high stress, poor diet, and lack of exercise can amplify the risks. The association between birth control pills and high blood pressure doesn’t discriminate by age, although the degree of risk may vary. Early awareness and proactive monitoring are just as important for younger users.
8. How do emotional stress and mental health influence blood pressure on birth control?
Emotional stress can significantly impact blood pressure by activating the sympathetic nervous system and elevating cortisol levels. When this physiological stress response interacts with hormonal contraceptives, it may create a synergistic effect that increases the likelihood of hypertension. Women who experience chronic stress or anxiety should be particularly mindful of how their birth control regimen may interact with these factors. This connection further complicates the question of whether birth control can cause high blood pressure, as it involves both internal hormonal dynamics and external emotional triggers. Incorporating stress management techniques can be a valuable addition to your preventive health strategy.
9. Is it true that birth control’s effect on blood pressure can linger after discontinuation?
In some cases, yes. Although most women see their blood pressure return to baseline after stopping hormonal contraceptives, others may experience lingering effects—especially if they were already at risk. Long-term use can potentially create vascular changes or reinforce pre-existing hypertensive tendencies that do not resolve immediately. This possibility reinforces the importance of monitoring your blood pressure not only while taking birth control but also after discontinuation. The association between birth control pills and high blood pressure may persist in subtle ways, depending on the individual’s overall health profile and length of use.
10. Are there any promising developments in contraceptive research aimed at reducing cardiovascular risks?
Yes, ongoing research is focused on creating newer hormonal contraceptives that have minimal systemic effects. These include ultra-low-dose pills, transdermal options with improved vascular profiles, and hormone-releasing implants that provide contraception with fewer cardiovascular side effects. Personalized medicine approaches, such as tailoring birth control to a woman’s genetic and metabolic profile, are also on the horizon. These advancements aim to reduce the likelihood that birth control can cause high blood pressure while preserving efficacy and convenience. As innovation progresses, future options may offer safer choices for women with or at risk of hypertension.
Closing Reflections on the Birth Control–Blood Pressure Connection
In summary, the question of whether birth control can cause high blood pressure is both medically valid and nuanced. While not every woman who uses hormonal contraceptives will experience elevated blood pressure, there is sufficient scientific evidence to warrant careful screening, monitoring, and risk assessment. Estrogen-containing birth control pills, in particular, have been shown to affect vascular function and blood pressure regulation through multiple mechanisms. Progestin-only options may offer a safer alternative for some women but are not entirely risk-free.
Importantly, the link between birth control pills and high blood pressure must be viewed within the broader context of individual health profiles and lifestyle factors. Women should not be discouraged from using hormonal contraception when it is appropriate and beneficial, but they should be empowered with the knowledge to make informed decisions. By staying vigilant about cardiovascular health, working closely with healthcare providers, and choosing the most appropriate contraceptive method, women can protect both their reproductive and cardiovascular well-being.
Ultimately, recognizing the potential for birth control to influence blood pressure highlights the importance of personalized medicine. Through ongoing research, patient education, and individualized care, it is possible to balance the benefits of hormonal contraception with a commitment to long-term heart health.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Contraceptive Hormone Use and Cardiovascular Disease
Oral Contraceptive Pills and Hypertension: A Review of Current Evidence and Recommendations
Hormonal Contraception in Women with Hypertension
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.