Introduction: Exploring the Potential of Enzymes in Glucose Management
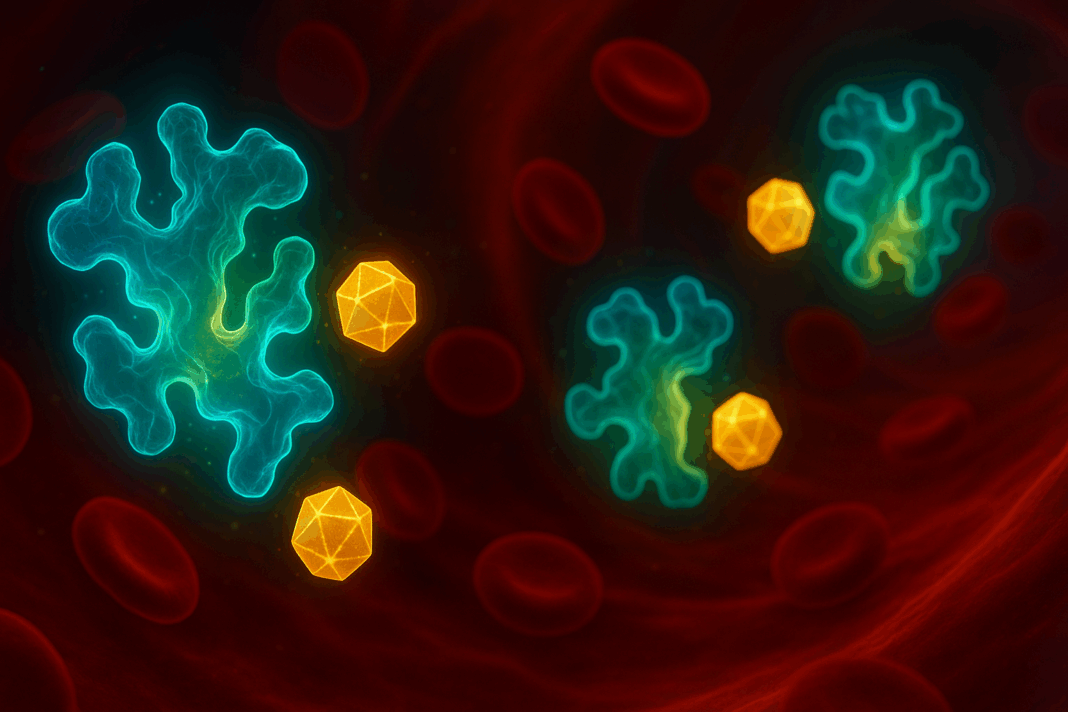
In recent years, the intersection of enzymology and endocrinology has opened a promising frontier in diabetes research. As diabetes continues to affect over 500 million individuals globally, scientists and clinicians are actively exploring innovative, biologically grounded strategies to complement or even enhance traditional treatment modalities. One of the more intriguing developments centers around the question: can enzymes lower glucose levels? This line of inquiry is not merely academic—it holds the potential to revolutionize how we understand and manage diabetes, particularly for those seeking adjunct or alternative therapies that align with the body’s natural biochemical processes.
You may also like: Breakthroughs in Current Diabetes Research: What the Latest Studies Reveal About Treatment and Prevention
The foundation of this interest lies in the biochemical nature of enzymes: proteins that catalyze vital chemical reactions in the body. From digestion to energy metabolism, enzymes are indispensable. In the context of diabetes, specific enzymes have been found to influence glucose metabolism directly, either by enhancing glucose uptake, altering carbohydrate digestion, or modulating insulin signaling pathways. The emergence of these findings has led researchers to investigate the possibility of utilizing what are now commonly referred to as “diabetes enzymes” to create targeted interventions.
This article explores the scientific basis behind enzyme-based therapies for glucose regulation, offering a comprehensive overview of the most recent studies, mechanisms of action, clinical implications, and future directions. Throughout this exploration, we will naturally integrate discussions around the central question—can enzymes lower glucose levels—and evaluate the validity and scope of enzyme therapy within the broader landscape of diabetes care.
Understanding the Role of Enzymes in Human Metabolism
To appreciate how enzymes might contribute to glucose regulation, it’s important first to understand their fundamental roles in human metabolism. Enzymes are biological catalysts that accelerate chemical reactions essential for life. Each enzyme is specific to a particular reaction or group of reactions, functioning with remarkable precision and efficiency.
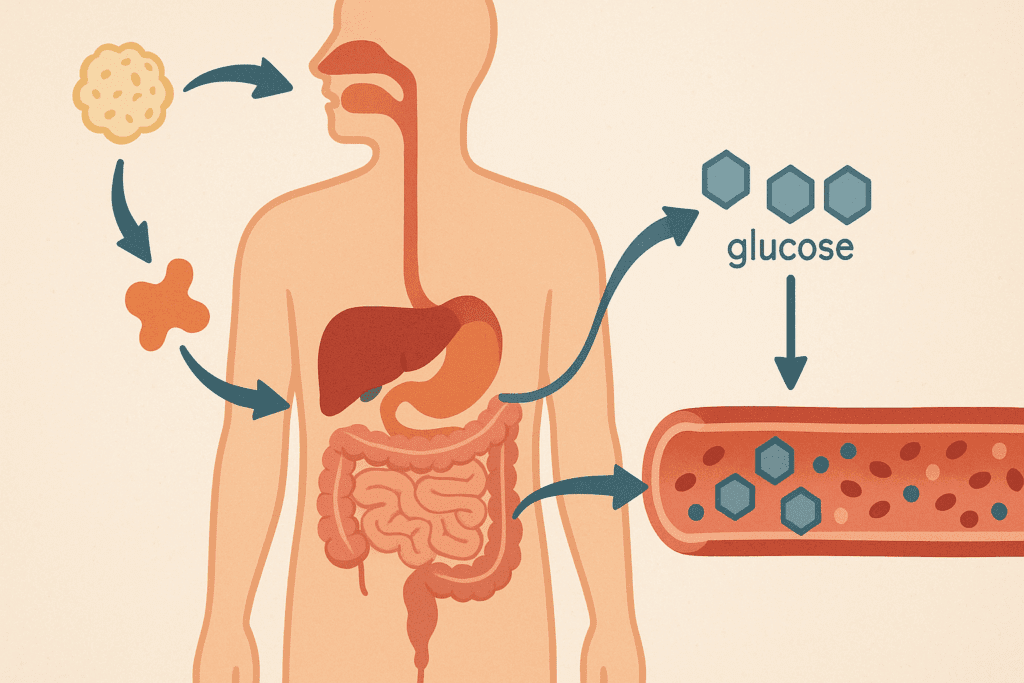
In the context of carbohydrate metabolism, several key enzymes are involved in breaking down complex carbohydrates into simple sugars, primarily glucose, which serves as a critical energy source. Amylase, for example, begins the process by breaking down starch in the mouth and small intestine, while maltase and sucrase further process disaccharides into absorbable monosaccharides. Once in the bloodstream, glucose’s fate is largely determined by enzymes like hexokinase and glucokinase, which facilitate its entry into glycolytic pathways, and by insulin-regulated mechanisms.
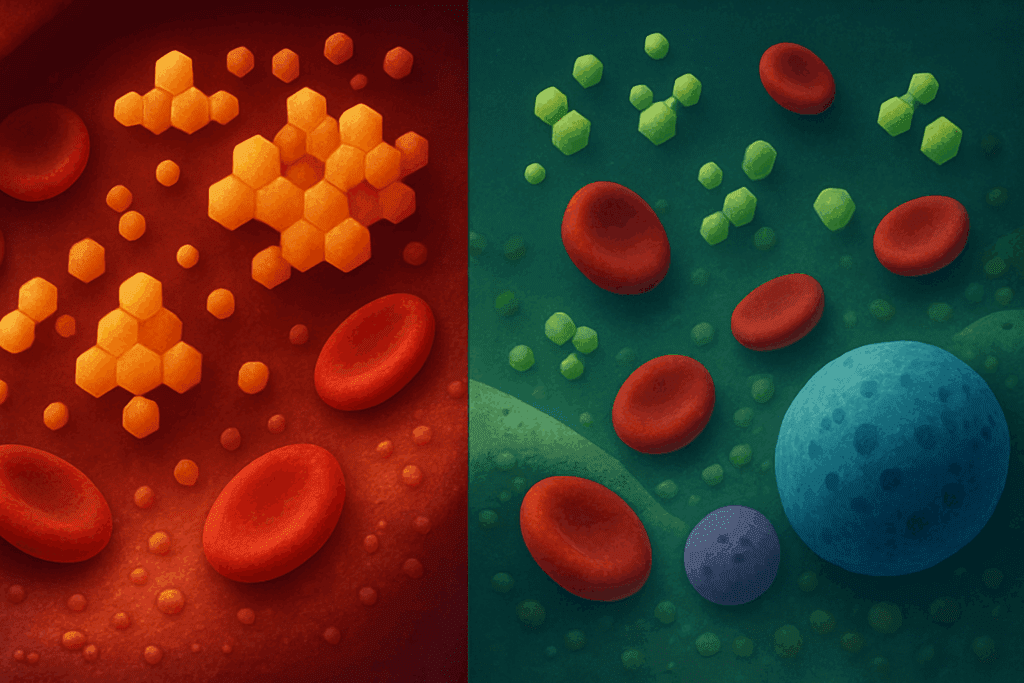
These intricate processes are finely balanced in healthy individuals. However, in diabetes, especially type 2 diabetes, this balance is disrupted due to insulin resistance or impaired insulin secretion. Enzymatic dysfunction may either exacerbate or help compensate for these disruptions, depending on how specific enzymes behave. Understanding and potentially modifying these enzyme pathways opens a door to novel therapies that operate at a molecular level, potentially improving outcomes beyond what standard pharmacological interventions offer.
The Science Behind Diabetes Enzymes and Glucose Regulation
Emerging research has identified a class of enzymes whose modulation appears to significantly influence blood glucose levels. These so-called “diabetes enzymes” have gained attention due to their ability to target specific stages in the glucose metabolic cycle, including absorption, digestion, uptake, and storage.
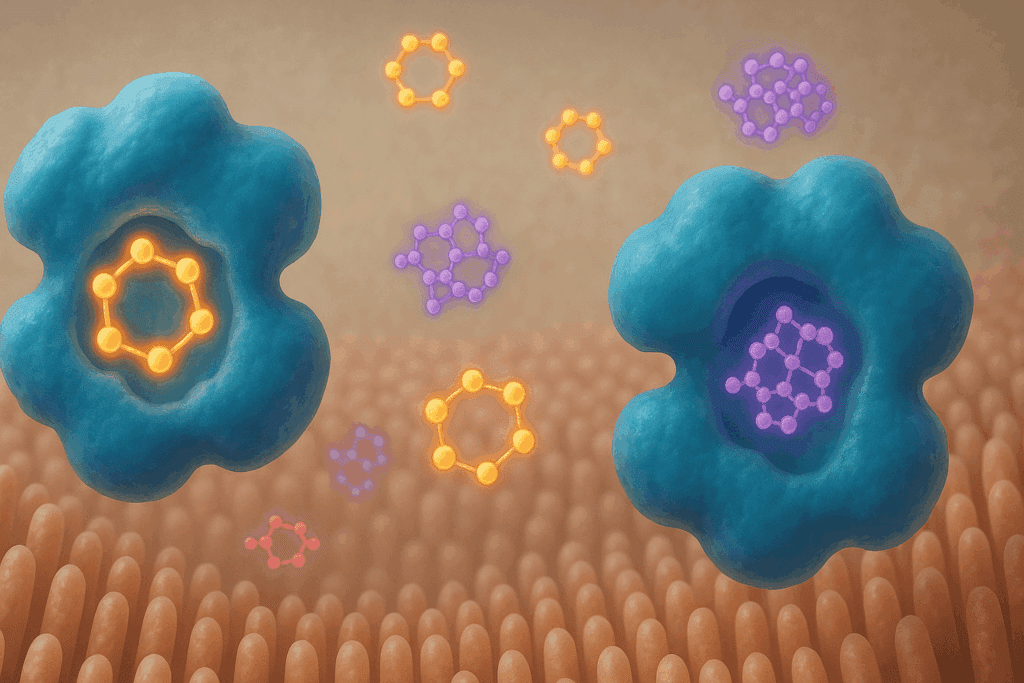
One of the most studied groups in this context is the family of alpha-glucosidase enzymes. Located in the intestinal brush border, alpha-glucosidase facilitates the final step of carbohydrate digestion, converting oligosaccharides into glucose. Inhibiting this enzyme slows carbohydrate absorption and leads to a more gradual postprandial rise in blood glucose. This principle underpins the therapeutic action of drugs like acarbose and miglitol, which are synthetic alpha-glucosidase inhibitors used to manage type 2 diabetes.
Another enzyme of interest is dipeptidyl peptidase-4 (DPP-4), which breaks down incretin hormones like GLP-1. Incretins stimulate insulin secretion in response to meals, and by inhibiting DPP-4, these hormones remain active longer, enhancing insulin response and thereby reducing blood glucose levels. DPP-4 inhibitors are now widely used as part of standard diabetes management protocols.
Recent advances have also highlighted enzymes such as AMPK (AMP-activated protein kinase), which, while not traditionally categorized under digestive enzymes, plays a critical role in cellular energy homeostasis. Activating AMPK can increase glucose uptake in muscle and fat tissue independently of insulin, which is especially valuable in insulin-resistant states.
These discoveries indicate that targeting enzymes may offer not only symptom relief but also deeper metabolic correction, positioning enzyme-based therapies as more than just auxiliary tools—they could become central components of precision medicine for diabetes.
Can Enzymes Lower Glucose Levels? Evidence from Clinical and Preclinical Studies
The question of whether enzymes can lower glucose levels has transitioned from theoretical speculation to evidence-based inquiry. Both animal models and human clinical trials have begun to affirm that enzyme modulation can influence glycemic outcomes significantly.
In preclinical studies, rodents treated with natural enzyme inhibitors derived from plant sources—such as mulberry extract or salacia oblonga—showed reduced postprandial glucose spikes and improved insulin sensitivity. These findings have spurred interest in botanical supplements that naturally contain diabetes enzyme modulators. While these studies are preliminary, they lay a foundation for future clinical applications.
Human trials have further solidified the potential of enzyme-based approaches. A landmark study published in Diabetes Care examined the effects of alpha-glucosidase inhibitors on HbA1c levels in patients with type 2 diabetes. The results revealed a consistent reduction in HbA1c by approximately 0.5–0.8%, along with improved postprandial glucose profiles. Similarly, DPP-4 inhibitors such as sitagliptin have been shown to reduce HbA1c levels by comparable margins with relatively few side effects, particularly in patients intolerant to metformin.
Other research efforts are exploring enzyme therapy in combination with lifestyle interventions. For instance, studies that paired alpha-glucosidase inhibitors with low-glycemic diets found synergistic effects on glycemic control, suggesting that enzyme therapies may be most effective when used as part of a holistic treatment plan. These findings collectively support the hypothesis that enzymes can lower glucose levels and do so in a clinically meaningful way.

Plant-Based Enzyme Inhibitors: A Natural Approach to Diabetes Management
An exciting subfield of enzyme-based diabetes therapy involves naturally occurring enzyme inhibitors found in plants. Many traditional herbal medicines have long been used to treat symptoms of diabetes, and modern research is beginning to uncover the enzymatic mechanisms behind these effects.
For example, flavonoids and polyphenols found in foods like green tea, cinnamon, and bitter melon have demonstrated alpha-glucosidase and DPP-4 inhibitory activity in vitro. This enzymatic modulation may explain the observed reductions in post-meal glucose spikes when these foods are consumed regularly. Furthermore, compounds like berberine have shown AMPK-activating properties, mirroring the effects of pharmaceutical agents like metformin.
Clinical trials evaluating these natural compounds remain limited in scope but are gradually gaining momentum. Small-scale studies on bitter melon supplements, for instance, have reported improved glucose tolerance and reductions in fasting blood sugar. While more robust randomized controlled trials are needed, the initial findings are promising and suggest a potential role for enzyme-focused nutritional strategies in diabetes care.
Importantly, plant-based enzyme inhibitors offer advantages in terms of safety, tolerability, and accessibility. Many are available as dietary supplements and may serve as adjunct therapies for individuals seeking to reduce dependence on prescription medications. However, caution is warranted, as the variability in supplement potency and lack of regulation require oversight and guidance from healthcare professionals.
Enzyme Therapy and Its Potential Role in Personalized Diabetes Treatment
As the field of diabetes care shifts toward personalization and precision medicine, enzyme-based therapies offer a uniquely adaptable platform. Because enzymes are highly specific in their actions, therapies targeting them can be fine-tuned to address individual metabolic profiles, dietary patterns, and genetic predispositions.
For instance, individuals with higher postprandial glucose spikes may benefit more from alpha-glucosidase inhibitors, while those with impaired insulin secretion might respond better to DPP-4 inhibitors or GLP-1-based strategies. Similarly, patients with high insulin resistance could find improved outcomes with AMPK activators. This specificity not only increases therapeutic efficacy but may also reduce the incidence of adverse effects, as interventions are more closely aligned with the individual’s physiological needs.
Moreover, enzyme therapy can potentially be integrated with genomic and metabolomic data to identify biomarkers that predict response. This level of customization marks a significant evolution from the one-size-fits-all approach that has dominated diabetes care for decades. As more is learned about the interplay between enzymes and systemic glucose regulation, the ability to tailor treatment plans will likely expand, offering new hope for individuals struggling with glycemic control despite existing therapies.
Limitations, Safety Concerns, and the Need for Continued Research
Despite the exciting potential of enzyme-based approaches, several limitations must be acknowledged. First and foremost is the variability in individual response, which can be influenced by genetic factors, gut microbiota composition, and coexisting medical conditions. This variability underscores the importance of clinical trials that include diverse populations to better understand who stands to benefit most.
There are also safety considerations, particularly when enzyme inhibitors are used long-term. Gastrointestinal side effects are common with alpha-glucosidase inhibitors, including bloating, diarrhea, and flatulence due to undigested carbohydrates fermenting in the colon. DPP-4 inhibitors, while generally well-tolerated, have raised concerns about potential links to pancreatitis and joint pain, although causality remains unconfirmed.
Furthermore, natural enzyme inhibitors, while appealing, often suffer from inconsistencies in formulation and lack of regulatory oversight. Standardizing extracts, identifying active compounds, and determining optimal dosages are essential steps before these can be recommended widely. Until these issues are addressed through rigorous research, enzyme therapies should be considered complementary rather than primary interventions.
Lastly, more long-term data are needed to assess the impact of enzyme therapies on complications associated with diabetes, such as cardiovascular disease, neuropathy, and nephropathy. While glycemic control is a critical target, the ultimate goal of therapy is to reduce morbidity and improve quality of life—metrics that require years of follow-up to evaluate fully.
Frequently Asked Questions: Enzyme-Based Therapies and Blood Sugar Control
1. How do enzyme-based therapies differ from conventional diabetes medications?
Enzyme-based therapies represent a fundamentally different approach compared to conventional diabetes medications. Rather than simply increasing insulin production or enhancing insulin sensitivity, these therapies aim to influence the biochemical pathways that regulate how glucose is metabolized, digested, and absorbed. By targeting specific enzymes involved in carbohydrate breakdown or glucose transport, they can help manage blood sugar levels more subtly and physiologically. For instance, instead of flooding the body with exogenous insulin, a therapy targeting a diabetes enzyme could help extend the life of naturally produced insulin or slow glucose absorption. This raises the question—can enzymes lower glucose levels with fewer side effects? In some cases, enzyme-based strategies may offer a gentler, more targeted alternative, especially for patients experiencing gastrointestinal distress or hypoglycemia from standard treatments.
2. Are there lifestyle factors that affect how well diabetes enzymes work?
Yes, lifestyle choices can significantly impact the efficacy of diabetes enzyme activity. Diet plays a particularly crucial role, as high-fat or high-glycemic meals can overwhelm enzyme-inhibiting therapies by rapidly increasing postprandial glucose. Conversely, low-carbohydrate diets or meals high in fiber can enhance the effectiveness of alpha-glucosidase inhibitors by slowing digestion and reducing glucose surges. Exercise also plays a role by influencing enzymes like AMPK, which improves glucose uptake in muscles independent of insulin. When asking whether can enzymes lower glucose levels effectively, it’s important to consider how sleep, stress, and even hydration status might modulate enzymatic function. For optimal results, enzyme therapies should be integrated into a holistic lifestyle plan.
3. What emerging enzyme targets are researchers exploring beyond the commonly known ones?
In addition to well-established enzymes like DPP-4 and alpha-glucosidase, researchers are investigating newer targets such as protein tyrosine phosphatase 1B (PTP1B), which negatively regulates insulin signaling. Inhibiting PTP1B has shown promise in improving insulin sensitivity and lowering glucose levels in animal models. Another exciting target is fructokinase, an enzyme involved in hepatic glucose metabolism; altering its activity may reduce the accumulation of liver fat and improve glucose control. Some studies are also looking at sirtuins, a family of enzymes associated with cellular aging and metabolic regulation. These cutting-edge developments add depth to the inquiry: can enzymes lower glucose levels through entirely novel biochemical pathways? If proven effective in humans, they could pave the way for future therapies that extend beyond traditional glucose management strategies.
4. How might enzyme therapies benefit people with prediabetes or metabolic syndrome?
While much of the research on diabetes enzymes focuses on patients with established type 2 diabetes, those with prediabetes or metabolic syndrome could also see significant benefits. In these early stages, insulin resistance and elevated post-meal glucose levels are often present, but beta-cell function is typically still intact. Enzyme therapies could help delay or even prevent progression by targeting the root metabolic dysfunction before full-blown diabetes develops. For example, slowing carbohydrate absorption with an alpha-glucosidase inhibitor might reduce the glycemic burden on pancreatic beta cells. When considering if can enzymes lower glucose levels in prediabetes, the evidence suggests they can indeed play a preventive role when introduced early alongside lifestyle interventions.
5. Can enzymes that lower glucose levels also impact weight loss or appetite?
There is growing interest in how diabetes enzyme modulation may influence appetite and weight. Some enzyme therapies, particularly those that prolong incretin activity (such as DPP-4 inhibitors), can enhance satiety and reduce calorie intake. Additionally, enzymes like AMPK are deeply involved in energy regulation and fat oxidation, which means that activating them may help promote fat loss and curb excessive appetite. While enzyme therapies aren’t a replacement for structured weight management programs, they may complement these efforts by regulating the hormonal signals involved in hunger and metabolism. The interplay between blood sugar and weight makes it even more relevant to explore whether can enzymes lower glucose levels while offering auxiliary metabolic benefits.
6. Are there risks of using enzyme-based supplements without medical supervision?
Yes, there are potential risks to using enzyme-based supplements without professional guidance. Many over-the-counter products claim to modulate a diabetes enzyme, but these supplements can vary widely in potency, purity, and bioavailability. In some cases, they may interact with prescription medications or exacerbate underlying health conditions, such as kidney disease or gastrointestinal disorders. Additionally, overuse of enzyme inhibitors can lead to malabsorption issues, especially when they interfere with nutrient breakdown. The question of can enzymes lower glucose levels safely hinges on responsible use—under the supervision of a healthcare provider who can tailor recommendations to individual health profiles and monitor for adverse effects.
7. How do gut microbiota influence enzyme therapy outcomes in diabetes?
Emerging research suggests that gut microbiota can modulate the effectiveness of diabetes enzyme therapies. Specific bacterial strains can influence how certain enzymes behave, either enhancing or diminishing their function. For example, the production of short-chain fatty acids by gut bacteria has been shown to activate AMPK, contributing to improved glucose regulation. Moreover, enzyme inhibitors that act in the gut—like alpha-glucosidase blockers—may alter the microbial environment, with unknown long-term effects. As scientists investigate can enzymes lower glucose levels sustainably, understanding the gut-enzyme connection may hold the key to optimizing outcomes and minimizing unintended consequences.
8. Could enzyme therapies be used alongside insulin for better control in type 1 diabetes?
While enzyme-based treatments have largely been studied in the context of type 2 diabetes, there’s growing curiosity about their role in type 1 diabetes as adjunct therapies. Since insulin therapy is non-negotiable for type 1 patients, the use of enzymes would be aimed at fine-tuning postprandial control and possibly reducing the total insulin burden. For example, alpha-glucosidase inhibitors might slow glucose absorption, allowing for more predictable insulin dosing. Similarly, AMPK activators could enhance glucose uptake in peripheral tissues, potentially offering tighter control. The notion that can enzymes lower glucose levels even in insulin-dependent diabetes opens up possibilities for hybrid treatment models that merge metabolic and hormonal strategies.
9. What role do genetics play in determining enzyme activity related to glucose control?
Genetic variation can have a profound effect on how diabetes enzymes function. Single nucleotide polymorphisms (SNPs) in genes that encode key metabolic enzymes may influence how individuals respond to both dietary carbohydrates and pharmaceutical treatments. For instance, variations in the gene for DPP-4 can affect the rate at which incretins are broken down, altering the efficacy of DPP-4 inhibitors. Similarly, mutations in AMPK subunits may blunt or exaggerate their glucose-lowering effects. These differences highlight the need for personalized medicine approaches when determining whether can enzymes lower glucose levels effectively in a given individual. Genetic screening could one day guide clinicians in selecting the most appropriate enzyme-based therapies.
10. What is the future outlook for enzyme therapy in diabetes management?
The future of enzyme therapy in diabetes is both promising and dynamic. With growing interest in natural and precision-based interventions, the therapeutic landscape is expanding to include biologics, peptide-based enzyme modulators, and even gene-editing strategies that regulate enzyme expression. Artificial intelligence and computational biology are accelerating the discovery of novel diabetes enzyme targets, allowing for more predictive and personalized interventions. Additionally, wearable biosensors could one day monitor enzyme activity in real-time, providing immediate feedback on glucose dynamics and treatment effectiveness. As the question—can enzymes lower glucose levels—continues to be explored, it becomes increasingly clear that enzyme modulation is not a fringe idea but a central component of the next generation of diabetes care.
Conclusion: The Future of Diabetes Enzyme Therapies and the Path Forward
The question—can enzymes lower glucose levels—has, over the past decade, transformed from speculative theory to a medically validated concept. Backed by a growing body of research, enzyme-based therapies now occupy a promising niche in the expanding arsenal against diabetes. Whether through pharmaceutical inhibitors, natural plant compounds, or emerging biologics, the modulation of key diabetes enzymes offers a pathway to more precise, effective, and potentially safer treatment strategies.
What makes this approach particularly compelling is its alignment with the principles of personalized medicine. Enzymes operate within finely tuned biological networks, and by targeting them with surgical precision, clinicians can craft interventions that fit the unique metabolic makeup of each patient. This is a profound shift from traditional strategies that often rely on broad-spectrum pharmacology with generalized outcomes.
Nonetheless, caution and scientific rigor remain paramount. While the ability of enzymes to lower glucose levels is increasingly well-supported, the optimal methods, combinations, and long-term implications of such therapies require further exploration. Collaboration between endocrinologists, molecular biologists, pharmacologists, and nutritionists will be essential in moving this field forward.
As we continue to uncover the biochemical subtleties of glucose regulation, one thing is clear: enzyme-based therapies hold real, research-backed promise. Their integration into modern diabetes care may not only enhance glycemic control but also usher in a new era of treatment rooted in the body’s natural mechanisms—one that is as elegant as it is effective.
glucose metabolism support, natural blood sugar control, enzyme therapy for diabetes, postprandial glucose management, glycemic response regulation, metabolic health strategies, non-insulin diabetes treatments, functional foods for diabetes, glucose absorption inhibitors, incretin hormone support, blood sugar management research, personalized diabetes care, plant-based diabetes solutions, carbohydrate digestion regulation, AMPK activation and glucose, insulin resistance therapies, gut health and diabetes, enzyme activity and metabolism, innovative diabetes treatments, precision medicine for diabetes
Further Reading:
A review on potential anti-diabetic mechanisms of chitosan and its derivatives
Type II diabetes mellitus: a review on recent drug based therapeutics
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While MedNewsPedia strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. MedNewsPedia, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of MedNewsPedia.